Obesity, diabetes and COVID-19 severe symptoms
Here are references to some recent research regarding obesity,
diabetes (type 2 at least) and COVID-19. It seems that
several aspects of obesity directly increase the risk of severe
COVID-19 symptoms - and so the risk of permanent harm or death:
- Excessive numbers of adipocytes (fat cells), such as in the abdomen and in the fatty lining of the heart.
- Ectopic adipocytes in the lungs, other organs and muscles.
- These adipocytes expressing ACE2 on their surfaces, so making
them able to be infected by SARS-CoV-2. This and other ways in
which obesity - especially visceral obesity (around the waist) -
worsens COVID-19 outcomes is described in:
- These adipocytes creating pro-inflammatory signaling molecules,
worsening the cytokine storm of overly-aggressive, dysregulated, immune
response which causes severe COVID-19 symptoms.
- Circulating 25OHD (on which the immune cells and many other cell
types rely upon to feed their autocrine/paracrine signaling systems) is
reduced in obesity due to the downregulation of the gene which creates
the 25-hydroxylase enzyme in the liver - which is what converts D3 into
25OHD. I have not mentioned this article further below. Please
see:
Vitamin D Metabolism Revised: Fall of
Dogmas
Roger Bouillon, Dan Bikle
Journal of Bone and Mineral Research
Volume 34, Issue 11 2019-10-07
https://doi.org/10.1002/jbmr.3884
|
- I don't have time to read this dense article but it is surely
highly relevant to understanding the cellular and molecular mechanisms
by which obesity greatly exacerbates inflammation and so severe
COVID-19. I expect that a full understanding of this would
involve pathological failure of regulatory immune cells to function
properly, in part - probably in large part or entirely - due to
inadequate supplies of 25OHD for their autocrine signaling
systems. ../#vitd-autocrine .
The
Pivotal Role of Adipocyte-Na K peptide in Reversing Systemic
Inflammation in Obesity and COVID-19 in the Development of Heart Failure
Zi-jian Xie, Joel Novograd, Yaakov Itzkowitz, Ariel Sher, Yosef D.
Buchen, Komal Sodhi, Nader G. Abraham and Joseph I. Shapiro.
Antioxidants 2020, 9(11), 1129; 2020-11-14
https://doi.org/10.3390/antiox9111129
- There are some processes in common with obesity's causal relationship with severe influenza:
Obesity drives sepsis as well - a severe immune dysregulation disorder
which can be triggered by various types of infection and by burns.
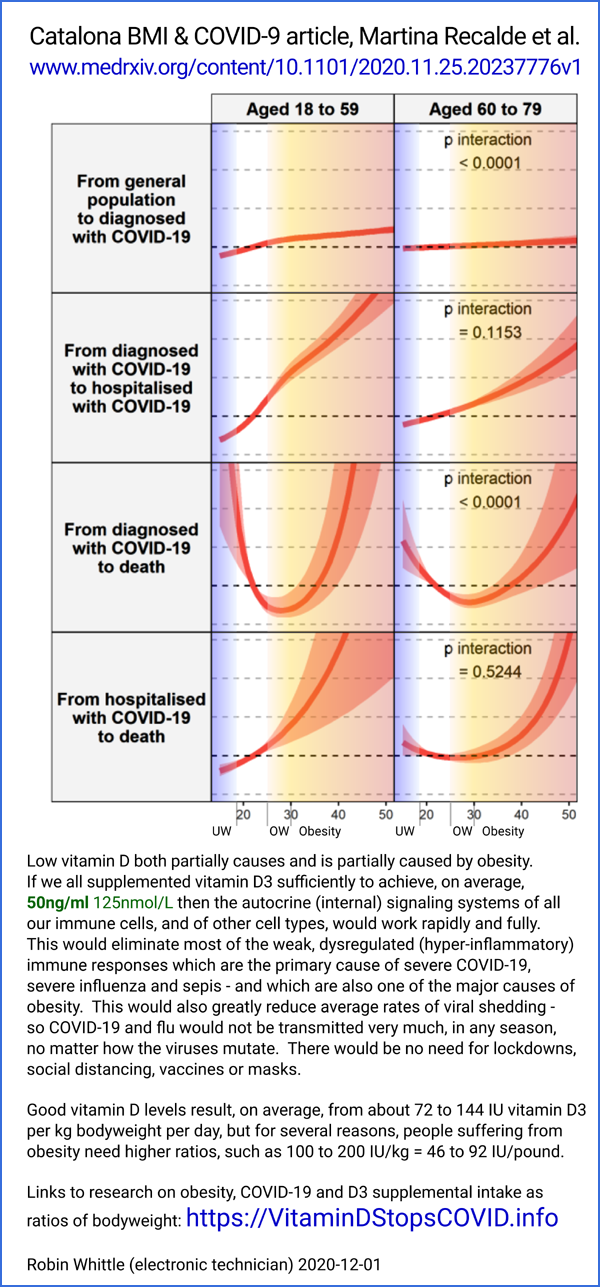
- This is a particularly interesting population based analysis:
Body
mass index and risk of COVID-19 diagnosis, hospitalisation, and death:
a population-based multi-state cohort analysis including 2,524,926
people in Catalonia, Spain
Martina Recalde, Andrea Pistillo, Sergio Fernandez-Bertolin, Elena
Roel, Maria Aragon, Heinz Freisling, Daniel Prieto-Alhambra, Edward
Burn, Talita Duarte-Salles 2020-11-28
https://www.medrxiv.org/content/10.1101/2020.11.25.20237776v1
|
The researchers found only a moderate association between high BMI and
risk of infection with SARS-CoV-2, for those under 80, with a steeper
association for those older than 80. Here are some of the interesting graphs:
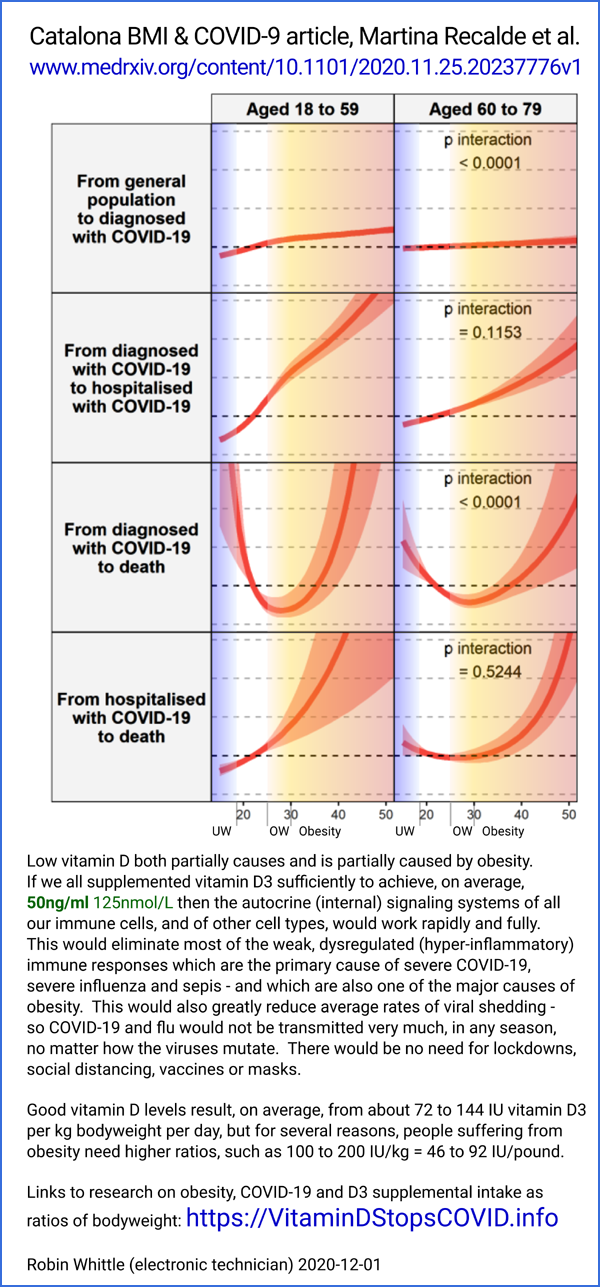
Perhaps
the very underweight are mainly the very aged and the MDs think
that there is little to be gained from intensive care.
My suggestions on vitamin D3 supplemental intake as a ratio of
bodyweight, with higher ratios for people suffering from obesity:
https://aminotheory.com/cv19/obesity/ .
I do not have time to keep up with the dozens or hundreds of academic articles on obesity and COVID-19. If you find any articles of particular interest in this field, please let me know and I will mention them here. Robin Whittle <rw@firstpr.com.au> .
Since obesity causes and is caused by low vitamin D 25OHD levels, most
observations of the immune dysregulation in people suffering from
obesity should be considered in light of the strong likelihood (to me
it is a certainty) that this
dysregulation will be greatly reduced or even eliminated by raising
25OHD levels rapidly and robustly. This is something which most
researchers and MDs do not consider. Be sure to read about
the molecular mechanisms of autocrine signaling failure of Th1
regulatory lymphocytes, and how this directly drives inflammation,
cytokine storm etc. due entirely to lack of vitamin D 250HD: ../icu/#2020-McGregor .
Most of these pages here under
/cv19/ concern the need for robust vitamin D supplementation, but see especially my proposal for using both
25OHD calcifediol and bolus D3 at the same time, as soon as possible,
for anyone with severe or potentially severe COVID-19: ../#25plusD3
. This includes anyone suffering from obesity who has not yet
contracted COVID-19 - because sooner or later they probably will.
The sooner everyone's 25OHD levels are brought to healthy ca. 50ng/ml
levels the better. It would be very difficult to give obese people
enough D3 to cause toxicity, and that would take months to occur
anyway. Since obese people face grave challenges with immune
dysregulation in the face of COVID-19, I would be inclined to aim for
higher levels, such as up to 100ng/ml . See ../d3
for the self-limiting nature of 25OHD levels and how toxicity only
becomes a concern at levels over 150ng/ml (375nmol/L). See also my
proposal for using ratios of bodyweight to decided D3 supplementation
quantities, with higher ratios for those suffering from obesity: https://VitaminDStopsCOVID.info/01-supp/ ,
When wondering why some countries or groups of people within countries
have better or worse outcomes with COVID-19, vitamin D and other
nutrients are surely an important factor, as are on-average genetic
differences between particular groups of people such as ../#haplotypes . Varying rates of obesity surely play a role as well
This is a cursory discussion of the field and I have no medical training. (../#disclaimer)
Robin Whittle rw@firstpr.com.au
. 2020-07-18 Last update 2022-01-05
To my other website: https://VitaminDStopsCOVID.info .
To the main COVID-19 page of this site: http://aminotheory.com/cv19/,
concerning nutritional supplements - especially vitamin D and boron -
for all adults and some children ASAP, so their immune system firstly
fight the SARS-CoV-2 virus well, and secondly, if the infection gets to
the lungs, will not respond with a dysregulated, overly-inflammatory
way which causes the serious harm and risk of death.
Links such as [W] are to the relevant Wikipedia page.
Be sure to read the Disclaimer!
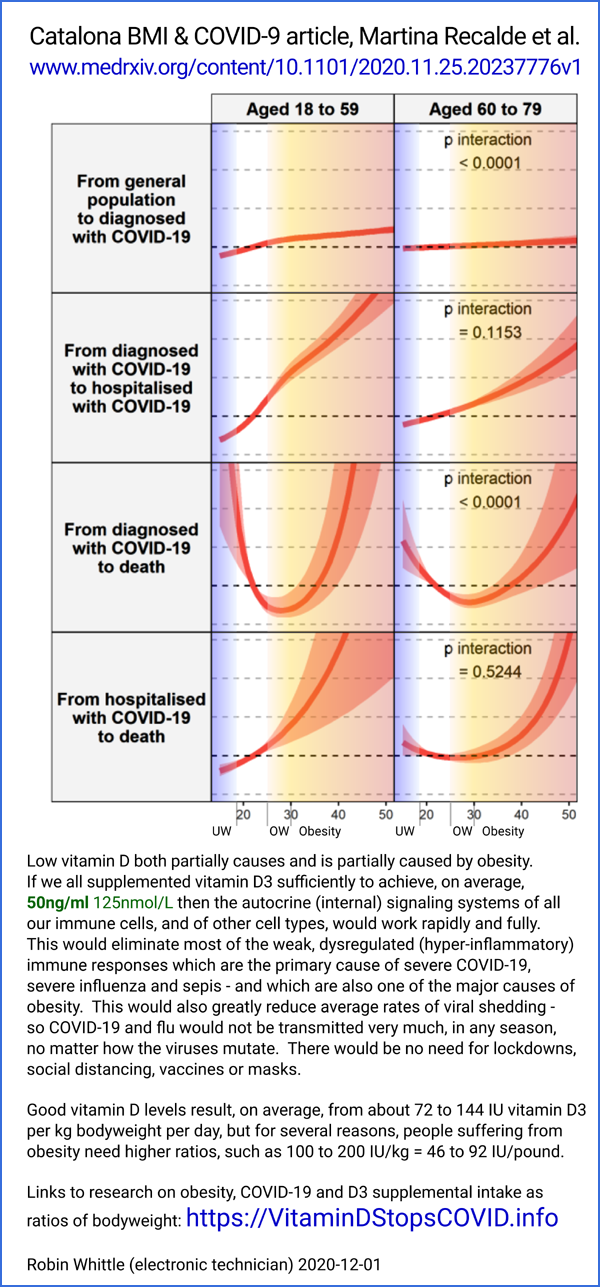
Obesity itself, even after correcting all nutritional deficiencies
and excesses, is likely to remain a serious risk factor for harm from
COVID-19, due to the activities of fat cells
It is very well known that being
overweight or especially obese is a high risk factor for COVID-19
severe symptoms and death. "Severe symptoms" doesn't just
mean having a hard time in hospital. It almost certainly means
microembolisms and perhaps larger blood clots in multiple organs -
lungs, brain, spinal cord, heart, liver, kidneys etc. - which can lead
to lasting disability.
There's a lot of talk about the death rate from COVID-19 being no worse
than influenza once the true number of people who were infected is
known. While I am not sure this is the case, even if it was,
COVID-19 with severe symptoms - and sometimes with few symptoms - leads
to a terrible burden of damage due to the hypercoagulative state of the
blood which results naturally from the high level of damage (killing
and breaking up) of the endothelial cells (the inner lining of blood
vessels) especially in the lungs. No illness before this -
with the possible exception of SARS (SARS-CoV) - leaves such a trail of
this kind of damage , much of which may be permanent. I
have read many reports from nurses and doctors stating they have never
seen anything like this illness. A 2020-07-08 report on
neurological damage even for some people with mild symptoms:
Yet for most people, there are few if any symptoms. The virus
itself need not be problem - but it is if the person's immune system is
weakened and/or dysregulated to the point of being self-destructively
overly-inflammatory.
Obesity correlates with various other conditions associated with severe
COVID-19 symptoms. There's a lot of research concerning
these to low vitamin D levels. I think it is reasonable to assume
that, over many years, low vitamin D levels are a significant
contributing cause to most or all of the conditions which are
considered comorbid with severe COVID-19 symptoms. Since COVID-19
didn't cause these conditions, they are direct contributing causes of
COVID-19 severe symptoms and/or they are results of some other,
separate, conditions (including genetic variation between individuals)
which contribute both to the development of the condition and to
COVID-19 severe symptoms.
While low vitamin D levels surely, to some extent at least, contribute
to the development and maintenance of obesity, obesity itself
contributes to low vitamin D levels because vitamin D - in its most
important blood circulation borne form, 25 hydroxy vitamin D AKA 25OHD
- is fat soluble. So 25OHD which would normally be in the blood
(in solution and bound to vitamin D carrier protein) is diverted to
adipocytes in fatty tissues all around the body. There, it may be
slowly degraded - so as far as I know little of this is available to be
returned to the blood unless the fat is metabolised to produce energy.
So for a given intake of supplementary vitamin D3 plus whatever comes
from sun exposure and food (both usually too low to reach the 40 to
60ng/ml 25OHD levels required for good health - see the main page)
obese people have less D3 and so 25OHD (D3 is converted in the liver
into 25OHD) in their blood than other people. This is
partly due to their bodies being bigger, and so presumably having a
greater volume of blood, but it is also due to them having much more
fat than usual, with the 25OHD (and I guess the unconverted D3) going
there and generally not returning to the blood.
To the extent that low vitamin D levels (25OHD in circulation) drives
obesity, and to the extent that obesity drives low 25OHD levels, there
is a positive feedback loop where the two conditions drive each other
and so are more difficult to escape than either would be alone.
The extra vitamin D needs of obese people needs to be remembered when
considering D3 dosage. See the main page for graphs and
discussion of supplementary D3 dosage according to body weight and the
resulting 25OHD levels.
../#2014-Ekwaru and
../#2020-Baker-a .
In mid -July 2020 I knew that obesity was perhaps the biggest single risk factor for COVID-19 severe symptoms and death.
I had been optimistic that if these people could take suitably large D3
supplements to raise their 25OHD levels safely above 40ng/ml
(100nmol/l) - and ideally higher, above 60 or so, since this is still
far from the 150ng/ml levels where vitamin D toxicity might occur - in
the weeks and months before contracting COVID-19, that they would be
largely protected from serious symptoms and death.
This was based on the idea that their obesity was only a marginal
actual driver of severe symptoms and that the real risk factor was
their low vitamin D levels. However, some of the research I
mention below strongly suggests that there are several aspects of
obesity itself which directly drive COVID-19 disease
mechanisms.
Obesity is a tough problem. There's nothing below regarding how
to tackle it, other than the assumption that everyone - including
especially obese people - really need to get all their nutrients sorted
out, because deficiencies in vitamin D and other micronutrients AND
excesses of salt and insufficient potassium are extremely common and
drive numerous chronic illnesses, including obesity.
Please see the main page
../ for numerous research articles concerning vitamin D and other nutrients and immune system health.
Please see
this page at
VitaminDWiki for links to research on COVID-19 comorbidities, including overweight and obesity.
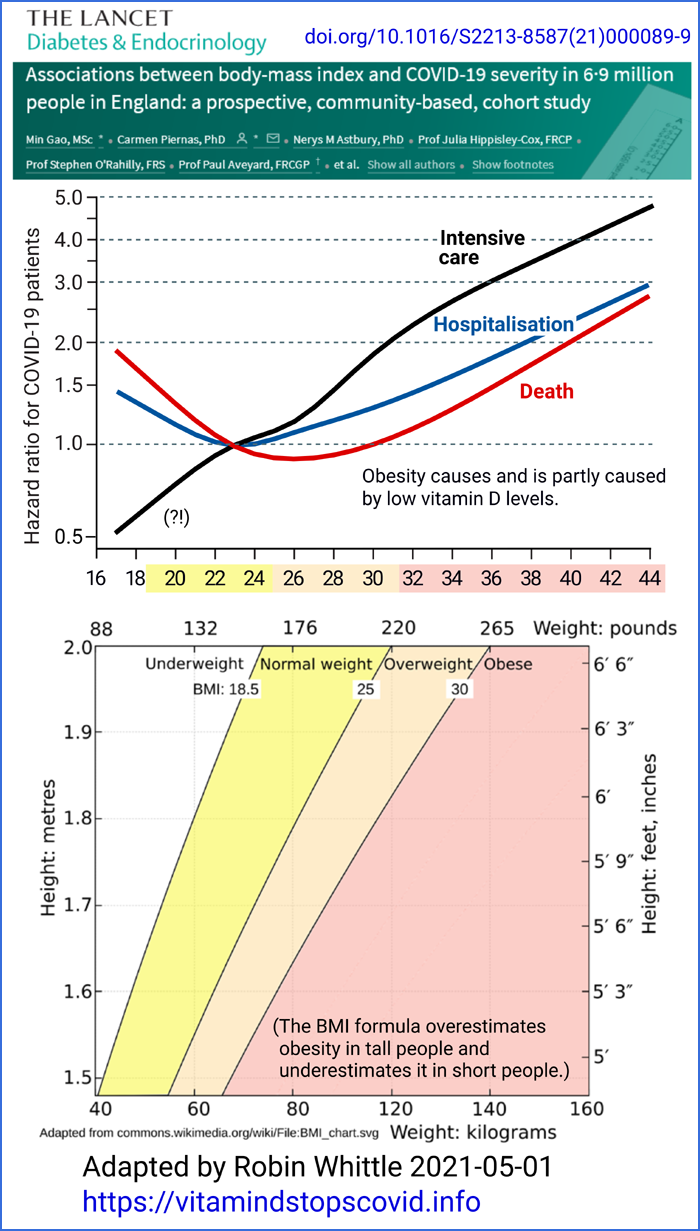
Below is a chart I adapted from this article, by extending the scale to 100%:
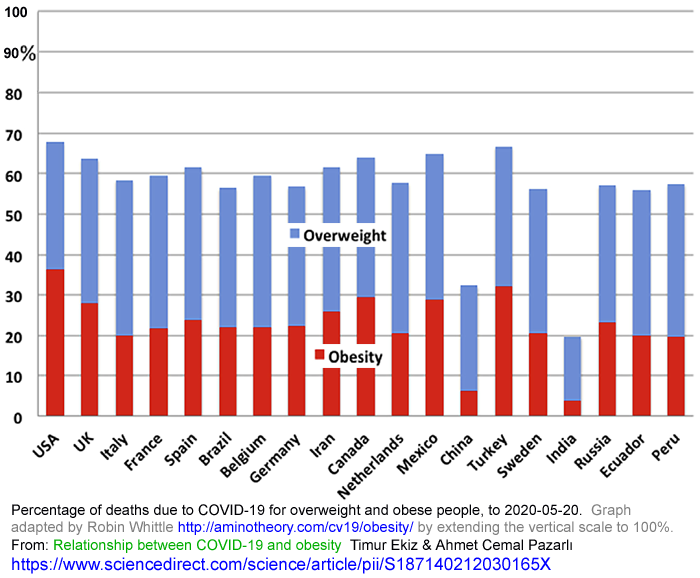
These need to be considered in light of the prevalence of overweight
and obesity in the general population - which is not provided.
The authors highlight vitamin D supplementation as one of the
approaches to be employed fighting COVID-19 in the context of
overweight and obesity.
Adipocytes (fat cells) play several roles in COVID-19 severity
While several aspects of obesity,
including the chronic inflammatory response (no-doubt driven in large
part by vitamin D levels well below the safe 40 to 60ng/ml levels
recommended by MDs and vitamin D researchers - see the main page)
probably drive COVID-19 severity, this article explores direct
mechanisms resulting from the activities of adipocytes.
Complex interactions occur between the immune system and adipose tissue. The overexpression of inflammatory adipokines from visceral
fat depots can affect the immune response, impair the chemotaxis, and
alter the macrophage differentiation. The imbalance between anti-
and pro-inflammatory adipokine secretion from thoracic visceral fat depots, such as the epicardial and mediastinal, can also play a role in the cytokine storm described in patients with severe SARS-CoV2.
|
Adipokines [
W] are cell-signaling secreted by adipose (fat) tissue.
Visceral,
in this context, refers to the internal organs. Visceral fat
refers not only to fat in the organs, but in the area of the organs -
around the abdomen - AKA belly fat AKA active fat:
Thoracic fat is an uncommon term, defined
here
as "adipose tissue from the right pulmonary artery to the diaphragm and
from the chest wall to the descending aorta" - so I think this means
fat surrounding the heart.
As you can see from the main CV19 page
../ an overly
inflammatory immune response to the SARS-CoV-2 viral infection in the
lungs leads directly to the cytokine storm and endothelial cell damage
there, which drives COVID-19 severe symptoms directly and via the
resulting hypercoagulatory state of the blood.
Interestingly, adiponectin was reported to predict mortality in critically ill (COVID-19) patients upon admission to the intensive care unit. The innate
inflammatory response of the visceral fat depots can cause an
upregulation and higher release of inflammatory cytokines such as IL-6.
Excessive pro-inflammatory cytokine release was thought to be the link
between visceral obesity and influenza-related severe respiratory
complications. As elderly individuals are at higher risk of
COVID-19 complications and poorer outcome, it is worth noting that
aging can cause visceral fat accumulation and adipose tissue
inflammation and fibrosis.
|
Adiponectin [
W]
is a protein hormone involved in regulating blood glucose levels and
fatty acid breakdown. (Fatty acids are fats - and are an
essential part of all cells.) It is expressed primarily in
adipocytes but also in muscle and the brain. Although its
244 amino acid protein sequence is different, its overall structural
shape closely resembles that of Tumor necrosis factor alpha
TNFα [
W]
. TNFα
along with IL-6 (interleukin 6) is one of the several pro-inflammatory
cytokines which drive the overly-aggressive immune response which is a
crucial part of severe COVID-19 symptoms.
Tocilizumab, Adipokines and Severe Complications of COVID-19
Antonella
Fioravanti, Brunetta Porcelli, Lucia Terzuoli, Maria Romana Bacarelli,
Sara Tenti Sara Cheleschi. Clinical Drug Investigation 2020-07-13
https://doi.org/10.1007/s40261-020-00950-2
|
The first thing which caught my eye in this article was the mention of
ectopic adipocytes - fat cells in locations they do not belong. I had not heard of this. The reference they give is to the
Malavazos article, which doesn't mention them. These articles goes into some detail:
The
Release of Adipose Stromal Cells from Subcutaneous Adipose Tissue
Regulates Ectopic Intramuscular Adipocyte Deposition. In
rats, subcutaneous (beneath the skin) adipocyte progenitor (leads to
the creation of) cells and/or stromal (connective tissue cells
associated with fatty tissues) could be released into the circulation
and lodge at other locations in the body, leading to ectopic adipocytes
which the researchers showed were involved in insulin resistance [
W] and metabolic disorders [
W]. (Ectopic lipid deposition.)
The link between obesity and acute lung injury during infection can be
partially explained by the activation of the renin-angiotensin system.
It has been supposed that the virus uses an angiotensin-converting
enzyme 2 (ACE2)-dependent mechanism of cellular entry; this receptor is
also expressed in adipocytes, including ectopic adipocytes within the
alveolar interstitial.
|
Regarding the renin-angiotensin system [
W] which regulates blood pressure, and COVID-19, this is one of many articles of interest:
"alveolar interstitial" means the cells surrounding the alveoli - the
tiny air pockets in our lungs where oxygen and carbon-dioxide exchange
occurs with the blood. So it seems that obesity (by
implication in this context, but perhaps other conditions too) can lead
to fat cells accumulating in the lungs, as well as better known
locations in the liver and heart.
I found this article concerning
ectopic adipose tissue in the lungs. (All this is quick searching - a thorough treatise on these matters would take weeks.)
Growing data suggest that some patients with severe COVID‐19 infection
can develop a condition described as “cytokine storm”. Interestingly,
excess fat is associated with complement system overactivation, potentially capable of inducing inflammatory sequelae ultimately leading to such complication.
|
The complement system [
W] is part of the innate immune system which enhances (complements) the ability of antibodies and
phagocytic (cell destroying) immune system cells to clear
microbes
and damaged cells from an organism, promote inflammation, and attack
the pathogen's cell membrane. With a dysregulated immune
response (which caused or at least worsened by vitamin D deficiency),
this can damage healthy cells.
Visceral adipose tissue is capable of secreting IL-6,
whose levels were found to be retrospectively increased in
SARS-CoV-2 non-survivors.
|
If the important role of ectopic visceral and liver fat in
the pathogenesis of some of the obesity complications is recognized,
close to nothing is known about the possible accumulation of adipocytes
within the lung, although some evidence suggests its contributing role
to pulmonary injury. In fact, preclinical data demonstrated that fat
droplets accumulate within the alveolar interstitium in obese diabetic
rats,
and recent evidence obtained from a small population confirms that
subjects with obesity present accumulation of adipose tissue within the
lung parenchyma, its presence correlating with the inflammatory
infiltrate.
|
Terminology:
Parenchyma means the main tissue, in this case of the lungs.
The inflammatory infiltrate
refers to the set of immune system cells and (I guess) various
compounds including cytokines etc. which are present in inflamed
tissue, in the lungs in this case, and which presumably cause this
infiltration.
Edema, below: swelling caused by excess fluid trapped in the tissue.
We therefore hypothesize that obesity could play a role in predisposing
to serious COVID‐19 complications through several mechanisms: systemic
chronic inflammation, related comorbidities such as diabetes, increased
complement system activation and IL‐6 secretion. Ultimately, excess fat
could also lead to the possible presence of ectopic adipocytes within
the alveolar interstitial space that may suffer direct viral infection
and in turn aggravate the inflammatory infiltrate, therefore
contributing to the massive interstitial edema being observed.
|
Back to the
Fioravanti article.
We can postulate that obesity
may predispose to the development and progression of the COVID-19
disease through several mechanisms. Growing evidence demonstrated
that adipose tissue is an active endocrine organ and secretes many substances known as adipocytokines such as adiponectin, leptin, resistin, visfatin, chemerin, tumor necrosis factor TNF-α, IL-6,
factors of the complement system, growth factors, and adhesion
molecules, involved in the regulation of several processes including inflammation and immunity. Then, an abnormal secretion of adipocytokines from fat tissue can contribute to development of the condition described as cytokine storm which characterized the severe form of SARS-CoV-2.
|
They then discuss Tocilizumab [
W]
which is an artificial antibody which binds to and inhibits the IL-6
receptor. It is used in treating rheumatoid arthritis (RA) [
W].
Obligatory sidebar on yet
another disease which is associated with - and so no-doubt to a
significant extent caused by - deficiency in vitamin D and perhaps
other micronutrients
Google Scholar
search for:
"rheumatoid arthritis" "vitamin D"
This shows plenty of articles reporting low vitamin D is associated with RA.
No doubt Tocilizumab is helpful with RA and other such inflammatory diseases.
Q Why give an expensive, patented, drug
before trying to replete the sufferers in all nutrients known to be
involved in immune system health, and therefore which can be expected
to reduce the excessive inflammation which drives RA? (Vitamin D,
boron, omega 3 fatty acids, vitamin C and others.)
A There's a lot more money to
be made by selling drugs like this than from vitamin D or other
nutrients. Also, it gives the doctors and perhaps the patients
the impression that they are using a targeted, highly sophisticated, weapon of choice which directly reduces an important aspect of the disease.
Repeating the search with boron I found an article showing RA patients
have half the boron in their blood than controls. See the boron
section of the cv19 page:
../#boron-ra .
Assuming this is valid, it would not be surprising (especially in the
context of the research linking low boron to excessive inflammation) if
boron supplements helped reduce COVID-19 symptoms, obesity etc. etc.
They state that Tocilizumab treatment reduces the levels of circulating
leptin, chemerin, plasminogen activator inhibitor-1 (PAI-1), and
fibrinogen, while boosting the levels of
adiponectin:
Adiponectin
is an adipokine with insulin-sensitizing and anti-atherogenic
properties; hypoadiponectinemia [low levels of adiponectin] has been
shown to be associated with obesity, diabetes, metabolic inflammatory
syndrome and inflammation, also, low serum levels of adiponectin were
reported as predictor of mortality in critically ill patients in
intensive care units.
|
They describe the functions of two compounds mentioned above which are
produced by adipocytes, with the implication that having extra
adipocytes, as in obesity, and especially having ectopic adipocytes in
the lungs, would tend to cause worse, more inflammatory, outcomes with
COVID-19:
Leptin has pro-inflammatory properties stimulating the production of TNF-α, IL-6, and IL-12 and potential atherogenic effects. Chemerin
is a novel adipokine involved in inflammation (stimulates chemotaxis,
macrophages, and dendritic cells, induces the release of IL-6), in
coagulation and fibrinolysis; furthermore, elevated circulating chemerin levels correlate with endothelial dysfunction.
|
Diabetes, obesity and COVID-19 severity
Extra fat impedes ventilation - in normal and mechanically-assisted breathing.
According to this
article,
epicardical adipose tissue is the fat depot that exists on the surface of the myocardium and is
contained entirely beneath the pericardium [
W],
thus surrounding and in direct contact with the major coronary arteries
and their branches. This fat surrounding the heart is regarded
as a biologically active organ that may play a role in the association
between obesity and coronary artery disease (the largest cause of death
in the world).
Obesity
is associated with immune dysregulation and chronic inflammation that
could mediate progression toward organ failure in severe COVID-19
patients.
Myocarditis and cardiomyocyte dysfunction could be worsened by local biological effects of epicardial adipose tissue, a source of adipokines and pro-inflammatory mediators, and the volume of epicardial adipose tissue is directly associated with BMI.
Moreover, ACE2 is highly expressed in the epicardial adipose tissue of patients with obesity. This could promote virus internalisation into the adipocytes and enhance TNFα and IL-6 release
|
So the fat cells protecting the heart and enclosing the arteries
carrying blood to the heart muscles may become infected by SARS-CoV-2 -
and this part of the body may be subject to further immune system
overly-aggressive inflammatory destructive responses.
Obesity and diabetes are characterised by chronic low-grade inflammation
with increased concentrations of pro-inflammatory leptin and reduced
anti-inflammatory adiponectin. Additionally, people with obesity
are often physically inactive, more insulin resistant, and with gut
dysbiosis, which might increase the inflammatory response to infection
with SARS-CoV-2. Moreover, individuals with obesity have lower vitamin D concentrations, which could also reduce the immune response. The role of vitamin D supplementation is currently being investigated in ongoing clinical trials.
|
A dysregulated inflammatory innate and adaptive impaired immune response
might occur in patients with diabetes, accounting for the systemic
tissue damage and respiratory and multiorgan failure. The cytokine storm
is more likely to develop in patients with diabetes, as diabetes is
already characterised by low-grade chronic inflammation. Moreover, in
the case of high viral load, the capacity to raise an acute immune
response might be compromised in patients with diabetes, exposing them
to more severe adverse effects.
One study reported that patients with COVID-19 with diabetes had higher
concentrations of inflammation-related biomarkers, such as C-reactive
protein, serum ferritin, and IL-6, and a higher erythrocyte
sedimentation rate, compared with patients with COVID-19 without
diabetes.
|
"Erythrocyte
sedimentation rate" [
W]
refers to how quickly red blood cells, in the presence of an
anticoagulant, settle in a test tube over an hour.
According to
medlineplus.gov : "A faster-than-normal rate may indicate inflammation in the body. Inflammation is part of your immune response system.".
Most people have inadequate vitamin D, boron and omega-3 fatty
acids. Adequate levels of these are known to reduce the excessive
inflammation which results from immune system dysregulation. See
the main page
../ for more details.
Some other articles regarding obesity, diabetes and COVID-19
I haven't had time to look at these yet.
Commentary: COVID-19 and diabetes mellitus: What we know, how our patients should be treated now, and what should happen next
Angeliki M. Angelidi, Matthew J. Belanger, Christos S. Mantzoros. 2020-04-19 Metabolism
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7167295/
|
Obesity and Higher Risk for Severe Complications of Covid-19: What to do when the two pandemics meet
Alessandra Valerio et al. J Popul Ther Clin Pharmacol 27(S Pt 1):e31-e36 2020-06-29.
https://pubmed.ncbi.nlm.nih.gov/32650354/
|
../ to the main COVID-19
page of this site.
To the index page of this site: ../../
Contact details and copyright information: ../../contact/
©
2020 Robin Whittle - please link to this site rather than copy the
whole of its contents Daylesford, Victoria,
Australia