Vitamin D Supplementation Guide - for those (most of us) who are
likely to get COVID-19 before too long - and especially for those who
are aged, overweight, obese, or suffering other conditions which create
high risks of serious symptoms, harm and death.
The best research indicates that we should aim for higher vitamin
D levels - and so take greater amounts of supplemental vitamin D - than
is recommended by most government health authorities.
2021-01-31: Please see an important update regarding mutations in the SARS-CoV-2 viruses which cause COVID-19.
The British variant is more transmissible. The separately evolved, but
otherwise identical, South African and Brazilian strain are more
transmissible still. There's no reason to believe they are less
harmful, and some reasons to believe they are at least as harmful or
more.
Researchers in Israel and France ran experiments with yeast (not
viruses) to evolve, in an accelerated manner, the likely mutations
which would give rise to more transmissible variants of SARS-CoV-2, due
to the variations in the spike protein's Receptor Binding Domain having
a greater affinity for the ACE-2 receptor. Their experiments evolved
mutations including the same three which cause the South African /
Brazilian strain to be much more transmissible. Their experiments
also discovered other mutations which would make still more
transmissible variants of SARS-CoV-2, but which have not yet evolved in
the virus. The British strain has 3.5 times the RBD affinity for ACE-2 of the strains common in mid-2020. The South African / Brazilian strain has 12.7
times this affinity. Their experiments found multiple combinations of
mutations, including one which conferred an approximately 640 times the affinity of mid-2020 strains.
It is reasonable to expect that the viruses, in the wild, in the months
and years to come, will evolve to embody at least some, and perhaps
all, of the mutations this team discovered - and there may be other
mutations as well which increase transmissibility.
Therefore, we cannot assume that the strains which affected most
countries in the middle of 2020 will be the ones we have to contend
with now, in early 2021, much less later in the year and in the future.
These mutations tend to make immunity from prior infections or vaccines
against older strains less effective, so reinfection with new strains
seems possible and likely.
Perhaps future strains with very high RBD affinity for ACE-2 will
render any vaccine-induced immunity, and perhaps infection induced
immunity, much less able to prevent infection, or to reduce the extent
of an infection once it starts. If so, then vaccines, social
distancing, masks, lockdowns etc. will be even less effective than they
are today.
Since population-wide, year-in year-out, antiviral drugs are
impractical and undesirable, then the only option would be to do what I
and others have been suggesting since March 2020: population-wide
substantial supplementation with vitamin D3 and ideally other nutrients
to boost strong initial immune responses to the infection and, most
importantly, to reduce, as much as possible, the common tendency for
the dysregulated, hyper-inflammatory, self-destructive immune responses
which cause some people to have severe COVID-19 symptoms.
I worked unsustainably on these websites from March to December 2020.
I will try to update them with the very most significant research, such
as just mentioned - but in general I need to get back to my work with
electronic musical instruments.
|
|
Robin Whittle rw@firstpr.com.au
. 2020-08-02 Last update 2020-08-08 15:00 UTC
2020-11-19 update: Please see a later page where I suggest D3 supplemental intake quantities as a ratio of bodyweight:
and these two sections of where I suggest a combination of 25OHD
calcifediol and bolus D3 for urgent treatment of people with severe or
potentially severe COVID-19 symptoms, flu or sepsis:
To the main COVID-19 page of this site: http://aminotheory.com/cv19/,
concerning nutritional supplements - especially vitamin D -
for all adults and some children ASAP, so their immune system firstly
fight the SARS-CoV-2 virus well, and secondly, if the infection gets to
the lungs, will not respond with a dysregulated, overly-inflammatory
way which causes the serious harm and risk of death.
The updates/ page lists all the significant updates to these cv19 pages.
Links such as [W] are to the relevant Wikipedia page.
Links such as [DW] are to Henry Lahore's remarkable Vitamin D Wiki.
Be sure to read the Disclaimer!
I am not a doctor, and even if I was, I have not examined you.
Doctors can bring vast experience and knowledge to bear on your
particular situation. It is a very high level skill of immense
potential value to you. However many doctors don't know as much
as they should about nutrition - for reasons I discuss below.
A few key points before all the details
The purpose of this page is to help you or your doctor decide, by
reference to the best research, how to improve your general health -
and especially your immune system health - with vitamin D
supplements. Before getting to the detailed material, here are a
few important points - all of which are explained further below or on the main
cv19
page and those which branch from it.
- There's very little vitamin D in food, including fortified food. By all means eat eggs, oily fish (excellent
for omega 3 fatty acids) - but no palatable amount of these will give
you more than a small fraction of the vitamin D you need to be healthy.
- Many multivitamins
contain vitamin D (ideally D3). Likewise many calcium
tablets. At best, these can provide you with only a fraction of
the vitamin D you need to be healthy.
- Direct (not through glass or sunscreen), high elevation (midday - not early morning or late afternoon) sun exposure
on your skin will produce vitamin D3. However, most people cannot
get this all year round, and even then not all people can raise their
vitamin D levels enough to be replete. All such exposure to short
wavelength (about 295nm) UVB radiation, from the Sun or from tanning
lamps, inevitably causes DNA damage and so increases the risk of skin
cancer.
You only need about 1/3 as much UV as causes pinkness to maximise the
skin's production of vitamin D - and this only needs to be done once a
day. ../#vitd-basics So there are ways of using UV exposure to get good amounts
of vitamin D, while minimising skin damage and risk of cancer.
People with brown or black skin need a lot more UVB light than white-skinned people to produce significant amounts of vitamin D. As we age, it gets harder too.
Most people wisely protect themselves from the UVB component of sunlight.
This and the two points above means that without
supplements, most people, in most countries, do not get the vitamin D
levels in their blood which current research shows is necessary for
good health - especially immune system health.
- Most or all the people who suffer severe symptoms from COVID-19
do so because their immune system is weak and/or dysregulated.
"Dysregulated" means overly aggressive, hyper-inflammatory and so both
ineffective against the viral infection and self
destructive. This leads to the cytokine storm which damages
the epithelial cells which form the inner lining of blood
vessels.
This
occurs particularly in the lungs, and when the body senses damage
to blood vessels, it puts the blood into a hypercoagulative
state. It is this state - thick blood sponteneously forming
tiny blood clots (microembolisms) all over the body - which does
terrible harm to people with severe COVID-19 symptoms.
In some cases this can begin when people only have relatively mild
symptoms, such as no breathing difficulties. Microembolisms can
form in all organs - the brain, heart, lungs, liver,
kidneys, spinal cord etc. This can cause lasting damage and
organ failure. Larger blood clots in the brain cause stroke and
in the heart, heart attack.
Vitamin D deficiency is the most important, easily correctable cause of
immune system weakness and dysregulation. Omega 3 fatty acids
(oils) as found in fish oil and from algae sources are deficient in
most people. Increasing intake of these, with oily fish and or
supplement capsules will greatly assist the immune system. Like
vitamin D, and omega 3 fatty acids, research shows that boron and some other nutrients such as zinc, play an important role in
improving immune system regulation, including especially by reducing
the chances of the hyperinflammatory cytokine storm which drives
COVID-19 severe symptoms. All this is explained, with links
to research articles, on the main cv19 page and those which branch from it.
- Most
people need substantial vitamin D supplements in order to attain the 40
to 60ng/ml target blood levels recommended in the articles cited
below.
Many people buy 0.025mg (1000IU) D3 capsules and think that one a day
is a good supplemental intake. (In Australia, this is the
maximum amount of D3 for tablets or
capsules can be sold in shops, though some online sellers and
naturopaths supply
higher capacity capsules.)
- Vitamin D3 is much preferred. This is the same vitamin your
skin makes when illuminated by UVB light, such as from high elevation
sunlight. Use D2 if that is all you can get, but its half life in
the body is shorter. For some bizarre reason I am yet come to
understand, in the USA, doctors can only prescribe D2.
- For any given body weight and D3 intake (plus food and D3 from
UVB light) there is quite a variation in the resulting blood
levels. D3 is converted, over a period of a week or so, in the
liver, into the form of vitamin D which is stored in the blood over the
longer term - months. An OH (hydroxyl group - oxygen and
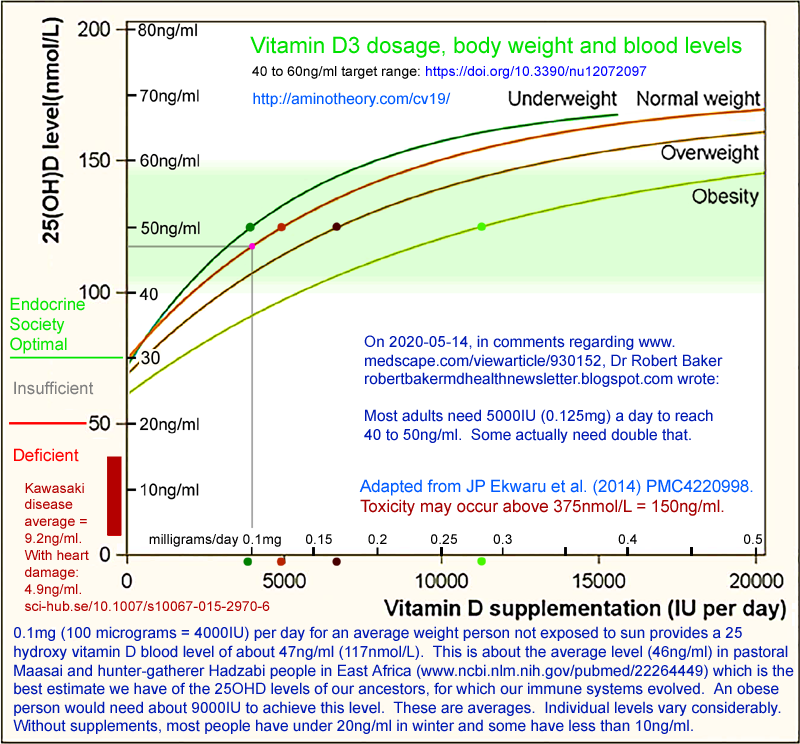
hydrogen) is attached at the 25 position (top right in the diagrams below) to form 25 hydroxy vitamin D,
AKA calcidiol and 25OHD:
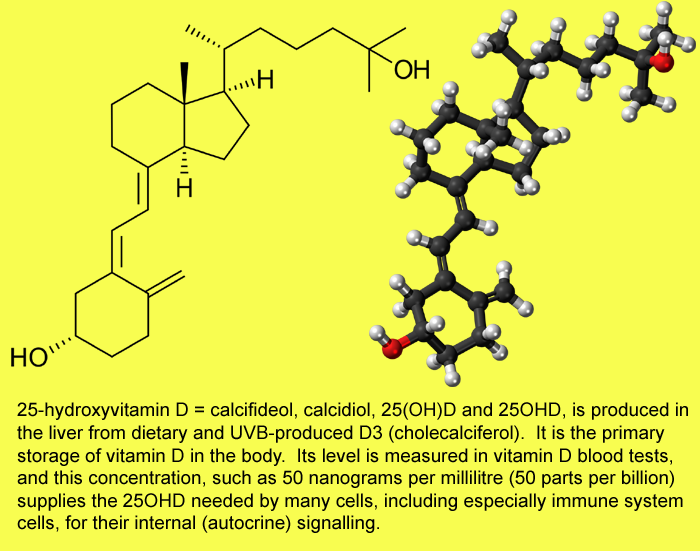
(Images from Wikipedia.)
- The 25OHD level in the blood is the most important
factor controlling numerous processes in the body, especially the
ability of many types of immune system cells to conduct their internal
signaling, respond to inputs and so directly fight infection and/or
regulate other aspects of the immune response so as not to damage the
self.
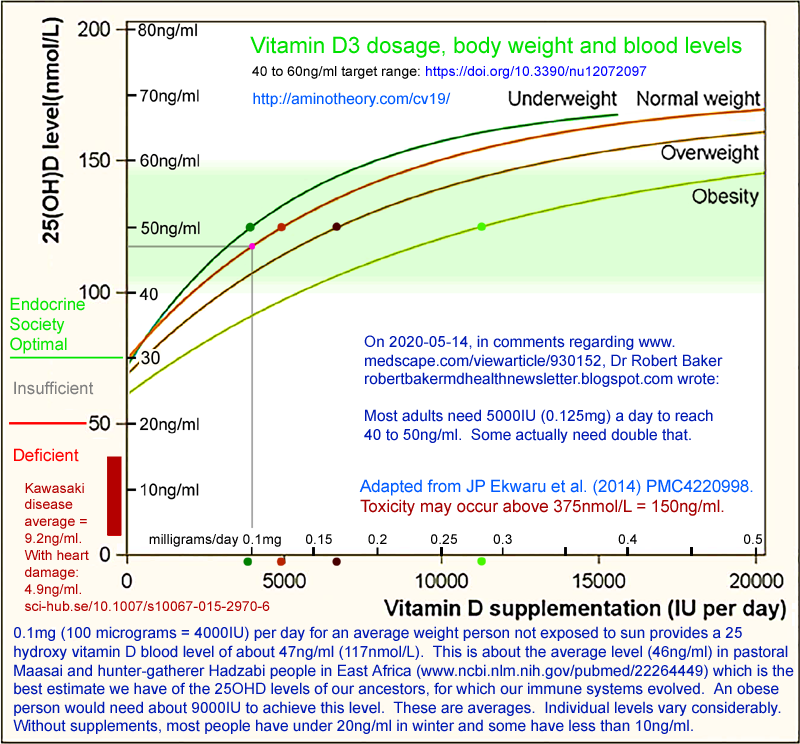
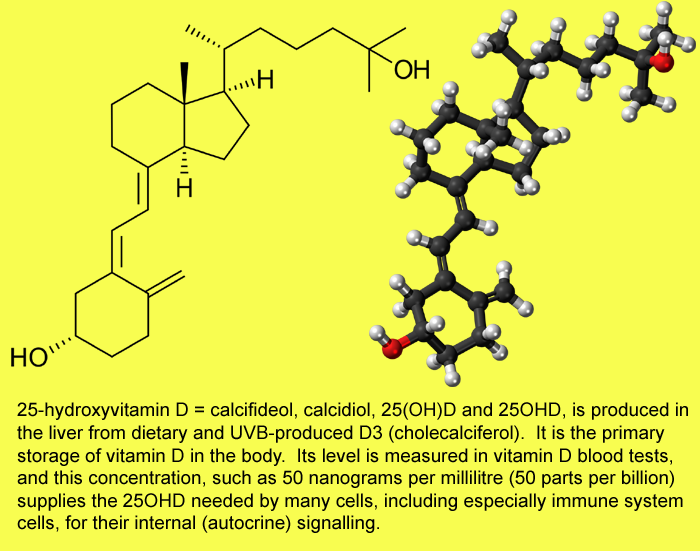
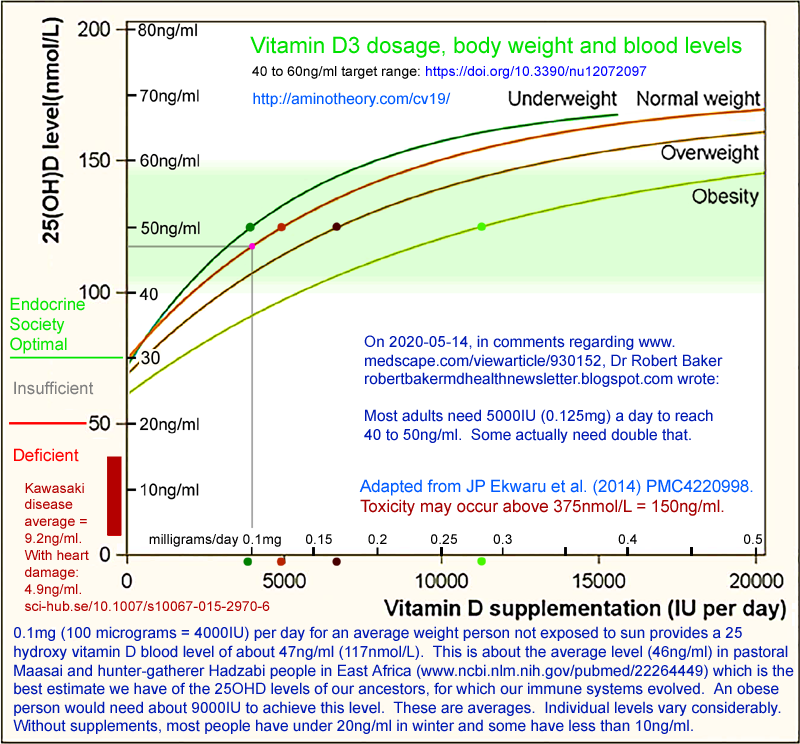
Above is a graph of 25OHD blood levels according to body weight and
D3 supplemental intake. These are averages over many
people. However there is a great deal of variation between
individuals, for various genetic reasons which are somewhat
understood, and for numerous reasons which remain a mystery.
One
of the variables contributing to these different 25OHD outcomes is
what sort of meal the D3 supplements are taken with, if any.
I found conflicting research on this, which I discuss in the
final section below.
- 0.1mg to 0.15mg (milligrams = thousandths of a gram), also known as 4000IU (International Units) to 6000IU, is a perfectly good daily dose for average weight adults.
In the UK, the recommended daily D3 dose is 0.01mg (400IU) and in the
USA and many other countries, it is 0.015mg (600IU). These
recommendations are one tenth of what most people need. These
government recommended daily doses are just plain wrong. Researchers and MDs who are most up to date with vitamin D research
have been arguing against these very low recommendations since 2008.
- Overweight and obese
people need extra vitamin D in part due to their larger bodies, but
also due to their larger proportion of fatty (adipose) tissue, which
sequesters the vitamin D. So 0.2mg to 0.3mg (8000 to 12,000IU) or more is appropriate.
- According to the best research, and the urging of vitamin D experts - MDs and researchers - since 2008 everyone should aim for 40 to 60ng/ml
vitamin D levels in their blood. (100 to 150nmol/L.)
This is significantly higher than other, still widely used, thresholds
above which vitamin D is regarded as sufficient: 30ng/ml (Endocrine Society), 20ng/ml (USA) and, most scandalously - despite decades of protests by vitamin D experts - only 10ng/ml (25nmol/L) in the UK and in many European countries.
100ng/ml is the high end of normal, according to the Endocrine Society. This is fine. Toxicity may be
a problem above 150 to 180ng/ml - and these levels can only occur due
to sustained (months or years) very high levels of supplementation, far
beyond what most people need to be healthy.
50ng/ml means that 1 part in 20,000,000 by weight of the blood is
25OHD. Assuming 5 litres total blood volume, and a similar
concentration in 50kg of tissue this would be 2.75 milligrams of 25OHD
in the whole body. This is the weight of a 6mm (1/4") square of
ordinary 80gsm paper.
- Some 25OHD is converted in the kidneys to 1,25-dihydoxyvitamin D
(calcitriol = 1,25OHD) which is the form of vitamin D which most
activates the vitamin D receptor [W],
a complex protein found in most types of cell. This circulating
level of 1,25OHD is tightly regulated in a system with the parathyroid
hormone and regulates calcium metabolism and bone density. This
circulating 1,25OHD is a hormone - a circulating signaling compound
which affects cells all over the body.
- For the functioning of immune system cells and other cell types,
what matters is the level of 25OHD, which is not a hormone, but is
needed and consumed by their internal signaling processes in which
1,25OHD is created inside the cell, to activate vitamin D receptors
also inside the cell. The activated receptor travels to the
nucleus where, depending on the cell type, multiple genes
are up-regulated or downregulated, so controlling the proteins
synthesized in the cell and therefore its actions.
- Some people, with
particular illnesses, such as MS (multiple sclerosis [W]) find significant
benefits from taking much more the amounts just mentioned, and with 25OHD levels well above the 40 to 60ng/ml range we are aiming for in this discussion. This
is ideally done under medical supervision, and should be done with full
knowledge of all the research, and with attention to other nutrients,
such as magnesium and vitamin K2.
- Some ill-advised people, or those who haven't properly researched the
field, think it would be a good idea to take megadoses of vitamins. Maybe
there are good arguments for this - at least for some people with particular needs. Also, with vitamin B12, it is
common and apparently safe to take doses far higher than the RDA
(Recommended Daily Allowance). Every week or so I use a B12 spray
which gives me 48,000% of the RDA. So this is 480 / 7 = 68 times the
RDA. As far as I know, this is OK.
- Unless you really know what you are doing and there are specific reasons for doing so, it is not OK to continually have a high intake
of vitamin D, except for short periods to raise your 25OHD level.
High daily intakes in the context of this guide means about 0.5mg (20,000IU) a day for normal weight people to about 0.5mg (40,000IU) or more for obese people.
According to UK government advice, the maximum allowable intake for adults of any weight, is
0.1mg (4000IU) a day. This too low, and vitamin D experts have
been arguing against it for years.
You might get away with it, but you may be harming yourself.
You might have been encouraged to do so by reckless books such as this
one:
You might have heard of megadose vitamin C being safe and beneficial
(maybe it is, for some people). If you have some sense of the
immense importance of vitamin D, you might think that more is more.
Adequate vitamin D is vital for good health, but for most people,
beyond that there's no benefit. For most people, very high
intakes over long periods are required to get levels above 150ng/ml,
which may cause hypercalcemia [W],
the most common result of vitamin D toxicity. This lowers bone
density and calcifies blood vessels, which drives heart disease.
There are valid uses of 1.25mg (50,000IU) D3 a day for long periods,
under medical supervision, for treating particular diseases, for some
people. For instance see https://sci-hub.tw/10.1016/j.jsbmb.2018.12.010
. One of the authors of this article takes 0.75mg (30,000) IU to
greatly reduce what was previously frequently debilitating asthma.
My concern is people doing this for a lark, without medical care,
especially if they have not read and understood a relevant subset of
the vast and ever-growing research literature on vitamin D.
Vitamin D, Immune System Health and COVID-19
You are reading a web page.
I am writing to you as if I am speaking to you, about your health - which I
am
genuinely concerned about, even though I don't know you. I am doing
this in an effort to make this information easy to understand, and to
impress upon you the importance of getting it right.
I know more about vitamin D, nutrition and the immune system than the
average bear, but I am not a doctor. I am an electronic technician and
computer programmer.
Ideally you would have a doctor who was up to speed with the latest
research, and able to advise you freely about all aspects of
healthcare. Below I discuss the reasons why this may not be the
case. The ideal of a fully informed doctor, examining you and
providing
personalised medical advice, is not attainable for many
people.
The purpose of this and the other pages here
../is
to help you understand more about nutrition, read the best research
and make up your own mind on how to proceed. Perhaps you will
feel
confident making your own decisions. Perhaps you will discuss it
with
other people - and ideally your doctor. Then, this and the other
pages may be an easy way he or she can find the latest research, rather
than
relying on outdated government guidelines.
There's a general reason I am concerned about your health: it would
make me happy if everyone was healthy and happy. Most
people are inadequately nourished, even with the best available food -
and almost all of us eat too much salt.
There are
two special reasons why I am concerned about your health and
the health of every other human. Both special reasons arise from the coronavirus
pandemic in which we all are at high risk of being infected with the
SARS-CoV-2 virus, leading to the disease condition COVID-19. Please see
../3-reasons/
for more details. I believe that when all things are considered,
pretty much everyone has a strong interest in most people improving
their nutrition to ensure their immune system works well, especially
with the threat of COVID-19.
Many people have no symptoms, or very mild symptoms. If this was
the case for everyone, COVID-19 would be just a nuisance.
The reason it is a
worldwide health
crisis beyond any in living memory, and the reason why whole countries
are in lockdown, with social isolation, little or no productive work or
education, reduced access to health care, cancellation of all public
gatherings etc. is solely due to the fact that
some
people suffer severe symptoms and lasting harm, and a subset of these
people are killed either directly by COVID-19, or in combination with
the impact of other illnesses.
The impact of these severe symptoms is disastrous. So are the
lockdown and other measures which are currently the only way
governments have of protecting their people from risk of harm and death.
People who think this is just like the flu are avoiding the harsh
reality of the lasting harm and deaths of people of all
ages. From babies, to adolescents, to young adults (with
COVID-19, anyone under 50 is young) to middle aged adults and
especially the elderly, death is a risk and the chance of lasting harm,
such as from organ damage due to micro-embolisms (tiny blood clots) is
much higher.
Inadequate nutrition (of which inadequate vitamin D is the most
important, best researched and easiest to fix) is already the cause of
immense and arguably disastrous suffering from a long list of illnesses
and chronic conditions most people accept as normal. These
include many cancers (the rates of which would significantly reduced
with adequate vitamin D), most neurodegeneration (dementia, Alzheimer's
disease, Parkinson's disease etc.) and numerous auto-immune diseases
(asthma, MS, Crohn's disease etc. - subject to considerable genetic
variation).
We are already in a vitamin D pandemic with profound impacts of
suffering, harm, disability and early death.
The purpose of this web page is to help you and your family and
friends
- ideally with the help of your doctor - make the best decisions about
nutrition for immune system health. But it is part of a
bigger plan to improve everyone's health. Whatever I or anyone
else seriously suggests should be done must be applicable to most
people - including those who are poor and who have no access to the
medical care we expect in Western nations.
Working with your doctor . . .
The whole of biology and is complex. The human
nutrition subset of biology is complex and the subject of ongoing research. Quite a few
questions about nutrition are contentious. This means that even
among the best experts, there is disagreement as to mechanisms, how
much of a nutrient people need, what interactions the nutrient has with
others, whether or not to supplement, how best to supplement, how best
to present this information to the public and what recommendations
should be made by government health officials.
We must recognise and cope with these controversies when learning about vitamin
D, how much to take, and what hopes we might reasonably have of it
improving our health.
There is a seemingly endless number of vitamin D research articles,
mainly concerning humans. It is hard for me to imagine how any
one person could keep up with these - even the most dedicated vitamin D
researcher. If anyone can do it, it is Henry Lahore, a
retired ex-Boeing electronics engineer, whose Vitamin D Wiki is a
prodigiously expansive repository of links to, and discussion of,
vitamin D research:
Doctors are trained in, and continue to learn, a substantial subset of
the vast and ever-expanding body of medical knowledge. They are
skilled in assessing the condition of patients, and in applying all their
knowledge and experience to improve each patient's health.
Doctors are generally trained in all the things that can go wrong
with
people's bodies, and in intervention strategies to respond to
these. They are highly trained in the use of drugs for this
purpose, but also know lots about immunisation, resuscitation, some
aspects of surgery and physical skills such as dealing with warts and
blocked ears etc. Ideally they also kind, sympathetic and get
along with all their patients - as well has understanding and being
able to help with their mental, emotional and social difficulties,
The scope of doctors' work is broader than that of any profession I
know. They have huge responsibilities and frequently very heavy
workloads.
From all I can tell - and this includes what some doctors themselves
say - doctors are generally not trained as much as they should be about
nutrition.
Furthermore, the pharmaceutical industry has an inordinate influence on
doctors initial and continuing education. Patented drugs are
constantly promoted to doctors. Drugs are promoted to patients as
well, and many patients expect their doctors to issue prescriptions for
carefully targeted drugs, with few or no side effects, which will
quickly resolve or at last contain their health problems.
Supplemental vitamin D3 (cholecalciferol) is a pharmaceutical, made from
UVB exposure of 7-dehydro-cholesterol, a cholesterol derivative usually
obtained from wool fat. However, pharmaceutical grade D3 is made
by multiple manufacturers - in recent decades primarily in China and
India, in a highly competitive market. In 1kg lots, pharma-grade
D3 costs USD$2.50 a gram, which is cheap. Furthermore,
there's not much money to be made from it, per person using it per
year, because if they took the impressive sounding 4000IU a day (the
upper limit of safety according to the advice of the UK and other
governments), this is only 1/10,000th of a gram. So the ex-factory cost of
the D3, per person, would be USD$0.09
per year.
It would be a mistake to think that people like me - who suggest that
almost everyone should be taking substantial (0.1mg a day - or 0.2mg to 0.3mg a day for
the obese) vitamin D supplements - are somehow acting in the interests of
Big Pharma.
Big Pharma has countless billions of dollars in revenue to loose if
everyone got the amount of vitamin D which maximises their health -
particularly their immune system health. Likewise the hospital
system. Likewise quite a lot of medical research industry,
which is working on apparently complex and hard-to-solve problems, such
as Alzheimers disease, which would be greatly reduced with good
nutrition - and vitamin D is the most important of these missing
nutrients.
Doctors would have a lot less work to do as well, but most would welcome this because they really want their patients to thrive.
Since medicine is a very well researched field, most doctors are not
solving fresh problems every day. Their primary task is to arrive
at a correct diagnosis and to choose the best intervention - which is
frequently thought to involve drugs or perhaps surgery. Some conditions
are difficult to clearly diagnose, and some diagnostic categories and
the best ways of tackling them are the subject of ongoing debate.
(For instance, fats, statins and heart disease; fibromyaligia.)
In the vast scope of their work, vitamin D is a relatively small
sub-field - except for those doctors who have gone to special trouble
to study it. These doctors will recommend D3 supplementation in
line with the latest research, and may want to test their patients'
25OHD levels once a year to see that it is within the fairly broad
target range - ideally
40 to 60ng/ml, with levels up to 100 to perhaps
150mg a cause for reducing the dose, and not for alarm. For
instance, see what one such doctor wrote about levels and dosing:
../#2020-Baker-a
.
I don't have a list of doctor who take a special interest in nutrition
and especially vitamin D. Here are the websites of two:
Most doctors have no time to read the latest vitamin D research.
I don't think there are enough hours in the day for even the keenest vitamin D researchers to read it all.
Most doctors rely on clinical guidelines which are perhaps a decade or more out
of step with current research. There is a great deal of
debate about these guidelines, and it seems that the committees which
set them are subject to numerous pressures and are reluctant to alter
their recommendations significantly, since this would be an admission
that their critics, over the years, were
right.
For some background on the decades-old debate about vitamin D, please see this extensive article by
William B. Grant
(PhD, physics) who has written peer-reviewed journal articles
concerning UVB, vitamin D, cancer and Alzheimer's disease.
He is one of the 48 researchers and MDs at
GrassrootsHealth.net who since 2008 have advocated
40 to 60ng/ml as the target range for 25OHD.
As in any field, I have seen research I consider sound and some not so under the banner: "orthomolecular". It means [
W]
maintaining health through nutritional supplementation - "the
right molecules in the right amounts" - which is a perfectly good
principle.
Doctors operate under a variety of difficulties which tend to make
their treatment decisions more likely to accord with established
guidelines, rather than with the best research. These include:
- They are not aware of the latest research.
- They may be required to abide by government or professional
association guidelines, by their employer - or be similarly constrained
by fear of not being covered by malpractice insurance if something goes
wrong and a patient decides to sue them. (I think this threat is
much worse in the USA than in most other countries.)
- They may want some time to pass for the latest research to be
corroborated, or at least regarded as being substantial, before basing
treatment decisions on it. (In software, the latest version of a
program may well have bugs and deficiencies compared to the previous
version.)
- Even if they have read recent research which is at odds with
guidelines they are supposed to follow, they may be very wary of
stepping outside the guidelines if this is what most other doctors in
their country are following.
Especially in the age of social media blood sport Colosseum-like venues
such as Twitter - where the twit mob can have a person convicted,
tarred and feathered for all the world to see (and find forever via
search engines, even if the mob eventually changes its mind), even
without substantial evidence, in hours or days - doctors are wary of
being perceived as controversial. There's a long line of "vitamin
megadose" stories. While some of them concern matters of
substance and genuine scientific interest, doctors are at pains to
avoid any association with the reckless end of this genre - and there's
a lot of it in popular books, blogs etc. See the abovementioned
book by Jeff T. Bowles.
The ability of a doctor to remain employed in his or her profession
depends very much on avoiding any such controversy - anything which
might make someone think of a word beginning with 'q' and which should
not be uttered within 50 metres of any good doctor.
- When working on a team, such as in an ICU, the team approach to
diagnosis and treatment may be explicitly defined by documents which
one doctor - or even the whole team - cannot alter or deviate from.
- Especially in the USA, doctors may be constrained in their
treatment options by what insurance companies regard as legitimate and
cost-effective.
- Fear of being sued - especially in the USA - may weigh heavily on
the minds of doctors, including the fear that their insurance company
would not defend any action they took which was outside the range
allowed by government or professional association guidelines.
There is an information chain with numerous delays and
distortions. A discovery is made. It takes time to
write it up in an academic article and have it peer reviewed and
published. Ideally, over months and years, other people read it,
cite it and perhaps replicate it, with similarly published
research. Then, perhaps, one or more of these articles will be
included in a review article, in which, perhaps, the conclusion of the
review article is changed towards the clinical implications of the new
(by now a few years old) research. Then, if there are a few
such review articles, some doctors will discuss it in a forum or
conference, and many of them will say they will wait for a randomized
controlled trial (RCT) - or two - to be performed showing that the
potential new treatment approach will be helpful to their patients, if
applied as intended, without significant ill-effects. (Such
caution is reasonable in the case of novel drugs being pushed by
pharmaceutical companies, where the ill-effects are likely to be
unknown without years of extensive testing or clinical use.)
So over the next few years, with luck, some good souls may get the
funding (such as millions of dollars) to employ themselves for another
year or two to run the RCT. (Though some RCTs take 5 or 10
years.) Eventually, if the RCT is done well, and the
desired benefit is shown to be significant (useful and unlikely to have
occurred by chance) then someone will want a second RCT just to be sure
. . . .
All the above is true of patented high-profit single-manufacturer
drugs, generic drugs and naturally occurring, if manufactured,
nutrients. In the case of patented drugs, the drug company
will invest the money to run the trials and they will be done
ASAP. For generic drugs and nutrients, the only source of funding
is government agencies or philanthropic funds - so it is very much
harder to fund expensive research into these.
Years later, a committee meets to revise its now 5 or 10 year old
guidelines. Maybe it will be persuaded by the RCT results, as
found to be good by one or more subsequent review papers, that its
earlier guidelines were wrong and so need to be changed significantly.
If they do this, it takes time for their conclusions to be published,
and then time for anyone to take much notice, such as a second
committee in another country which sets guidelines in part based on
those which have just been changed. Then, some years later,
the guidelines for that country may be changed, and over the next few
years, with luck, the doctors in those countries will begin to base
their treatment decisions on the "new" guidelines.
Meanwhile, patients are not benefiting from the best research.
There are good reasons for caution in medicine. There are
examples in history of treatment decisions being made according to
new information which did not, in the long run, turn out to be accurate.
However, what if the current guidelines are just plain wrong?
Exhibit A is the UK government guidelines that 10ng/ml 25OHD is
sufficient, and that most people should take 0.01mg (400IU) vitamin D -
and then perhaps only in winter. For a recent article which
defended these awful, deadly, harm-causing standards, see:
which I discuss further at
../#21authors
. Likewise the UK NICE report, which found no reason to
think that low vitamin D levels had anything to do with COVID-19 severe
symptoms:
https://www.nice.org.uk/advice/es28/evidence , critique:
http://www.drdavidgrimes.com/2020/07/covid-19-and-vitamin-d-uk-nice-r.html .
Upon the publication of the above article and the NICE report two
months later, newspapers, news sites etc. all over the world lit up
with headlines to the effect that vitamin D supplementation will be no
use in preventing COVID-19 infection (largely true) or reducing the risk of severe symptoms (disastrously false, I am
sure). Some people it is smart to dismiss what
they think is a flaky, overly simple, attempt at solving a very complex
and serious problem. They are ill-informed: nutritional
deficiencies can and do cause vastly complex, pervasive and seemingly
complex patterns of ill-health. It is not surprising, considering
the complexity of a single cell, and of an entire human body and the
hundreds of species of bacteria it hosts.
So there are numerous reasons why reality, as discovered by competent
researchers, takes a very long time to influence clinical practice for
the better, for
most
doctors. However, some are much more attuned to what is
actually happening, and will adapt their treatment and advice to the
public much more rapidly.
There is an extraordinarily strong
herd mentality among medical
practitioners. It took about 30 years before hand washing
was widely accepted as being necessary:
https://www.nationalgeographic.com/history/2020/03/handwashing-once-controversial-medical-advice/
The same applies now, with excellent work by doctors, such as Dr Paul Marik
../icu/#Marik-protocol who
found intravenous vitamin C in combination with anti-inflammatory
corticosteroids saves many ICU patients. This is not
surprising, given the importance of vitamin C to the immune system, and
the well known fact that it is drastically depleted, to the point of
being impossible to detect, in many ICU patients, especially those with
sepsis. Years later, many doctors are still reluctant to replete
this missing vitamin C the way he does, wanting RCTs etc. which Paul
Marik will not do, because it would involve denying life-saving treatment to half
his patients. (I think he would do better still with rapid, bolus
dose, 250HD vitamin D repletion.)
I am one of a growing number of people, including MDs, who believe that
the only way the current COVID-19 crisis can be resolved is a massive
program of nutritional supplementation to improve everyone's immune
system health. Vitamin D is the obvious choice.
Meanwhile most doctors haven't really thought about this. Pretty much everyone assumes the solution must be in avoiding
infection until everyone can be protected by a magic
vaccine.
In enquiring into vitamin D supplementation, you can't avoid
recognising the divergent views among MDs and other healthcare
professionals.
In 2016, my doctor told me straight that my 0.1mg D3 a day was
too much - that I was risking vitamin D toxicity. We discussed it
as "4000IU", which sounds so much more, perhaps scarily more. I
knew then that he was wrong. Now I know more about it, I take
about 0.175mg a day. I would probably be OK with the old
amount. But not knowing my 25OHD levels (I haven't needed
to see a doctor since then, and I am 64) maybe I would be better off
with more. I could double this again with zero risk of
toxicity.
Ideally, everyone would have easy,
affordable, access to a doctor whose knowledge of vitamin D and of
nutrition in general was up to date with the best, recent,
research.
Ideally everyone would follow their
advice, and perhaps get their vitamin D blood levels checked every year
or two, or five.
Most people's immune system would work much better than they do today
(especially if they ate less salt, more omega 3 fats and supplemented
with vitamin C, potassium and boron). I believe that if everyone in the
world had adequate vitamin D, there would be much less ill-health,
COVID-19 would be a minor nuisance except in very rare instances, there would no lockdowns and
I would be designing and building electronic musical instruments rather
than writing this web page.
If you can find a good - vitamin D nutrition aware - doctor, get your
25OHD levels tested and proceed from there, then there's no need to
read any further.
However, writing in early August 2020 (1.1 million new confirmed
COVID-19 cases in the last four days), who wants to go to a doctor's
office? Or sit in the waiting room of a pathology office to
have your blood drawn? No-one in their right mind would want to do this unless
they have a medical condition which is likely worse than the risk of
contracting COVID-19 from the other people in those rooms.
Not everyone can afford to see a doctor. I am writing not
just for people in the developed West - though many people in the West
can't afford to it either. I am writing for people in all countries - and
in many parts of the world, doctors are few and far between, distant,
and/or unaffordable. Likewise pathology labs and 25OHD tests.
. . . or without a personal doctor
Even if all doctors were up-to-speed on
vitamin D and nutrition in general, and even if they were nearby, could
be visited without risk of catching COVID-19, and were affordable,
there are not enough of them to cope with the world's population
turning up for consultations, 25OHD tests, individual advice on D3
supplementation etc. in the next few months - prompted by the severe
test of their immune system health which will occur if and when they contract COVID-19.
By necessity or choice, most people will be trying to decide about vitamin D
supplementation without the personalised assistance of doctors.
Fortunately, it is not hard to do. There is a wide range between
the D3 intakes which will most likely ensure adequate (at least
40ng/ml, for most people) 25OHD levels and those which would cause
toxicity. While toxicity may be a problem above, say,
160ng/ml - a factor of 4 - there is a much wider range of safe dosages,
because raising the 25OHD level a factor of 4 can only occur after
months of taking a very much larger amount (much greater than a factor
of 4) than whatever it takes, in general, to reach 40ng/ml. The
recommendation of the research cited below is a target range of
40 to 60ng/ml, with not
too much fuss if it goes above this, and with recognition than for a
few people (unless monitored with blood tests) a somewhat lower level
will result.
There are peer-reviewed journal articles which present good research -
or reviews of the research first reported in other articles - written
by highly regarded doctors who are also highly regarded vitamin D
researchers.
The first article I cite below is co-written by PhD endocrinologist and MD
Michael J Holick [
W]
http://drholick.com who,
since 1971 - when he identified for the first time several
forms of vitamin D in the body - has become the world's best known
vitamin D researcher. You may encounter a 2018 hatchet job
article about him in the New York Times, by Liz Szabo. For the
background to this, and the critical letters to the editor from other
researchers and MDs the NYT never published, see the above article by
William B. Grant. Google Scholar lists 129,482
citations for articles Dr Holick wrote or co-wrote.
D3 supplementation, body weight and long-term 25OHD levels - aiming for 40 to 60ng/ml
If you are keen to raise your vitamin D
levels rapidly - as seems reasonable if you have not been supplementing
and you are concerned about getting COVID-19 soon - then please see the
next section after reading this one.
The aim of this section is to enable you, or your doctor, to estimate
the amount of supplemental vitamin D you should take to aim for the 40 to 60ng/ml target range recommended in some research articles cited below.
This assumes that you get little vitamin D from food, unprotected UVB
light exposure, multivitamins or other supplement tablets. If you
are taking significant numbers of calcium tablets (citrate is
more bioavailable than most other kinds) then these may have vitamin D3
added, so take that into account.
This is not a particularly exact process, since 25OHD levels vary quite
a lot between people with the same supplemental intake. Fortunately, for most people - those without COVID-19 predisposing
conditions such as advanced age or being overweight or obese -
there's a large gap between what should do the trick in terms of good
health and the much higher amount of supplements which would cause
toxicity.
Your doctor might want to be more fussy. If you have a doctor,
and can experiment with dosages and 25OHD levels over months and years,
then you don't really need the chart below.
For now we assume we are aiming for about 50ng/ml 25OHD - but below I have some ideas (from an electronic technician - not a doctor) about why some people should aim higher.
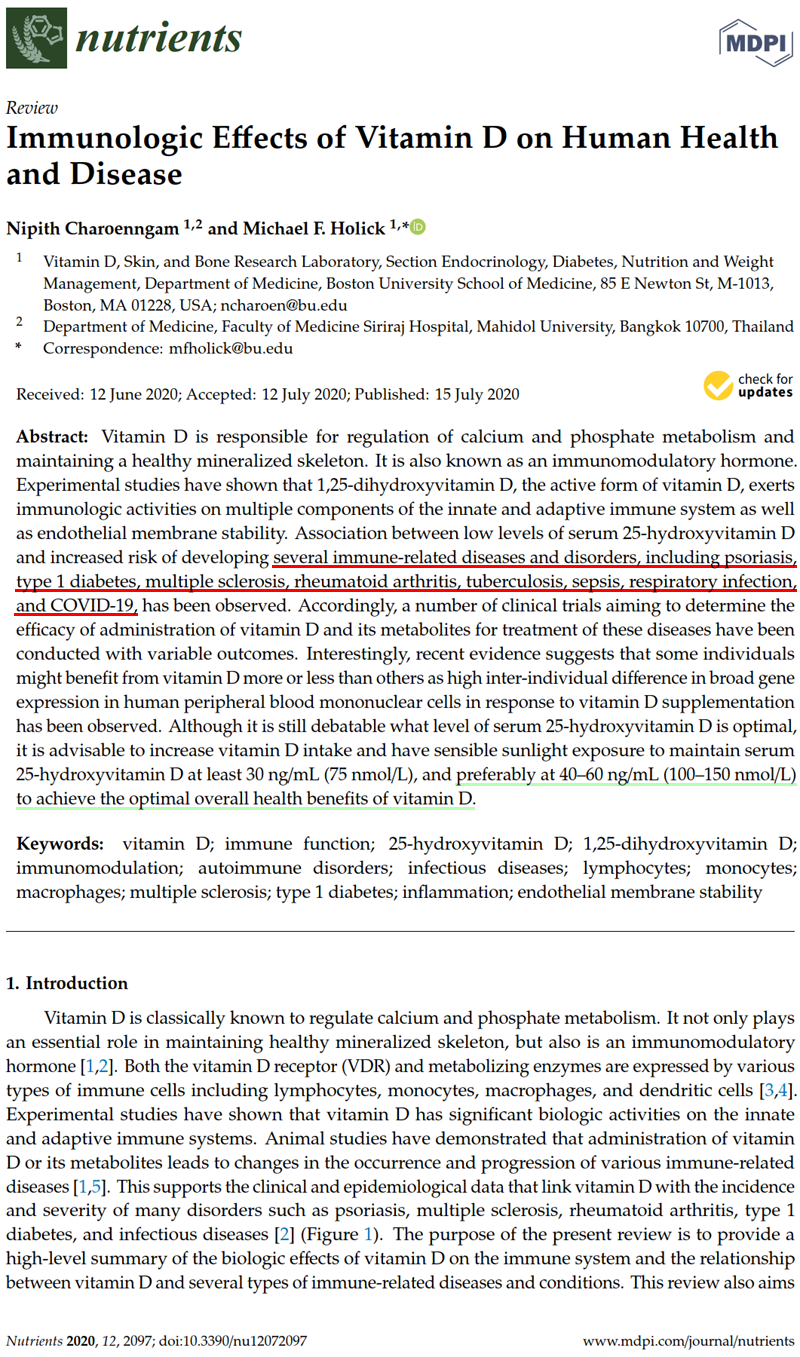
The most recent review article concerning immune system health and
vitamin D just two weeks old as I write this in early August 2020::
Immunologic Effects of Vitamin D on Human Health and Disease
Nipith Charoenngam, Michael F. Holick 2020-07-15
Nutrients 2020, 12(7), 2097 https://doi.org/10.3390/nu12072097
|
Another recent article which makes the same recommendation is:
Editorial – Vitamin D status: a key modulator of innate immunity and natural defense from acute viral respiratory infections
A. Fabbri, M. Infante, C. Ricordi Eur Rev Med Pharmacol Sci 2020; 24 (7): 4048-4052 2020-04-05
https://www.europeanreview.org/article/20876
|
We also believe that maintenance of circulating 25-hydroxyvitamin D levels of 40 - 60ng/ml would be optimal, since it has been suggested that concentrations amounting to 40ng/ml represent the beginning point of the plateau where the synthesis of the active form calcitriol becomes substrate-independent [2011-Hollis err] [2018-Wagner].
|
This last point refers to the
efficiency with which 1,25OHD (calcitriol) is produced inside cells,
such as lymphocytes, as part of their internal, autocrine [
W],
signaling system. This system is required for the cells to
respond properly to conditions, such as turning on direct anti-viral
attack chemicals when they are needed, and turning them off (or
signaling to other lymphocytes to turn off theirs) when they are no
longer needed and instead are hyper-inflammatory, and so
self-destructive.
In biochemistry, the original state of a molecule which an enzyme
modifies is called the "substrate". 1,25OHD is the form of
vitamin D which activates vitamin D receptors.
In this autocrine signaling system an enzyme works on a molecule of
25OHD and attaches an OH group to the 1 position, and so converts
it into 1,25OHD. The enzyme ejects this and then
waits for another 25OHD molecule to fall into position so it can repeat
the process. (The enzyme is a catalyst which is not changed by this operation. Other molecules are
consumed in providing the OH group and the required energy.)
The 25OHD level (as measured in blood tests) in the blood and so the
interstitial fluid in which all cells operate, sets the concentration
of 25OHD inside the cells where this enzyme operates. Below a
certain level (very approximately 40ng/ml), this reduces the ability of
the enzyme molecules to stay busy and produce 1,25OHD. So A. Fabbri et al.
are saying that if your 25OHD levels are
40 to 60ng/ml,
then this will be the concentration in the immune cells, and their
internal signaling will work properly, due to the process not being
slowed down due to inadequate supplies of 25OHD.
Now look at the graph on the main page
../#2020-UK-vit-D-BAME
of the appallingly low 25OHD levels of many people in the UK, in
winter. Even in summer, white people on average only reach
25ng/ml for a month or so before dropping back to
16ng/ml in mid-winter. Black, Asian and Ethnic Minority people's average levels vary from
10 to 15ng/ml all year round. See also
../#SAAD where we see that in the UK, 44% of South Asian women (from India, Pakistan and Bangladesh) average, year round
less than 6ng/ml!
Also see, on the icu page, this article
../icu/#2020-McGregor
, which reports that lymphocytes removed from the lungs of hospitalised
COVID-19 patients remained in their hyper-inflammatory state,
not progressing to their anti-inflammatory shut-down phase,
due entirely to lack of 25OHD
preventing their autocrine signaling system from working. Yet the
system worked fine in the same kinds of lymphocytes from healthy
control subjects.
(The first thing I wanted to know was the 25OHD levels of the COVID-19 patients and of the healthy
controls. I wrote a comment to their article asking if this was available.)
Are we connecting the dots boys and girls? Its not that hard. I figured this out in March: that the patient's
low
vitamin D is a major contributing cause of the dysregulated,
hyper-inflammatory, immune response which drives COVID-19
hypercoagulation - and sepsis, and influenza-pneumonia.
Just in, 2020-08-02: An ICU doctor
says :
"A lot of COVID patients who require hospitalization do have low vitamin
D levels," he says, but is quick to add that correlation does not equal
causation. "Does that mean we should give every hospitalized COVID
patient big doses of vitamin D when they hit the door? Maybe."
He would be upset if he brought some item of equipment to me and I
found its +/- 12 volt power supply lines were sagging and fluctuating
around 7 volts or so, and I handed it back to him, with an invoice, and
said: "The power rails are drooping. Maybe the circuit is drawing
too much current - so the power supply is OK. Maybe the circuit
is OK and the power supply needs to be fixed. Here you are.".
What is wrong with so many doctors?? This is the most perplexing thing!
As an electronic technician with a cursory understanding of vitamin D's
role in the immune system, it was obvious. However, it seems that
most doctors' minds are filled with thoughts of drugs and vaccines, and
of unprecedented global disaster, the need for RCTs before doing
anything at all novel . . . and are not attuned to the kind of
fault-finding detective work for novel problems which is a normal part
of electronic work. Despite hundreds of articles on low vitamin D
and dysregulated immune responses (and some on omega 3s and boron too),
most doctors still cannot properly imagine what harm results from
inadequate vitamin D.
Additionally, serum 25-hydroxyvitamin D levels of approximately greater than or equal to 40ng/ml
could* provide protection against acute viral respiratory infections, as
demonstrated in a prospective cohort study published in PLoS One and
conducted on 198 healthy adults [2020-Sabetta]. To reach these concentrations in adults, a dietary and/or supplemental intake of vitamin D up to 6000 IU/day
(0.15mg) – deemed to be safe – is required.
However, elderly subjects,
overweight/obese and diabetic patients, patients with malabsorption
syndromes**, and patients on medications affecting vitamin D metabolism may require even higher doses under medical supervision.
|
* In
the research article vernacular, "could" and "may" frequently mean "we
really think it will, but we can't prove it beyond reasonable doubt and
we don't want to look overly confident".
However they boldly use "is" later in the paragraph when they are very sure of themselves.
**
See below on Roux-en-Y and other weight-loss bariatric surgeries, many
of which are specifically designed to reduce fat absorption, and so
will reduce vitamin D3 absorption.
In sunny Africa one might think there's
no vitamin D deficiency, but most people wisely stay out of the sun,
and with very dark skin, don't make much vitamin D from the small
amount of direct sunlight they do get. So vitamin D deficiency is
a problem there too. Without reference to desired 25OHD levels,
Dr David Ajibade of the Nigerian based Brain and Body Foundation (
bio) stated, on 2020-07-25 in an
interview :
In
my opinion, the best way for black people to get adequate levels of
vitamin D is by supplementation. And the research shows that adults
should be getting no less than 10,000IU (0.25mg) a day.
In my opinion, the best
way for black people to get adequate levels of vitamin D is by
supplementation. And the research shows that adults should be getting no
less than 10,000 IUs a day.
Read more at:
https://www.vanguardngr.com/2020/07/vitamin-d-crucial-in-management-of-covid-19-sickle-cell-disorders-dr-david-ajibade/
In my opinion, the best
way for black people to get adequate levels of vitamin D is by
supplementation. And the research shows that adults should be getting no
less than 10,000 IUs a day. Read more at:
https://www.vanguardngr.com/2020/07/vitamin-d-crucial-in-management-of-covid-19-sickle-cell-disorders-dr-david-ajibade/
In my opinion, the best
way for black people to get adequate levels of vitamin D is by
supplementation. And the research shows that adults should be getting no
less than 10,000 IUs a day.
Read more at:
https://www.vanguardngr.com/2020/07/vitamin-d-crucial-in-management-of-covid-19-sickle-cell-disorders-dr-david-ajibade/
|
Finally, 48 vitamin D researchers and MDs (some are both) have been saying the same thing about
40 to 60ng/ml since 2008, with their Call to D*action for Public Health:
https://www.grassrootshealth.net/project/our-scientists/ . These include Michael Holick.
Here is the vitamin D intake vs. 25OHD by body weight chart and the
article which from which it was adapted. I added the text, the
ng/ml and milligram scales, the dots and the green target zone.
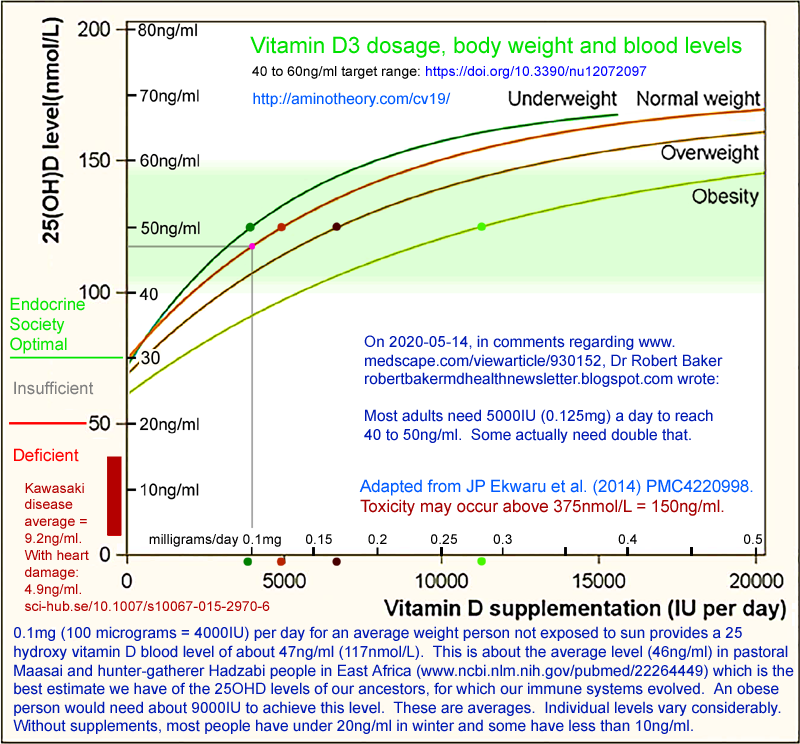
The 17,614 adult subjects in this research study mainly lived in Alberta, Canada, at latitudes of 49 to 60° north.
| We recommend vitamin D supplementation be 2 to 3 times higher for obese
subjects and 1.5 times higher for overweight subjects relative to normal
weight subjects. |
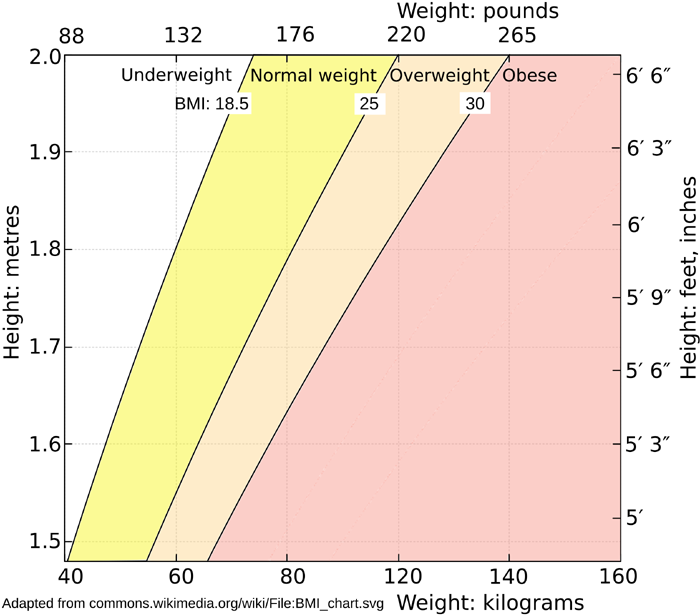
Here is a BMI (Body Mass Index [
W]) chart (
SVG file):
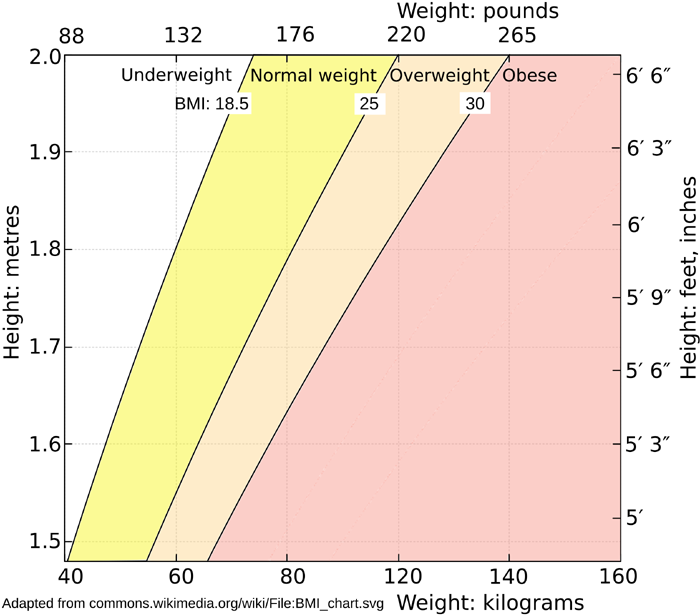
Sidebar on problems inherent in using BMI like this:
There are numerous critiques of the whole concept of Body Mass Index (BMI): Google: BMI controversy for various websites, academic articles etc. such as this and this.
I think it is best to recognise that the average height of male and
female Canadians is 1.75 and 1.62 metres respectively, so the four
curves were probably derived mainly from people in the 1.55 to 1.8
metre height range.
The two primary things we need to account for in increasing the
supplemental D3 intake above that of average weight and average height
people is that some people are heavier (the first multiplier) and
- independently of this - some people have a greater proportion of
their body weight as adipose tissue.
I just want to flag that this is not ideal. If I devised what
looks to me like a better chart to convert height and weight into a
daily D3 supplemental quantity, the result would not be based directly
on the best available peer-reviewed research articles - which is what I
want to achieve.
From the Ekwaru et al. graph it is easy to see vitamin D3 daily intake
rates which will, most likely, on average, achieve the 50ng/ml 25OHD level, in the middle of the target range
40 to 60ng/ml, for the four ranges of BMI are:
Body weight
|
BMI
|
Daily vitamin D3
supplement
milligrams
|
IU
|
Underweight
|
< 18.5
|
0.1mg
|
4,000
|
Normal
|
18.5 - 25 |
0.125mg
|
5,000
|
Overweight
|
25 - 30
|
0.175mg
|
7,000
|
Obesity
|
> 30
|
0.3mg
|
12,000
|
While this is statistically reasonably valid, each person's final 25OHD
is likely to vary quite a lot, so there's no point in fussing about
exact doses down to 10% accuracy.
The first thing people are going to think when looking at this and their bottle of 0.025mg (1000IU) vitamin D capsules is:
How much is this going to cost?
and the second is:
Do I really have to swallow so many capsules?
At a pinch, to start with, use whatever vitamin D3 (or even D2) you
have. For the longer term, it is a cheaper and more
convenient to use capsules with larger amounts of vitamin D.
It is relatively easy to get 0.12mg (5000IU) capsules - though in
Australia, try eBay or Amazon, since ordinary shops are not allowed to sell
capsules with more than 0.025mg = 1000IU.
Since it takes a week or so for most of the ingested D3 to be converted by the
liver into circulating 25OHD, and since the half-life of the 25OHD is
generally much longer than this, then there is no need to take
vitamin D supplements every day, or probably every week. Two
weeks between taking supplemental D3 is probably fine. I have an
article here somewhere on the half-life decreasing at higher
levels. The self-regulatory system for 25OHD changes some of it
into 24,25OHD, at a rate which scales with the 25OHD level.
My wife Tina and I have been using
1.25mg (50,000IU) D3 capsules for a few years:
These are a dry powder in a small capsule and cost USD$30 per 100, so USD$0.24 per milligram.
0.25mg (10,000IU) capsules are available from several companies, such as:
120 for USD$17 = USD$0.57 per milligram. This one is a "softgel"
capsule, with the D3 dissolved in olive oil. I guess this makes
it more bioavailable than in a dry form.
0.125mg (5000IU) olive oil capsules are also available:
240 for USD$23 = USD$0.77 per milligram.
Here's a table for the three different sizes of D3 capsule, at various
intervals, with the resulting average daily dose. The first one
would be pretty close to 0.1mg (4000IU) a day with a small amount of D3
from a multivitamin.
0.125mg
5000IU
|
0.25mg
10,000IU
|
1.25mg (50,000IU)
|
mg /day
| IU/day
|
|
|
1 / 2 weeks
|
0.089
|
3,571
|
|
1 Mon, Tue,
Wed
|
|
0.107
|
4,286
|
1 / 1 day
|
1 / 2 days
|
1 / 10 days
e.g. 1st, 10th & 20th
of the month.
|
0.125
| 5,000
|
1 Mon - Fri,
2 Sat & Sun
|
|
|
0.161
| 6,428
|
2 Mon - Fri
|
1 Mon - Fri
|
1 / week
|
0.179
| 7,142
|
2 Mon - Sat
|
1 Mon - Sat
|
|
0.214
| 8,571
|
2 / day
|
1 / day
|
6 / month
e.g. 1st, 6th, 12th,
18th, 24th & 30th
of the month.
|
0.250
|
10,000
|
|
1 Mon - Fri,
2 Sat & Sun |
|
0.321
|
12,857
|
|
2 Mon - Fri
|
1 Mon & Fri
|
0.357
|
14,286
|
It would be nice if we could get our
25OHD levels over some threshold, such as 40ng/ml, know this from
testing, and then be confident that COVID-19 would not cause us any
serious trouble. The situation is more
complex. Vitamin D levels are a very important thing we can and
should raise, but there are numerous factors at work, and it is
reasonable to expect that
some
people will suffer harm and be killed even if their 24OHD levels are
above 40ng/ml. Please see the chart of levels and ages from
the Iranian research study at:
../#2020-Maghbooli .
Obesity itself (irrespective of
other conditions, including vitamin D deficiency - though without
supplements it is safe to assume that obese people have very low
vitamin D)
presents a very high risk for COVID-19 serious harm and death. Some of the currently known mechanisms are mentioned in the research articles listed here:
../obesity/
. Everyone knows that most people who are harmed and killed by
COVID-19 are either 70, 80 or 90+ years old, or obese. There are
other risk factors such as diabetes and lung injury.
Some people with a particular genetic pattern (haplotype) on chromosome
3 are also at a high risk of COVID-19 severe symptoms. This is
rare in Africans, common in Europeans and, apparently, most prevalent
in Bangadeshis. See:
../#haplotypes
. This is a particular concern for Bangladeshis living in
the UK, far from the sun, with such low levels in the official guidance
for vitamin D supplementation and proper 25OHD levels.
My opinion as an electronic technician:
If I or a loved one was obese, or of
advanced years like this, and/or known or likely to have some other
risk factor, I would be inclined to err on the high side of these
dosages. Adding another 30% or 50% so is not going to get anyone
close to the 150ng/ml where toxicity might be
a problem - and there's a good chance that the the higher 25OHD level
resulting from the larger intake will make a crucial difference when
their immune
system is really put to the test by COVID-19.
Pregnant women
need vitamin D3 like anyone else, but it is much more important that
they get it than anyone else, because their baby's body building
itself.
We are used to complex products emerging from even more complex
factories, but biology builds itself, and problems in prenatal and
early childhood development are likely to last a lifetime.
It is well known that pregnant women should never smoke or use
alcohol. It should be better known that they need vitamin D
supplementation (unless perhaps they get a lot of sun exposure) and to
be replete in all other nutrients.
VitaminDWiki has hundreds of pages concerning pregnancy. Here are
some links on vitamin D deficiency contributing to the risk of
premature birth ,
preeclampsia ,
ADHD and
autism .
Babies and children need
vitamin D supplements too. As long as Baby is breastfeeding
substantially and Mother is vitamin D replete, there is no need for
supplemental D3.
There are various guidelines for supplementing children, but they may
be based on 25OHD levels lower than the
40 to 60ng/ml we are aiming for
here. It seems logical that supplemental doses could be
worked out from the baby's or child's weight as a fraction of the 70 kg
or so weight of an average weight adult, and the 0.125ng (5000IU) a day
amount mentioned above.
Some adults have
reduced fat absorption and other
reductions in nutrient absorption. This is certainly the case for anyone who has had
Roux-En-Y [
W] gastric bypass surgery [
W] [
DW],
which is specifically intended to reduce fat absorption. The
stomach is turned into a pouch there is no stomach sphincter or initial
part of the intestine, where a great deal of nutrient absorption takes
place. Food may rush through the system, without the stomach
sphincter to regulate its flow. In the USA, Roux-En-Y is a common
form of weight loss
surgery. Roux-En-Y patients must supplement with B12 to avoid
brain damage, and require special attention to other nutrients such as
iron.
Roux-En-Y is the most disruptive of several gastric bypass
surgeries. According to this article, which concerns gastric
bypass surgeries in general:
bone loss remains a problem even with "normal" levels of 25OHD. They state:
The results seen in this study suggest that in individuals who have had
gastric bypass surgery it may be necessary to maintain the 25(OH)D3
status of 40 to 80 ng/mL
recommended by the Vitamin D Council, together with a calcium intake of
1300 mg/day, which is the upper recommended daily intake (RDI)
suggested for postmenopausal women. Calcium intake of 1500 mg/day as
calcium citrate is now recommended in the 2014 position statement of
the American Society for Metabolic and Bariatric Surgery.
|
Assuming this was for weight loss, these people are likely still to be
overweight or obese, but hopefully no longer morbidly obese, have
an unknown deficiency in vitamin D absorption, and we are aiming not
for 40 to 60ng/ml but 40 to 80ng/ml. We see from the graph
that higher 25OHD levels become progressively harder to attain.
All these people should be under the medical supervision of doctors who
specialise in the nutritional requirements and other health problems
resulting from these surgeries. This article looks good, but it
is aiming for only 30ng/ml 25OHD:
I haven't found any clear guidance on this, but assuming a person is
overweight or borderline obese, and has had Roux-En-Y surgery, here are
the reasons I think they need higher D3 intakes than the 0.125mg
(5000IU) required (on average) for a normal weight person to attain
50ng/ml:
- They have extra adipocytes and so need more supplemental D3. (So double the intake at least, as per the graph above.)
- They are at high risk of COVID-19 severe symptoms. (So aim
for higher than 50ng/ml - double the intake again, I think. Also,
see above for a target range up to 80ng/ml above.)
- Their ability to absorb oral vitamin D is compromised to some unknown factor. (Double it again, I guess.)
On that basis, depending on the person's actual weight (a short person
with a BMI of 30 weighs less than a tall person with this) . . . and
again remembering you are reading the musing of an electronic
technician . . . it looks like giving them 8 times the normal D3
intake would make sense: 1.00mg = 40,000IU. This
seems like a lot, and ideally there would be medical supervision with
blood tests and aiming for at least 50ng/ml (see above for 80ng/ml) -
but these people face numerous health challenges and it may make good
sense for them to take quantities of vitamin D3 which would quite
likely lead to toxicity in a normal-weight person with no such
surgery, but which pose no such danger for their larger bodies.
Stomach banding does not involve such malabsorption as Roux-En-Y.
There are too many variables here to warrant more detailed speculation.
Bolus (loading) doses to raise 25OHD levels quickly
No-one should take 1.25mg (50,000IU) capsules once a day for long periods.
Recently I spoke by phone to a musical instrument customer in
Europe. After listening to my obligatory vitamin D pep-talk he
told me that he was going to quite some trouble to use supplements
to improve his health. He is educated, in his 30s, average
weight, thriving
and reasonably knowledgeable about nutrition.
However . . . he had been taking a 12.5mg (50,000IU) capsule once a day
for a year!
As far as we know it hasn't done him any harm, but he would probably have some
ridiculous 25OHD level and that this may have caused calcification of
his blood vessels, which results from hypercalcemia. This
takes months, but drives heart disease.
Don't do this!
I immediately thought of
PMC6334045/
which reports on a 73 year old retired nuclear physicist who took 1.5mg
(60,000IU) D3 a day for two years. He had no previous health
problems and did not smoke or drink etc. He got to 352ng/ml
25OHD, and had profound cognitive problems, including being confused
and drowsy. These and other symptoms including hypercalcemia
resolved after he stopped the supplements.
However, it is fine to take high doses of D3 for a short period of
time, since it takes a week or so to build up the 25OHD levels in the
bloodstream to healthy levels and much longer to reach dangerous levels
above 150ng/ml.
In early August 2020, with a quarter million verified new cases of
COVID-19 a day worldwide, it is reasonable to expect that we are going
to get the virus pretty soon. So - especially for the elderly or
the obese - I think it is a good idea to start supplementation with
higher doses to raise 25OHD levels to the desired 40 to 60ng/ml range
ASAP.
In Newcastle upon Tyne, in the far north of England, with predominantly white hospitalised COVID-19 patients, doctors
../#2020-Panagiotou are starting some of them on bolus doses of up to
5mg (300,000IU) of D3 on admission.
They only did this for patients with disastrously low vitamin D levels:
5.2ng/ml or less, with lower bolus doses for higher levels. I
think they should have had higher thresholds and much higher
maintenance doses.
There's something odd about UK doctors and vitamin D - it is as if they are
dealing out crack,
worrying about something terrible happening, as if the vitamin D
toxicity bogey man is just around the corner. Part of the reason
for this is probably the UK government's ridiculously low standard of
10ng/ml for being vitamin D replete. Another may be that in the
UK they use nmol/L (nanomols - a number of molecules - per Litre) for
25OHD levels, which are 2.5 times the ng/ml figures.
So to them,
40 to 60ng/ml may seem scarily high at 100 to 150nmol/L, when the population all-year-round average is less than
20ng/ml (50nmol/L).
In this section of the main page :
../#03-vit-d
is a link to an article describing a double-blind randomised controlled
trial - the highest standard of evidence in medicine. It
concerned ICU patients who needed mechanical ventilation for a variety
of illnesses and were on average overweight to obese. The control
group got out of hospital, on average, after
36 days. Those who received
1.25mg D3 (50,000IU) a day for five days = 6.25mg (250,000IU) got out, on average, after
25 days. Those who received
2.5mg D3 (100,000IU) a day for five days got out on average after
11 days.
These initial high doses were, on average, beneficial - and there were
no adverse outcomes. However, people in ICU might not be
absorbing the D3 very well.
Scaling back the higher of these doses (12.5mg = 500,000IU) total to
normal weight people, and assuming good absorption, I
guess
5mg (200,000IU) is probably a good way to start, over a day or several days.
Here are my thoughts as electronic technician of how I would respond in a disastrous situation where medical care was unavailable,
such as due to the hospitals being totally overloaded and all the
doctors and nurses either sick with the virus or working unsustainably
to help other people. The price of these
thoughts is $0.00 with a money back guarantee:
If
I, or some adult in my care, was suspected or known to have COVID-19,
and was reasonably assumed to have low vitamin D, due to no
supplementation beyond perhaps multivitamins, in the absence of any
well informed medical advice, I would give them, to start with, for
instance:
- 50 or younger, average weight: 3.75mg (150,000IU) D3.
- 70+ or obese: twice this.
It is impossible to give
someone vitamin D toxicity with intakes such as this for a short
period. There would be unknown unknowns - but with the risk of
COVID-19 severe symptoms, lasting harm and death bearing down on them
like a freight train, I would do all I could to get their 25OHD levels
up to 40 to 60ng/ml ASAP, or ideally higher for someone who was obese,
elderly or facing multiple risk factors.
I would give them fish oil capsules such as 8 a day, unless I already knew they had been taking 4 a day for a long time.
I would also give them 10 or so mg boron a day. ../#08-boron
(At this point, your doctor is probably getting cranky because most
doctors do not know boron is an important nutrient for animals, that
the typical 1mg a day or so intake contributes in some or many people
to hyperinflammatory immune dysregulation, or that 20mg a day is the
level above which safety might be a concern. 114mg of laundry
borax, not substitute, provides 10mg of boron. The half-life in
circulation is 22 hours or so. My wife and I use 12mg boron a day, but
6 would probably be fine too.)
I would give them a gram or two of vitamin C a day, and some zinc (chelate, not oxide).
If they had a fever, I would not try to lower it because the pre-COVID-19 research I read ../fever/ indicated strongly that with a few exceptions, fever is a vital part of the early response to infection.
If, despite this, the person
developed breathing difficulties or any other signs of severe symptoms,
I would raise Hell to get a doctor or nurse to attend, or at least give
advice.
Doctors - especially in ICUs!
Please see the
../icu/ page and read up on the Marik Protocol AKA MATH+ Protocol.
Why not give every COVID-19 patient that arrives in hospital a gram of vitamin C and 2.5mg (100,000IU) at least, of vitamin D3?
Better still, can you give them oral (Rayaldee) or injected or IV 25OHD calcifideol?
Unless you know the patient has been supplementing with substantial D3
for weeks, then you can reasonably assume that their 25OHD levels are
low, and that you should move mountains to get it up to
40 to 60ng/ml
ASAP, ideally in an hour or so - with oral or parenteral 25OHD. Oral or IV D3 will
take days or a week or so to be converted in the liver (if the liver is
working) to the 25OHD your patient's immune cells desperately
need. By then it might be too late - hence the reason for large
D3 bolus doses including for instance half a dozen fish oil capsules.
Why not give them plenty of fish oil capsules?
Likewise zinc?
For you and your colleagues - all those who work in the hospital, or in
ambulances - why not raise their 25OHD levels as a matter of utmost
urgency, and get them all on vitamin C, omega 3s and zinc?
Vitamin D toxicity
Here are some links to research articles concerning vitamin D toxicity.
I want to do more work on this section, but it might be a while before I can do so.
It seems that many doctors, through an over-abundance of caution,
applied multiple times in series as warnings and maximum 25OHD levels
are passed from one doctor or committee to the next, in the chain which
links actual observations of hypercalcemia to the ordinary doctor's
understanding of those observations . . . that the notion of vitamin D
toxicity has been overdramatised to the point where some doctors,
especially in the UK, think that 10ng/ml is a healthy 25OHD level, and
that anything over 0.1mg (4000IU) a day for any adult carries an
unacceptable risk of vitamin D toxicity.
It seems that the best, up-to-date, academic journal article on vitamin D toxicity is:
Vitamin D Toxicity – A Clinical Perspective
Ewa
Marcinowska-Suchowierska, Małgorzata Kupisz-Urbańska, Jacek
Łukaszkiewicz, Paweł Płudowski and Glenville Jones. Front. Endocrinol.
2018-09-20
https://doi.org/10.3389/fendo.2018.00550
|
I think the previous widely cited reference work on this was:
An important commentary and related article:
Sarcoidosis is a condition in which
hypercalcemia can occur due to overproduction of 1,25OHD in some immune
system cells leaking into circulation and disturbing calcium
regulation. The most obvious response to this is to reduce both
calcium and vitamin D (25OHD) levels. However this is not
necessarily the correct response.
Sarcoidosis involves extreme immune system
dysregulation in which various types of immune cells attack each other,
mistaking each other for pathogens, and clump together all over the
body. Sounds like a vitamin D deficiency problem, doesn't
it? (Boron, omega 3 PUFAs, vitamin C too??) There may also
be bacteria multiplying inside lymphocytes.
The next article reports that vitamin D and calcium supplementation
for sarcoidosis patients is beneficial and does not result in
hypercalcemia:
To do: look at the articles which cite this one.
Taking supplemental D3 in various forms, with or without meals
I have only had a quick look at the
research on these questions. The findings seem to involve some
contradictions Google:
"fatty meal" "vitamin D" .
I understand that D3 already dissolved in water - such as in
fruit-juice supplemented with D3 - is quite well absorbed.
However, this is not relevant to the current discussion, since no-one
is going to drink so much fruit juice as would be required to total
0.15mg (5000IU) a day. I guess the same applies to vitamin D
gummies.
Not counting D3 in bottles of oil, there are three types of
supplemental D3: dry tablets, capsules with dry powder and oil-filled
capsules. Since D3 is fat soluble, I would expect the oil
filled capsules to be the most bio-available of these. However,
as far as I know, 1.25mg (50,000IU) capsules all contain dry powder.
Here is some research with mixed results, but overall support for taking oil capsules after a meal containing fat:
With these dry tablets, dry capsules or oil capsules I guess the worst
way of taking them would be without a meal, with lots of water.
This would wash them through the intestines relatively quickly, and the
intestines would not be geared up for absorbing fats.
I guess that the best approach would be to take D3 capsules towards the
end of or after a substantial meal containing at least some fat - as
most do - and then not drink too much for a while (which is good
general advice anyway). Then there is a chance for the D3 to
spend more time in the upper parts of the intestines, with them being
in a fat-absorbing mode of operation.
The same would be true of daily omega 3 capsules - though it is
possible that four of these might be detected by the body as a fatty
meal, and so be reasonably well absorbed.
My current preference is for taking D3 at the end of dinner, or with
omega 3 oil capsules after breakfast - since we don't want to take the
omega 3 capsules with or after dinner.
Some supplements, such as iron vs. calcium and/or magnesium, need to be
taken at separate times because each upsets the other's absorption
processes and the quantities involved, such as for calcium or magnesium
are quite large. D3 quantities are very small and I am not aware
of D3 disrupting any other nutrient's absorption, or of any other
nutrient disrupting D3's absorption.
The GrassrootsHealth researchers and MDs also recommend taking D3 with
a fatty meal. Their guide to vitamin D supplementation quantities:
cites this 2014 article
https://pubmed.ncbi.nlm.nih.gov/25441954/ which supports taking it with a fatty meal to maximise absorption.
../ to the main COVID-19
page of this site.
To the index page of this site: ../../
Contact details and copyright information: ../../contact/
©
2020 Robin Whittle - please link to this site rather than copy the
whole of its contents Daylesford, Victoria,
Australia