Articles concerning Kawasaki disease and COVID-19
This is an outrigger page from a particular part of the main page cv19/#kdarticles
. The primary purpose of this page is to link to 15 articles about
Kawasaki disease (Kawasaki syndrome) and COVID-19 which do NOT mention
this crucial research article which enables us to understand its cause,
no matter whether it is triggered by COVID-19 or any other condition:
extremely low vitamin D levels:
I found another 3 such articles on 2020-06-11: ../#more-KD-articles-1 and wrote to the authors of all of them. A copy of my message is below: #msg .
Once you have read this article, and looked at the research I present on these pages:
I believe that you will understand that vitamin D deficiency is the
biggest easy-to-correct factor causing severe and deadly outcomes with
COVID-19 in general, and with Kawasaki disease (whatever the trigger)
for babies, children and adolescents.
If and when some such articles appear which do cite Stefano Stagi et al. 2016, I will add them to a second list here.
I found these articles entirely with Google Scholar. I did not
chase references or look for web pages such a of health authorities,
blogs etc.
Robin Whittle rw@firstpr.com.au
. 2020-05-30 Last update 2020-06-11 11:00 UTC
To the main COVID-19 page of this site: http://aminotheory.com/cv19/
Be sure to read the Disclaimer!
List of articles concerning Kawasaki disease AND COVID-19 which do NOT cite Stefano Stagi et al. 2016
I may have missed one or two, but as
far as I can tell, this is all the articles listed on Google Scholar
concerning COVID-19 and Kawasaki disease, at the end of
2020-05-29. None of the articles mention Stefano Stagi et al
2016. Nor do they mention vitamin D, the word "vitamin" or
anything concerning nutrition.
There's no particular order. The
first block of articles are those I added on 2020-05-30.
We
describe the case of a 6-month-old infant admitted and diagnosed with
classic Kawasaki disease (KD), who also screened positive for COVID-19
in the setting of fever and minimal respiratory symptoms.
The cause of KD remains unknown, despite several decades of investigation.
Some evidence suggests an infectious trigger, with winter-spring
seasonality of the disease, and wave-like spread of Japanese epidemics
of KD. Various studies have described an association between
viral respiratory infections and KD, ranging from 9% to as high as 42%
of patients with KD testing positive for a respiratory viral infection
in the 30-days leading up to diagnosis of KD.
With
regards to her COVID-19 infection, our patient’s clinical course and
presentation were mild. Throughout her hospitalization, she did
not have any notable respiratory symptoms and repeat chest x-ray was
not obtained.
|
Upper extremity erythema and edema. Maculopapular rash. Elevated C-reactive protein (CRP
W) 13.3mg/dl. (Normal range to 0.3.) Normal platelets. Erythrocyte sedimentation rate [
W]
118mm/hr (ref range up to ~10mm/hr) indicates inflammation and that the
blood is in a coagulative state. No mention of lasting harm, though
they will continue to monitor her heart.
Kawasaki disease is a rare acute paediatric vasculitis, with coronary artery aneurysms
as its main complication. The diagnosis is based on the presence
of persistent fever, exanthema, lymphadenopathy, conjunctival
injection, and changes to the mucosae and extremities. Verdoni
and colleagues describe ten cases (seven boys, three girls; aged 7·5
years [SD 3·5]) of a Kawasaki-like disease occurring in Bergamo, Italy,
at the peak of the pandemic in the country (Feb 18 to April 20, 2020),
a monthly incidence some 30-fold higher than observed for Kawasaki disease across the previous 5 years.
Anecdotally, clinicians across Europe have identified clusters of
similar cases. In the UK, paediatricians have identified a small group
of children presenting with shock and
a multisystem inflammation to critical care units, some of whom have
coronary artery aneurysms, and a further group of less severely
ill children with a Kawasaki-like disease, who respond to a variety of
immunomodulatory treatments, including intravenous immunoglobulin,
corticosteroids, and biologics such as infliximab and anakinra
(Whittaker E, unpublished). Long-term echocardiogram data on coronary artery aneurysms are pending.
In response to this cluster in London, UK, we notified the National
Health Service of the emergence of an unusual disorder, and an alert
was issued on April 25. On the basis of the review of clinical
and laboratory features, a case definition of the syndrome we have
provisionally called paediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 (PIMS-TS) was formulated by experts in the UK and published by the Royal College of Paediatrics and Child Health.
. . . the mechanism for the Kawasaki-like disease described here and PIMS-TS might represent post-infectious inflammatory syndrome, which might be antibody or immune-complex mediated, particularly because in this Italian cohort there was little evidence of viral replication.
|
As best I understand this letter, the authors are concerned that with
the focus on COVID-19 patients and the difficulty of bringing children
to hospital, that children suffering from Kawasaki disease may not be
diagnosed in a timely manner. As far as I know, they are not
suggesting that COVID-19 might be triggering Kawasaki disease - but
perhaps that is assumed knowledge.
Without timely treatment, Coronary Arterial Aneurisms could occur in up to 25% of children with Kawasaki disease.
|
Several reports have recently highlighted a spike in the incidence of
KD in the COVID-19-positive pediatric population. These
presentations of KD may occur weeks after the diagnosis of COVID-19 and
possibly once the patient has recovered from the virus.
The etiology of KD is unknown. However, there have been theories related to infectious triggers.
|
On April 26, an alert was sent to general practitioners in London advising them of rising numbers of cases of a multisystem inflammatory state in children with overlapping features of toxic shock syndrome (TSS) and atypical KD. These cases were subsequently described in a correspondence in the Lancet on May 7, 2020, which detailed 8 children with critical illness characterized by severe inflammation, though not all had confirmed COVID-19 infection or exposure.
In Bergamo, Italy, KD was diagnosed in 20 children over a short period,
roughly equivalent to the total number of cases that region sees over 3
years. The French health minister reported that around 15
children were hospitalized in Paris hospitals with symptoms of
KD. On May 4, 2020, the New York City health department issued a
health alert describing 15 cases of
a multi-system inflammatory syndrome with features of KD or TSS.
Since then, media reports have increased dramatically in the New York
City area and now include Detroit and Chicago . . .
|
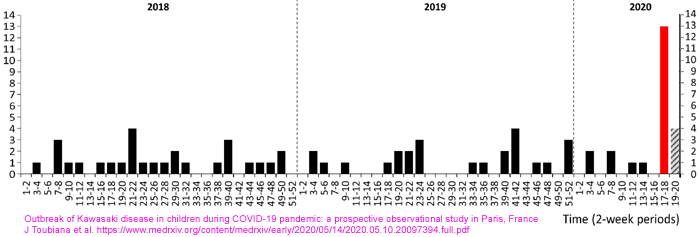
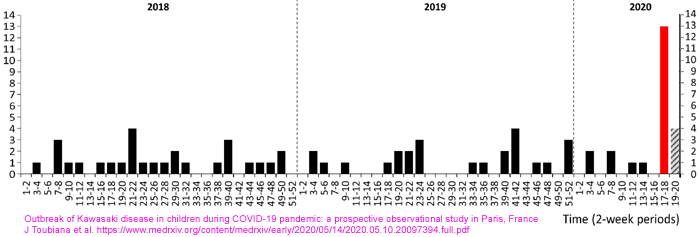
A total of 17 children were admitted for KD over an 11-day period, in
contrast with a mean of 1.0 case per 2-week period over 2018-2019.
Their median age was 7.5 (range, 3.7-16.6) years, and 59% of patients
originated from sub-Saharan Africa or Caribbean islands. Eleven patients presented with KD shock syndrome (KDSS) requiring intensive care support,
and 12 had myocarditis. All children had marked gastrointestinal
symptoms at the early stage of illness and high levels of inflammatory
markers. Fourteen patients (82%) had evidence of recent
SARS-CoV-2 infection (positive RT-PCR 7/17, positive IgG antibody
detection 14/16).
|
Everyone knows that dark skinned people living in Europe are likely to
have low vitamin D levels, unless they take supplements. The
clinicians ran a battery of lab tests, but 25OHD was not one of
them.
This proves beyond reasonable doubt that the clinicians did not
consider vitamin D deficiency as a possible cause, or even association,
with Kawasaki disease.
Kawasaki disease (KD) is the most common primary vasculitis in
childhood, affecting predominantly medium and small-sized
arteries. KD annual incidence is the highest in Japan, with more
than 300 per 100,000 children < 4 years of age, compared to 25 per
100,000 children < 5 years of age in North America. One of the
most severe complications of KD is coronary artery aneurysm. KD shock syndrome (KDSS) is a rare form of KD, frequently associated with myocarditis and requiring critical care support
during the acute phase of illness. Although the aetiology of KD
remains unclear, a role of a viral trigger on some genetically
predisposed children has been hypothesised . . .
|
All patients had high inflammatory parameters, including leukocytosis with a predominance of neutrophils, and high levels of C-reactive protein (CRP), procalcitonin (PCT), and serum interleukin-6. Anaemia was common with a median haemoglobin level reaching 8.1 (range, 5.3-12.2) g/dL. All patients had hyponatraemia (<135 mmol/L), and hypoalbuminaemia (<32 g/L) except one patient with mild KD.
|
I was surprised by the low sodium, but I am not a doctor. I wrote on
../cv19/ about excessive salt intake worsening immune system dysregulation, based on articles such as
Where there is sodium there may be sepsis PMC6735289 .
All but one of our patients had no suggestive symptoms of acute
Covid-19 disease and most had positive serum IgG responses, suggesting
that the development of KD in these patients is more likely to be the
result of a post-viral immunological reaction.
|
The observation of a higher rate of patients originating from sub-Saharan Africa and the Caribbean islands
is consistent with recent findings reported by Riphagen et al.,
suggesting either adverse social and living conditions or genetic
susceptibility. KD is rarely reported in sub-Saharan Africa, but it may be more common than previously thought.
|
These clinicians seem never to have heard of vitamin D deficiency in
dark-skinned people who move to less sunny, urban, environments such as
Paris! The parents' origins were:
- 59% sub-Saharan Africa/Caribbean islands.
- 59% Asia. [Vague - Japan, China?? Maybe India or Pakistan.]
- 12% Europe.
5-year-old
boy from a COVID-19 hotspot area in Kerala state of India who presented
in late April 2020 with acute febrile illness with abdominal pain and
loose stools followed by shock. On examination, child had bulbar
conjunctivitis and extremity edema.
Inflammatory
parameters were high (CRP- 120 mg/l, ESR 70 mm/hr, Ferritin 600 mg/dl)
and serum creatinine (1.35 mg/dl) and liver enzymes were elevated
(AST-85 U/L, ALT-60 U/L). Serum Albumin was low (2.1 gm/dl) and hyponatremia (124 mEq/L) was also present.
|
While
the etiology of Kawasaki Disease has been considered elusive for some
time, there is substantial data pointing to a likely viral
etiology. Many have hypothesized that some children may be genetically predisposed to a more robust inflammatory response to specific viruses. Once exposed to the specific virus, children then mount this exaggerated inflammatory response which clinically manifests as what is now defined to be Kawasaki Disease.
Viruses
associated with Kawasaki Disease include Influenza, Enterovirus,
Adenovirus, Parvovirus, Rhovirus, RSV, Varicella, Epstein-Barr,
measles, and dengue. Association with previous coronavirus has
also been demonstrated. With this in mind why should Kawasaki Disease
with Covid-19 come as a surprise?
Additionally, hyperinflammatory response to Covid-19 has been reported at length in adults.
Elevated inflammatory and reactive markers including C-reactive
protein, procalcitonin, ferritin, and D-dimer amongst others. In
fact, these have prognostic value as more ill Covid-19 patients have
higher values. In adults. accumulating evidence suggests that a
subgroup of patients with severe COVID-19 have a "cytokine storm syndrome" in which a cascade of activated cytokines leads to harmful auto-amplifying hyperinflammatory cytokine production.
Adult patients with worse illness and greater evidence of inflammation
also had a higher incidence of cardiac findings such as troponin leak
and ventricular dysfunction. Thus, these findings also may simply
be inherent to more severe Covid-19 secondary to overall inflammatory
response. This has been noted in viremia from other agents as well,
particularly in the form of myocarditis.
|
South
Thames Retrieval Service in London, UK, provides paediatric intensive
care support and retrieval to 2 million children in South East England. During a period of 10 days in mid-April, 2020, we noted an unprecedented cluster of eight children with hyperinflammatory shock, showing features similar to atypical Kawasaki disease, Kawasaki disease shock syndrome, or toxic shock syndrome (typical number is one or two children per week).
|
So every year, from a population of 2,000,000 children, there are normally 75 or so cases of Kawasaki disease.
None of this would be happening if the children had reasonable vitamin D intakes. The official UK recommendations
../#NHS-advice
are too low for adults - and for children with adult-sized bodies - but
they are probably fine for infants and younger children.
Why haven't the doctors thought of this?
Clinical presentations were similar, with unrelenting fever (38–40°C),
variable rash, conjunctivitis, peripheral oedema, and generalised
extremity pain with significant gastrointestinal symptoms.
Most of the children had no significant respiratory involvement, although seven of the children required mechanical ventilation for cardiovascular stabilisation.
One child developed arrhythmia with refractory shock, requiring extracorporeal life support, and died from a large cerebrovascular infarct.
|
A 14 year old Afro-Caribbean boy (95kg) died of stroke. He
was killed by his own immune system, triggered by a virus which would
not cause such trouble if he was properly nourished so that his immune
system was stronger and better regulated.
With sufficient micronutrients, including especially vitamin D (and he
would probably need 5000 to 8000IU a day to be replete, with that
weight) he would have been much healthier, and would never have
succumbed to Kawasaki disease.
Why is supplementation so difficult compared to these ICU heroics and
death? Why to the doctors not mention vitamin D? There are
surely reasons, but none of them are good.
This is a detailed case report concerning three boys 5, 10 (asthma) and
13 (hypothyroid) one girl 12 in New York. All survived.
Common laboratory findings among hospitalized [adult]
patients with RT-PCR positive SARS-CoV-2 infection include lymphopenia,
elevated lactate dehydrogenase levels, elevated inflammatory markers
(ferritin, C-reactive protein, and erythrocyte sedimentation rate),
elevated procalcitonin and elevated D-dimer. The same laboratory
findings were seen in these four children with COVID-19 post-infectious
cytokine release syndrome.
Additionally, all four children had an exaggerated cytokine storm with a profoundly elevated IL-6 and elevated IL-8 and TNF-α. Elevations in these cytokines can lead to increased vascular hyperpermeability, multiorgan failure and eventually fatality if the cytokine concentrations remain unabated over time. The
mechanism of injury during cytokine storm is poorly understood, but an
exaggerated initial response that persists over time is associated with
poor outcomes. Treatment with tocilizumab was initiated in all four patients to directly inhibit the IL-6 cytokine storm.
Interestingly,
three of these four patients presumably had asymptomatic COVID-19
infections, as they reported no recent symptoms of illness
yet had positive antibody testing. It is possible that the
mechanism of COVID-19 post-infectious cytokine release syndrome in
children is a post-infectious phenomenon related to an antibody complex mediated reaction.
|
30 children aged one day to 15
years, 23 with no predisposing conditions. All survived except an
11 year old girl who was undergoing chemotherapy for Acute Lyphocytic
Leukemia.
Higher representation of African American and Latino/Hispanic
patients. 177 patients to age 25. 44 in hospital of whom 9
were critically ill. Asthma was common, but not more so in
hospitalised patients than in those at home.
Only one patient - a 4 year old boy - was diagnosed as having Kawasaki
disease. He recieved PRVC ventilation. All survived.
This is a case report from Prague concerning an 8 year old girl with
severe inflammatory symptoms who received mechanical ventilation and at
one point lapsed into a coma. She recovered fully.
Her IL-6 was not particularly high. The report goes into some
detail about neutrophils, and mentions eosinophils being elevated at
one point.
They propose that some children are genetically predisposed to this
condition, which differs from ordinary Kawasaki disease in some ways -
in particular gastrointestinal symptoms - and from adult COVID-19 by
absence of lung symptoms.
The cause of Kawasaki disease is still unknown.
|
These researchers in Bergamo compared previous years' Kawasaki cases
with a group of 10 cases coinciding with the recent COVID-19 outbreak
there. The recent group was older and had more severe
symptoms than and which differed somewhat from those of the earlier
group. The recent group had a high proportion of hyponatremia
which was not present in the earlier group.
The rate of incidence, from a child population of about 1 million, was
30 times that of the average over previous years. All the new
patients survived.
They estimate the condition affects no more than 1 in 1000 children exposed to SARS-CoV-2.
Despite half a century having passed since Tomisaku Kawasaki first reported his 50 cases in Japan, the cause of Kawasaki disease remains unknown. The most accepted hypothesis supports an aberrant response of the immune system to one or more unidentified pathogens in genetically predisposed patients; however, the search for the infectious triggers has been disappointing. In Japan, during three epidemics recorded in 1979, 1982, and 1986, the highest Kawasaki disease incidence was seen in January, potentially suggesting that factors during winter months may trigger Kawasaki disease.
|
Vitamin D!!!
#msg
Here is what I wrote to the authors on 2020-06-11:
Dear Clinicians and Researchers,
I am writing to you because you are the corresponding author of one of
the 18 articles on Kawasaki disease and COVID-19 which I found recently
- none of which mention vitamin D.
Please see this 2016 research from Italy which shows that children with
Kawasaki disease averaged 9.2ng/ml 25OHD and that the worst affected
averaged 5.8ng/ml:
Even without this Italian report, or the recent reports of sub-30ng/ml
25OHD levels strongly correlating with the risk of severe COVID-19
symptoms (Alipio
https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3571484) and death (
Raharusun et al.
https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3585561),
it should be obvious to anyone with an understanding of vitamin D's
role in immune system regulation that vitamin D deficiency plays a
strong causative role in severe symptoms of COVID-19 for both adults
and children. I have linked to and quoted from some of this
research at
http://aminotheory.com/cv19/icu/ .
Please let me know any arguments you are aware of against the
hypothesis that vitamin D deficiency plays a strong and frequently
decisive role in the incidence of Kawasaki disease (once triggered by
an infection) and in the severe symptoms of COVID-19.
I have CCed Stefano Stagi and colleagues and Mary Van Buesekom.
Best regards
Robin Whittle
../ to the main COVID-19
page of this site.
To the index page of this site: ../../
Contact details and copyright information: ../../contact/
©
2020 Robin Whittle - please link to this site rather than copy the
whole of its contents Daylesford, Victoria,
Australia