Vitamin D & other nutritional supplements to
protect against severe COVID-19 symptoms
This is the only way we can cope with COVID-19 without the twin
disasters of the suffering, harm and death caused by some people's
weakened and dysregulated immune response to SARS-CoV-2 infection
and the comparably deadly, disastrous, lockdowns which are currently
government's only way of protecting people from harm and death.
(The current vaccines - most of which are not true vaccines and are
highly experimental - are protective for a while and are . However, new viral variants
require repeated rounds of vaccination of most of the population - and
the variants arise faster than this can be done.)
Ivermectin is also useful for prevention and treatment of COVID-19.
For links to the most pertinent
research on why vitamin D (and Ivermectin) are effective at reducing
severity of COVID-19, as well as reducing transmission, please see this
page on my other site:
I am writing articles (three so far) at https://nutrtionmatters.substack.com - where comments an be made.
Robin Whittle rw@firstpr.com.au 2022-02-27
Recent updates:
Generally the material on this site dates from mid 2020. Please see the above two sites for more up-to-date information.
There are two items on this or a related page which do not directly
relate to COVID-19, but which are of general interest, and which I try
to update. These are not elegantly formatted or anything like the
complete information I would like to provide, but I don't have the time
to do a proper job on them in the foreseeable future:
Potassium supplementation to increase the potassium to sodium ratio and
so reduce the risks of stroke, high blood pressure etc. See:
https://aminotheory.com/cv19/kna/ .
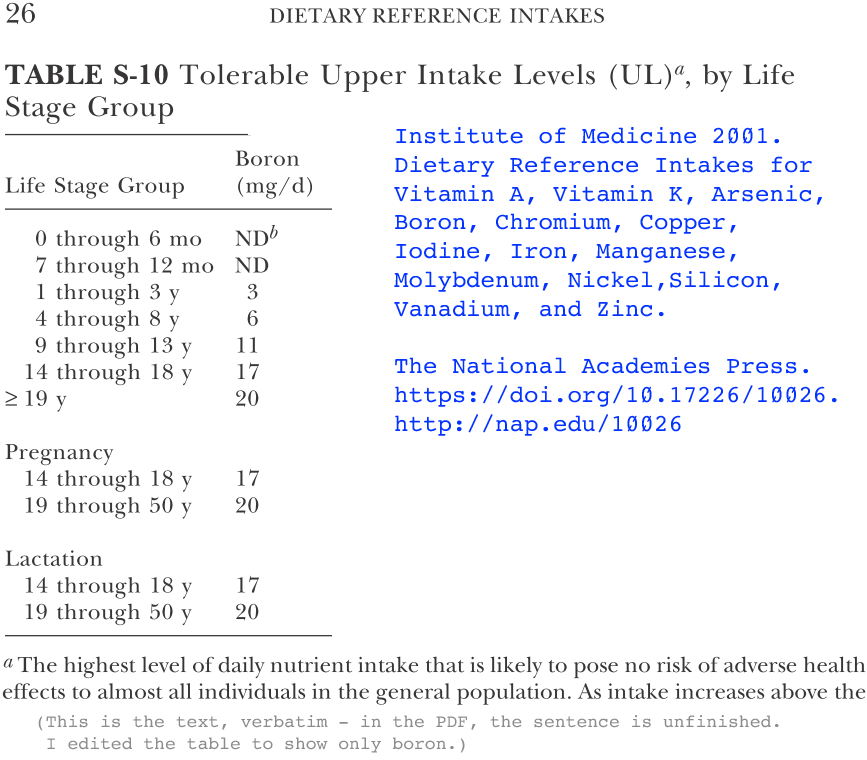
Boron supplementation for various reasons, including reducing
inflammatory autoimmune diseases and the risk of kidney stones, as well
as to enable existing kidney stones to disintegrate without the need
for surgery or ultrasound treatments:
This is a sub-section of the same page you are reading now, which I admit has grown to be unreasonably long:
https://aminotheory.com/cv19/#08-boron
. This concerns the fascinating field of boron nutrition. I
added a new section on 2022-02-27 concerning boron supplementation to
prevent the formation of kidney stones, and to disintegrate existing
kidney stones - including those identified by ultrasound which would
otherwise need surgical or ultrasound interventions:
https://aminotheory.com/cv19/#boron-kidney-stones .
Be sure to read the
Disclaimer below:
#disclaimer
which is followed by contact and copying details. I am not a
doctor. Even if I was, I have not examined you.
Be sure to see the list of recent research articles #lr !
Please see
Over 200 Scientists, Doctors, & Leading Authorities Call For Increased Vitamin D Use To Combat COVID-19:
https://vitamindforall.org/letter.html
If you are really interested in nutrition and the immune system,
please also consider joining the Nutrition for Immune System Health
(NISH) email discussion list, which I run:
https://NISH.groups.io .
I have a second website, and some infographics there and below:
Some of these infographics were in tweets: https://twitter.com/RobinWhittle3/
#vc
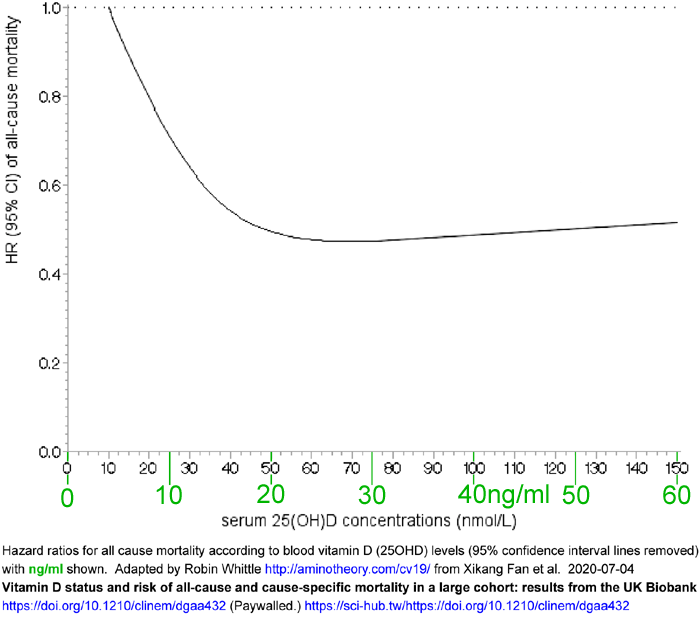
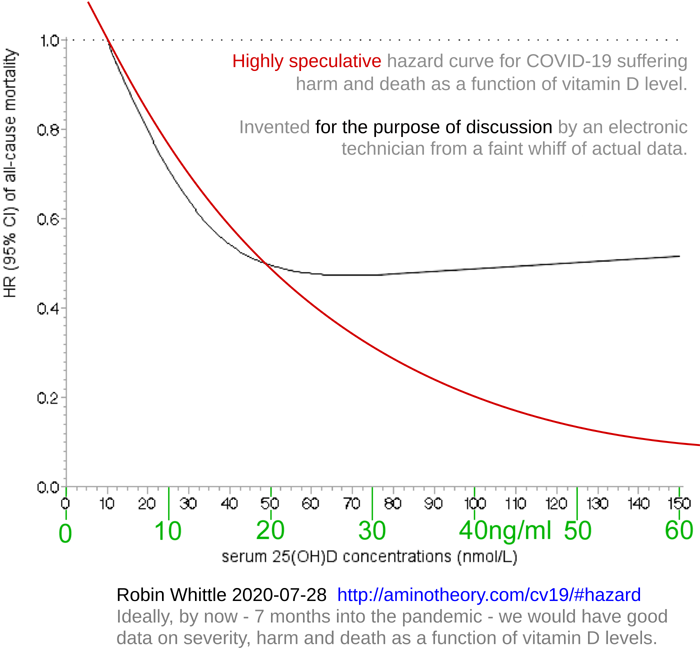
Biobank:
#2020-UK-vit-D-BAME
.
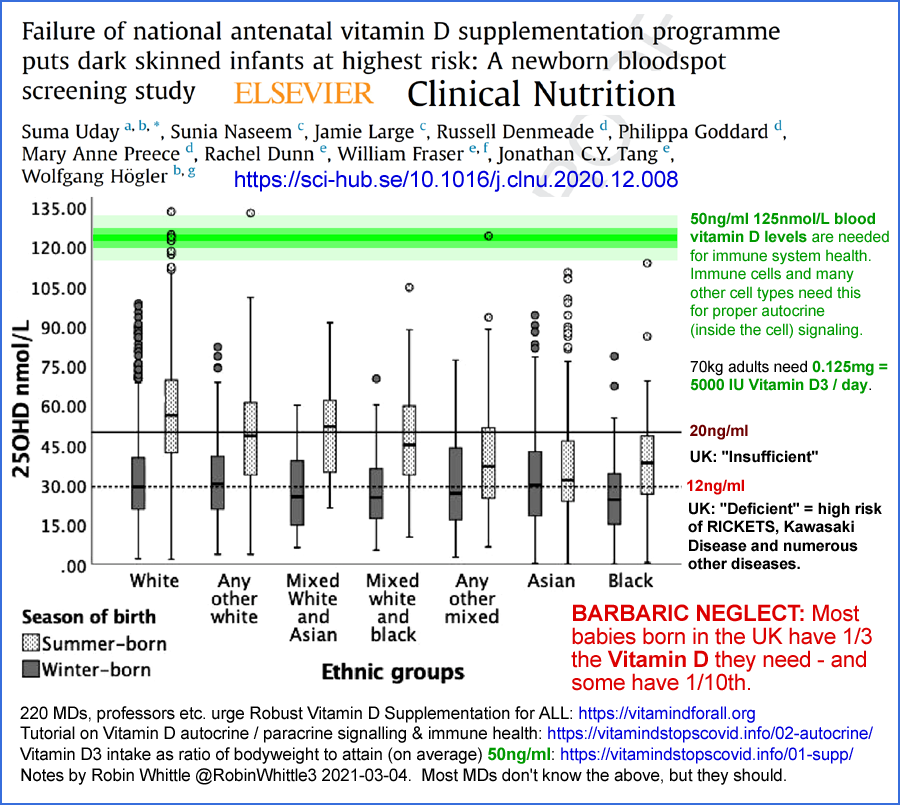
Vitamin D status of children with Paediatric
Inflammatory Multisystem Syndrome Temporally associated with Severe
acute respiratory syndrome coronavirus 2 (PIMS-TS)
Angeline Darren, Suma Uday, Deepthi
Jyothish and 9 others
British Journal of Nutrition, 2021-05-12
https://doi.org/10.1017/S0007114521001562
The association between vitamin D levels
and the clinical severity and inflammation markers in
pediatric COVID-19 patients: single-center experience from a
pandemic hospital
Elvan Bayramoglu, Gülsen Akkoç, Ayse Agbas, Özlem Akgün,
Kamer Yurdakul, Hatice Nilgün Selçuk Duru & Murat Elevli
European Journal of Pediatrics 2021-03-31
https://link.springer.com/article/10.1007/s00431-021-04030-1
For the Stagi et al. 2015 article on Kawasaki disease and vitamin D: #2015-Stagi.
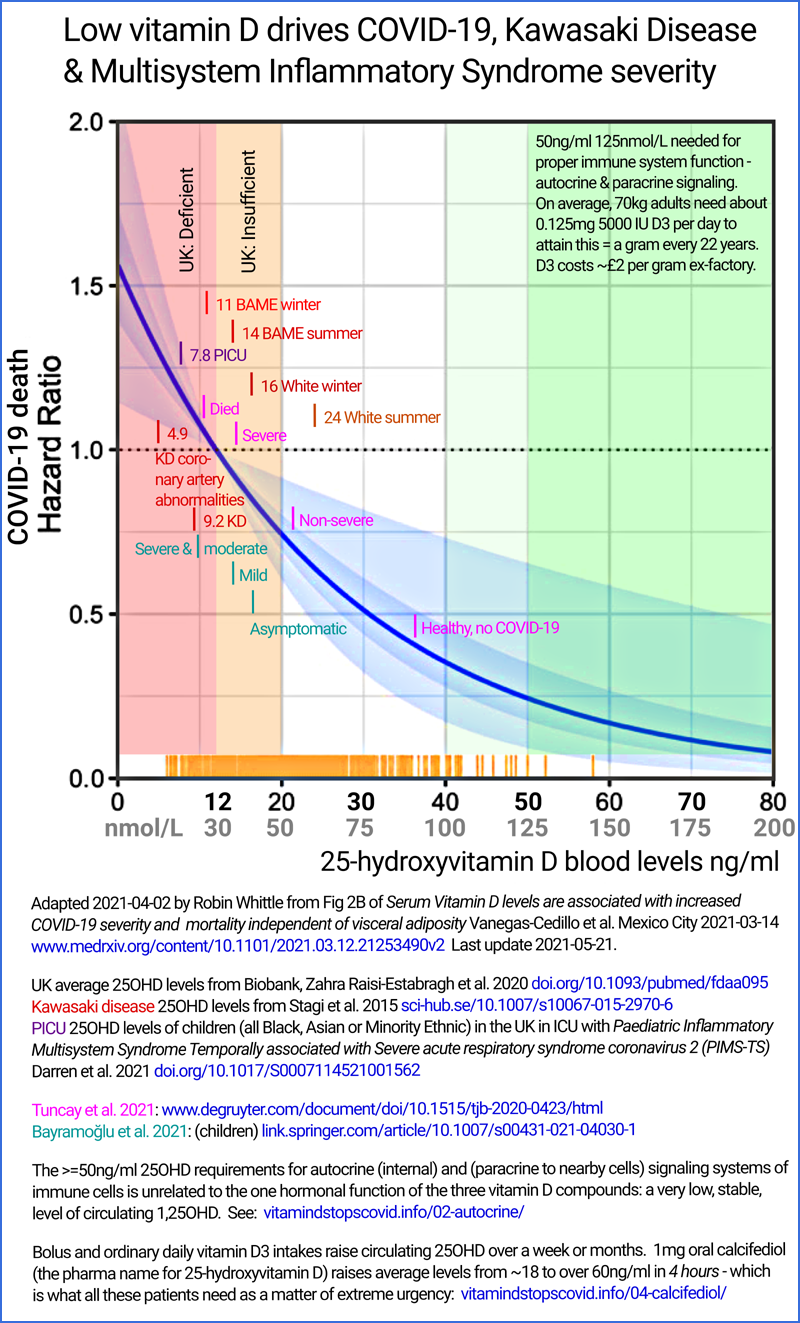
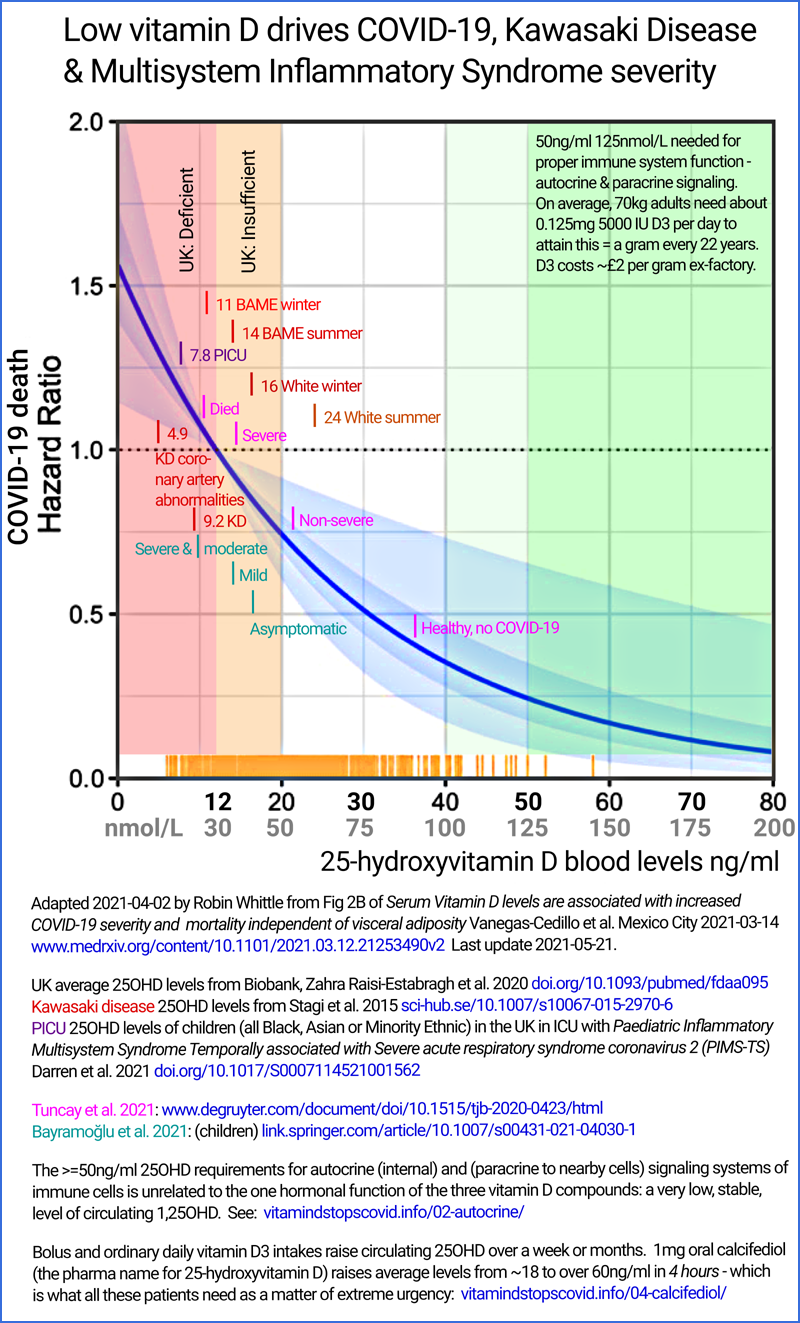
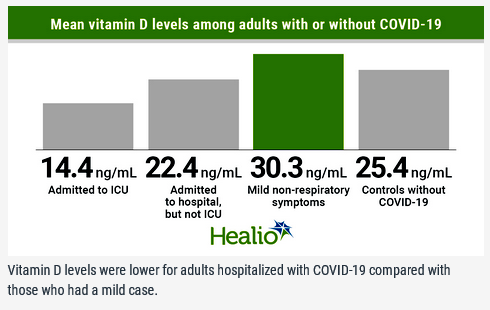
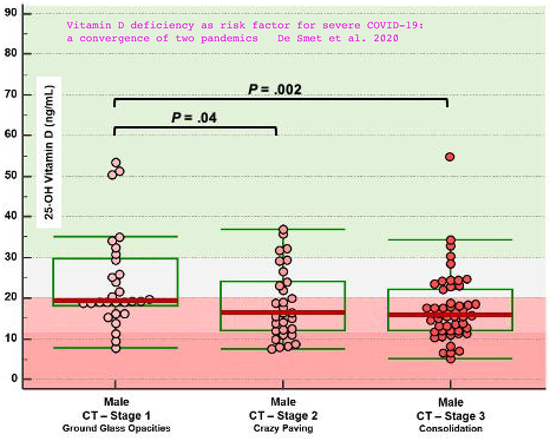
Different observations show the same relationship between low
vitamin D and severe COVID-19, although here the vitamin D blood
level is on the vertical axis:
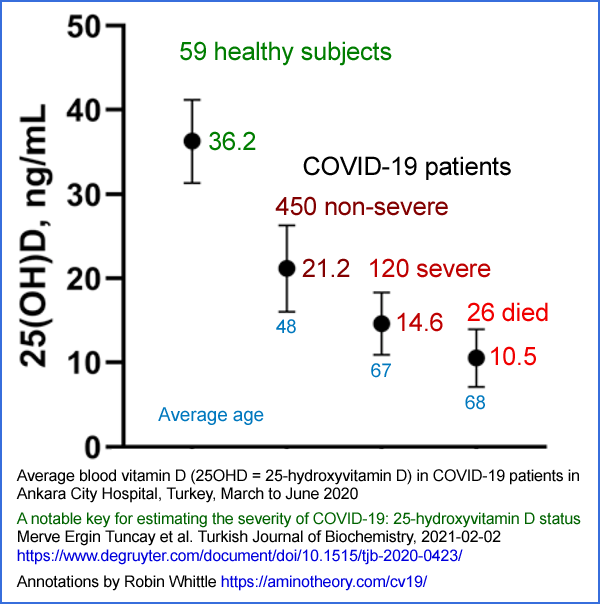
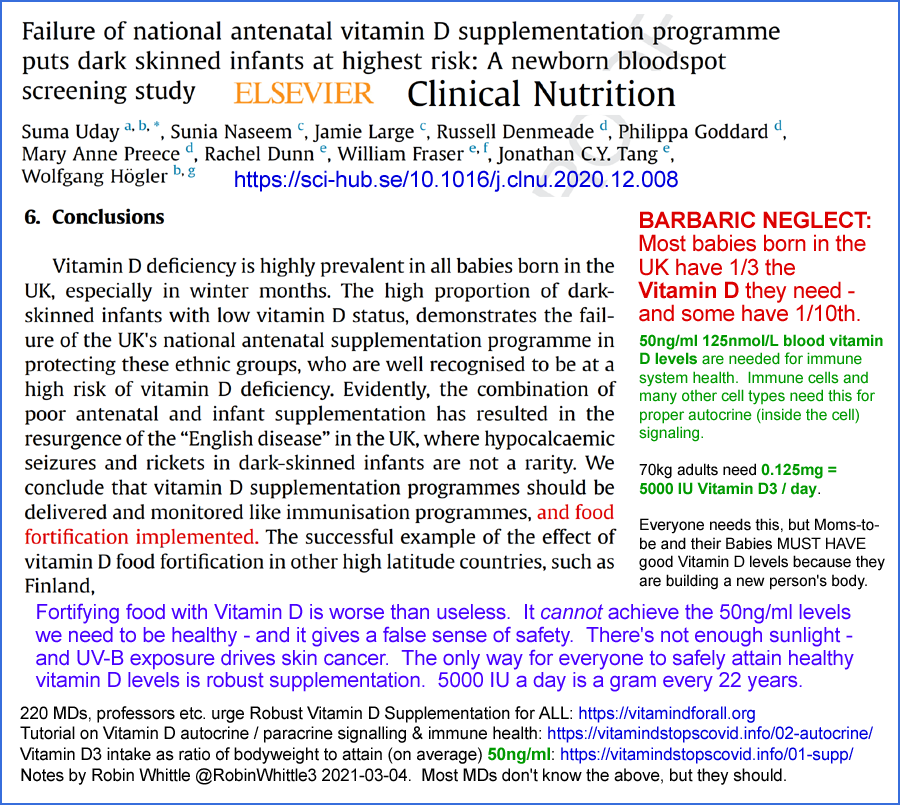
#uknewborns
Two infographics concerning the very low vitamin D levels of
newborn
babies in the UK. Their mother's vitamin D levels are on average
about 40% above their baby's levels - and these are still low for most
mothers.
Babies are trying to build their bodies. It is
Adults' responsibility to ensure Babies and their Moms are well
nourished. With all our knowledge and resources, we should do
better in this, the most basic and important of our
responsibilities. The failure to do so for so many Moms and their
Babies seems to me like BARBARIC NEGLECT. (I know it is mum in England, where I was born, but I like the American mom which is good in both private and public contexts.)
While I share the authors' serious concern about these low levels, I
am opposed to fortifying food with vitamin D because it cannot achieve
the ~50ng/ml 125nmol/L 25OHD levels we need, because it may give a
false sense of security and because all government efforts which might
to into food fortification would be better directed at encouraging and
supporting everyone to robustly supplement with vitamin D3, all year
round, with perhaps less in summer - while avoiding excessive (sunburn
creating) UV-B exposure: https://vitamindstopscovid.info/01-supp/
and:
#ukseas
Quick intro
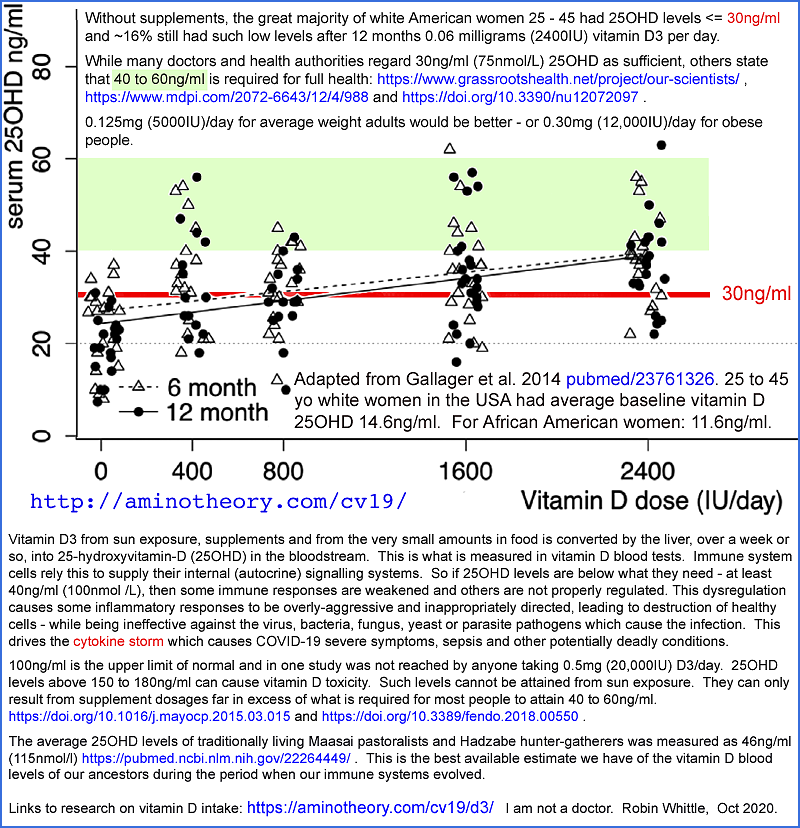
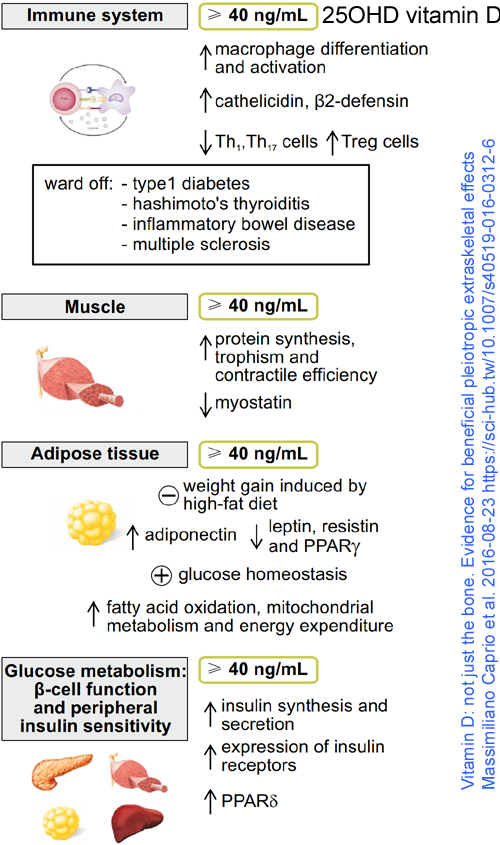
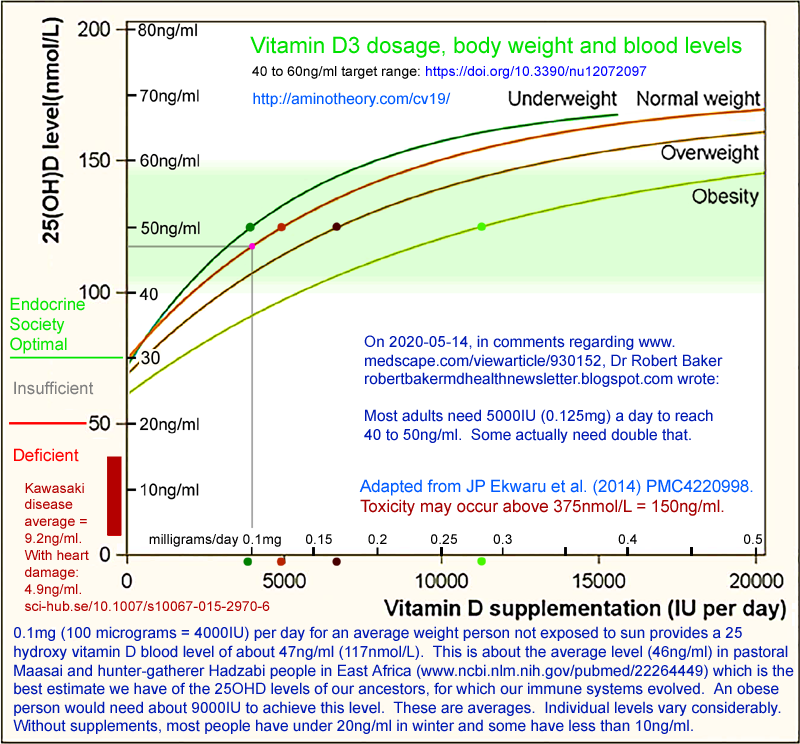
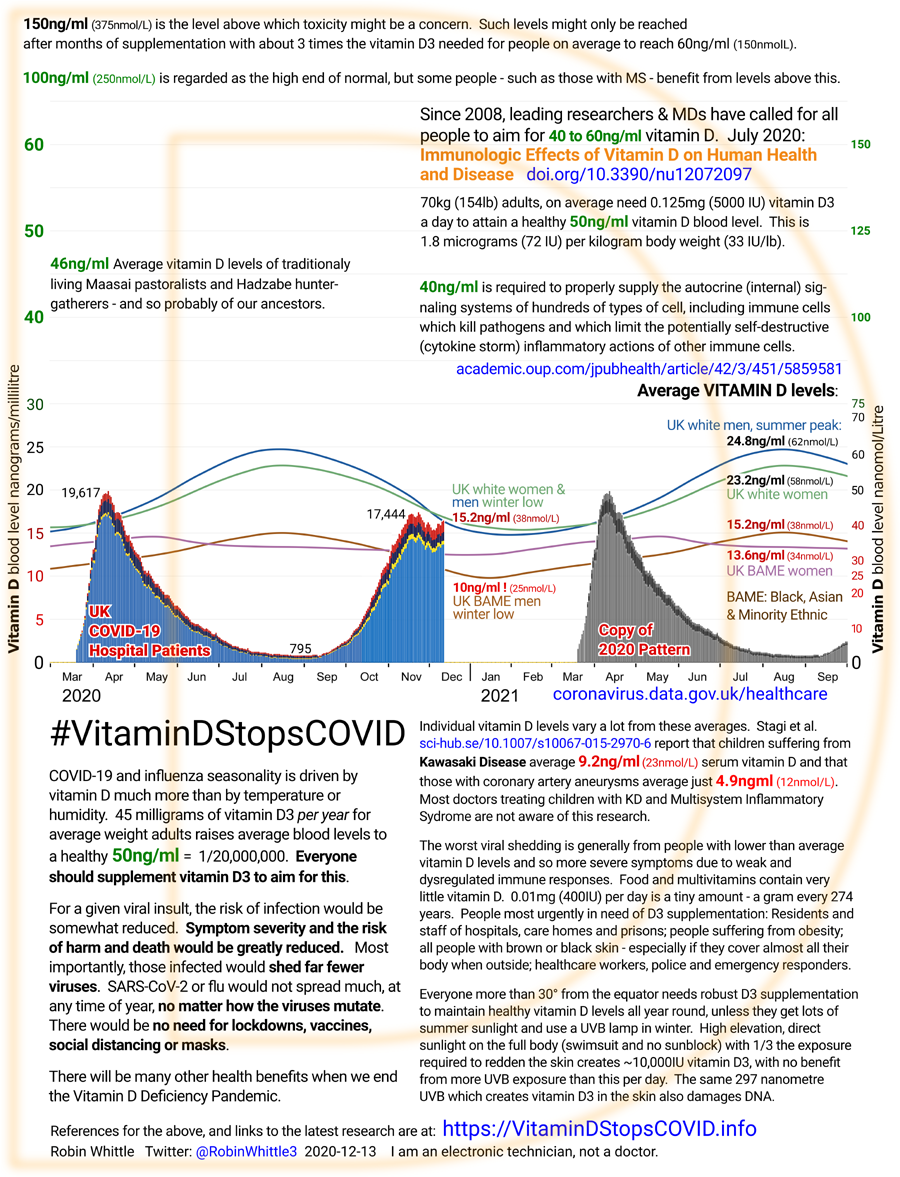
If everyone supplemented with
sufficient vitamin D3 to achieve ancestral blood levels (25OHD, the
form needed by immune cells and created from D3 in the liver) of
40 to 60ng/ml (100 to 150nmol/L = one part in 25 million to 16.7 million) then the autocrine signaling processes (explained
below) inside many types of cell, especially immune cells, would function properly.
With lower levels (such as
8 to
28ng/ml
- which is typical for people who do not supplement and who do not
receive much high elevation sunlight on their skin - the autocrine
signaling cannot work properly, so immune responses are both
weak and
dysregulated.
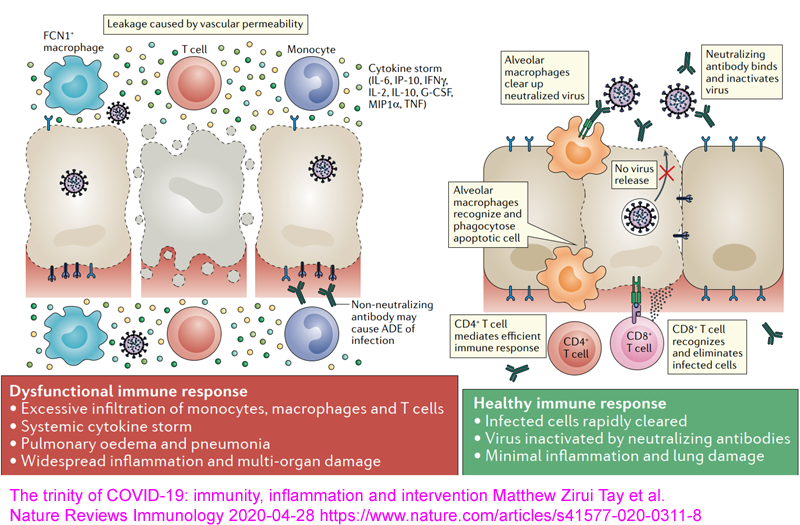
"Dysregulation" means overly-aggressive, pro-inflammatory and
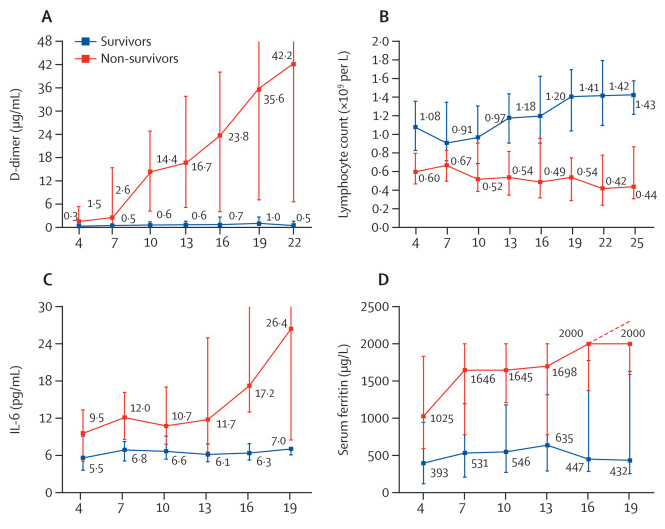
destructive - responses which drive the cytokine storm which is the
fundamental mechanism of COVID-19 severe symptoms and sepsis.
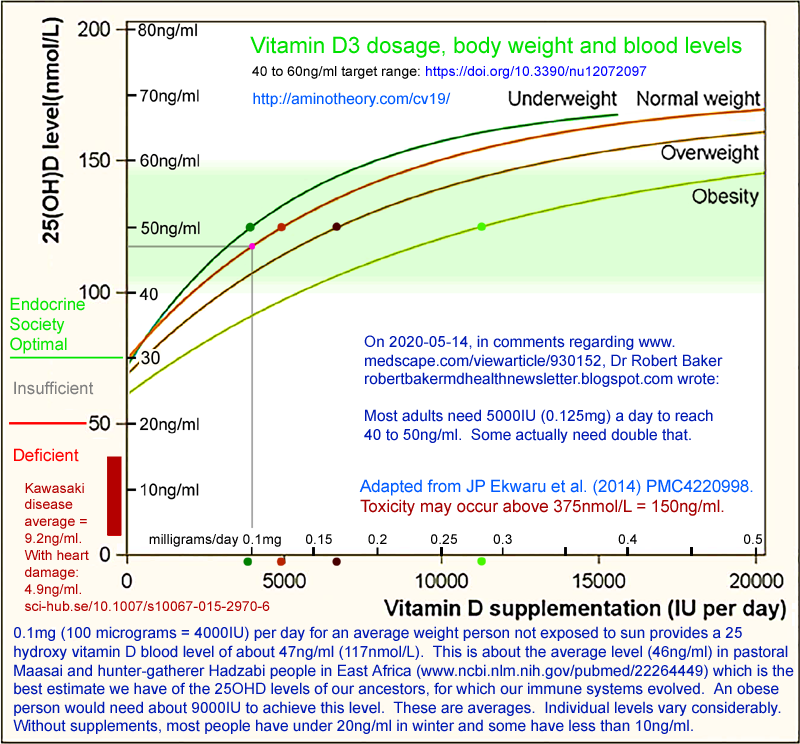
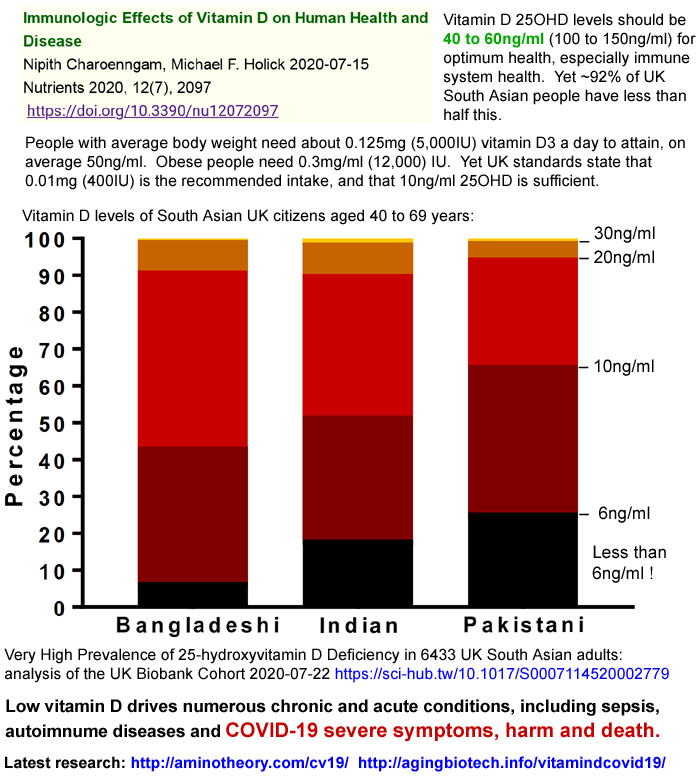
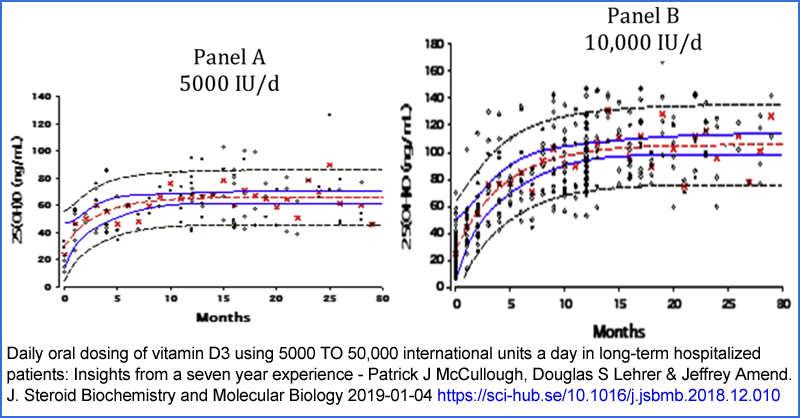
To achieve these target levels of
40 to 60ng/ml,
average weight adults need 0.125mg (5000IU = 1/8000 gram) of D3 a day -
and it is fine to take this average amount once every week or
two.
This is about ten times the intake many governments recommend. For instance the UK government recommends 0.01mg (400IU) D3 a day with vitamin D deficiency being defined as below
10ng/ml
(25nmol/L) - less than a quarter of what we need.
0.125mg is a gram every 22 years, and the ex-factory price of
pharmaceutical D3 is USD$2.50 a gram. So the cost of this
45 milligrams of D3 a year is about
US 13 cents a year.
(It just needs to be made into 52 weekly capsules of 0.875mg D3.)
Overweight people need more than this and obese people should take at
least twice as much. (See the
d3/ page for
details.) Toxicity is possible at levels above 150ng/ml,
but this can only be attained by weeks or months of ingesting ten or
more times this.
If everyone aimed for these this
40 to 60ng/ml
definition of vitamin D repletion, and most people achieved this
(there's not enough doctors or labs to be continually testing the
world's population for their 25OHD blood vitamin D levels), some would
have less than this and quite a few would have more, which is
fine. It would double or triple most people's current
levels. Assuming this was achieved, then,
all year round,
no matter how dark a person's skin, and
no matter how little their skin is exposed to high elevation sunlight:
- Everyone would be somewhat less likely to be infected by the SARS-CoV-2 virus (which causes COVID-19) for any given viral insult.
- If they were infected, their symptoms would be much milder than if they were infected with their current deficient levels. In most cases there would be few, if any, symptoms. Severe symptoms would be very rare and likewise the risk of death would be very much diminished.
- If they were infected, they would shed viruses at a lower rate then they would with their former, deficient, vitamin D levels. They would also shed viruses for fewer days.
- So the spread of COVID-19 would be greatly reduced, and for most people there would be no problems if they were infected. (This would provide some immunity, for months or perhaps years.)
Consequently:
There would be no need for lockdowns, social distancing, masks or vaccines. COVID-19
would probably spread slowly to the majority of the population, and a
much smaller number of people - those people with other serious
health concerns, including obesity and old age - would need medical
care if they were infected.
It would not matter how the SARS-CoV-19 virus mutated.
The virus can mutate to a different form which is not affected by
immunity gained from prior current strain infection, or from vaccines
targeting current stains. Such mutations wouldn't alter the
protection from severe symptoms given by adequate vitamin D levels.
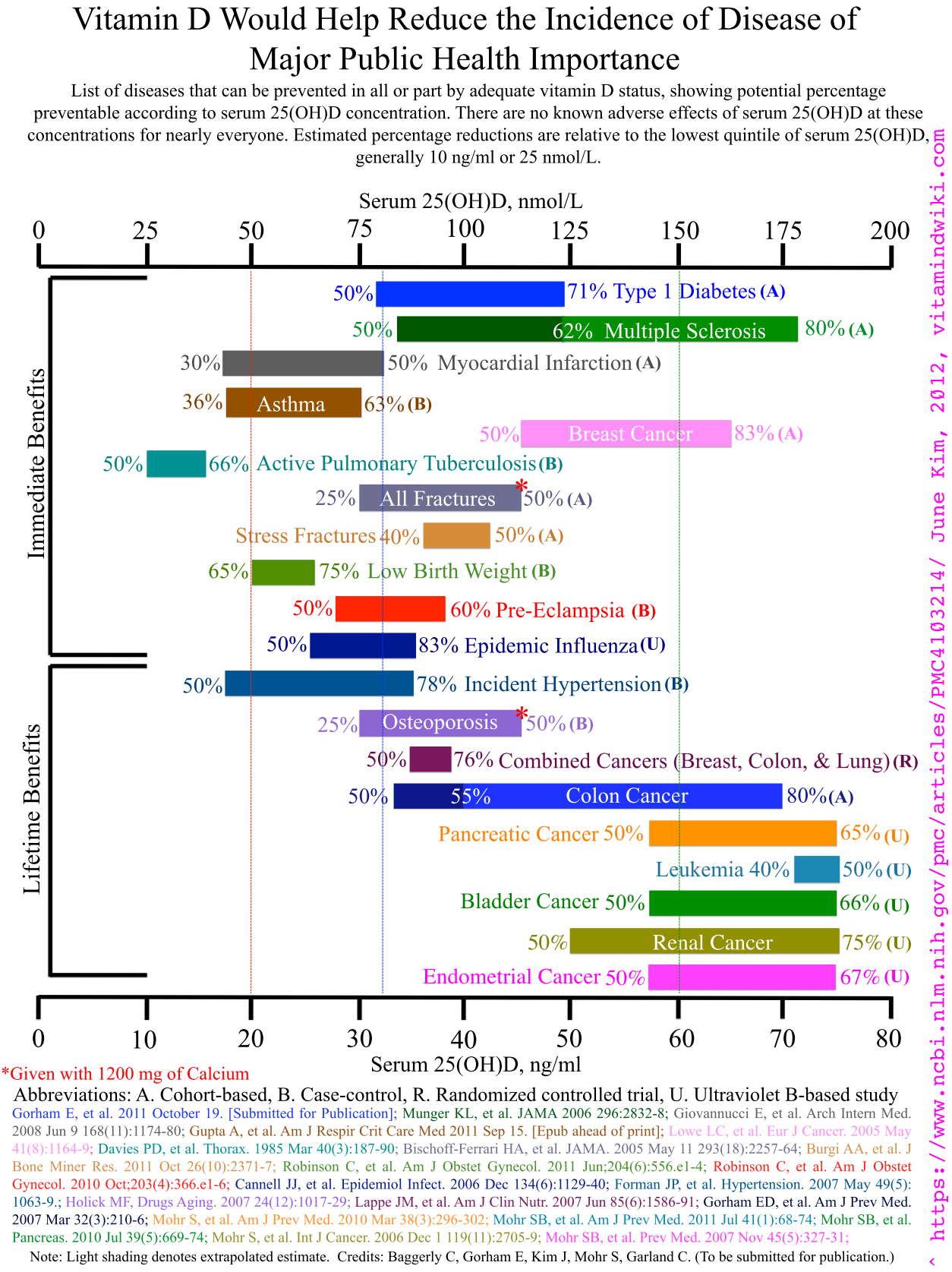
There are many chronic and acute diseases which are in small or large
part caused by vitamin D deficiency. These would become less
prevalent. See
#kp below for some of these listed.
Other major benefits of ending the global vitamin D deficiency pandemic include:
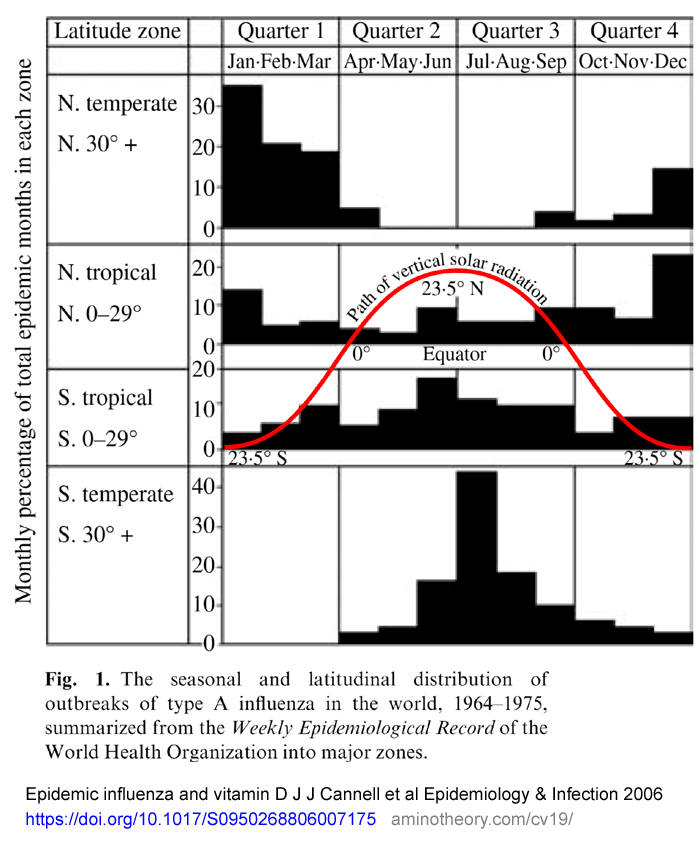
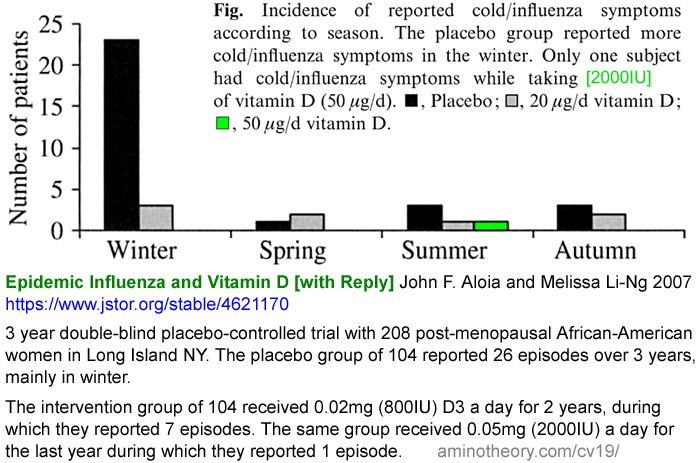
There would be no need for influenza vaccines. As with COVID-19, transmission and severity would both be greatly reduced, all year round.
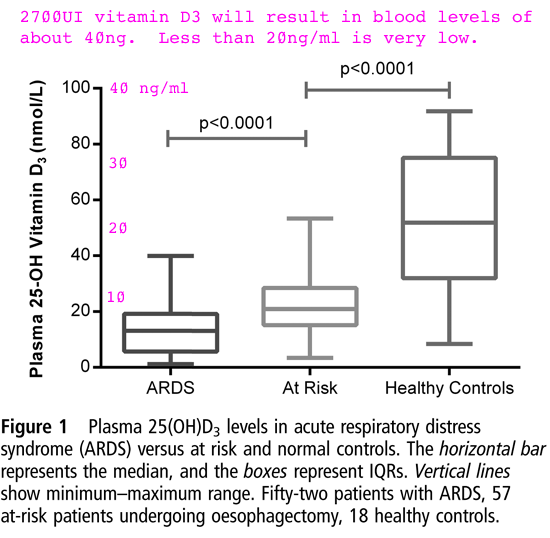
There would be a great reduction in incidence of sepsis - a suddenly occurring, difficult to diagnose quickly, immune dysregulation disorder which harms and kills within hours.
Likewise ARDS (Acute Respiratory Distress Syndrome) and, in children and adolescents, and Kawasaki disease and Multisystem Inflammatory Syndrome, both of which are triggered by COVID-19, but only in children and adolescents with very low vitamin D levels.
Most doctors are unaware of the importance of vitamin D to
immunity. For instance, despite excellent Italian research in
2015
#2015-Stagi showing that Kawasaki
disease children have very low levels of vitamin D, and those with the
lowest levels have the most severe symptoms (coronary artery
aneurysms), most doctors have no idea that low vitamin D levels are a
precondition for KD. So they don't supplement KD children with
D3, beyond whatever low level is in hospital food. The children
generally recover - perhaps in part due to gaining D3 from the plasma
transfusions they are typically given.
Most people assume that most doctors
are up-to-speed with all the pertinent research for whatever condition
they are being treated for. In the case of many diseases caused
by inadequate vitamin D, this is tragically not the case.
A handful of doctors and researchers have been trying to educate the
majority of doctors about vitamin D for decades, with limited
success. The need for this has long been critical, since millions
of people die from sepsis, influenza, ARDS and other conditions which
result in large part from inadequate vitamin D. The COVID-19
crisis makes this education campaign far more urgent.
Doctors and nurses have a very difficult job. They acquire
knowledge and experience of thousands of biological processes and human
diseases. They know all sorts of things, from
resuscitation, minor surgery, and ear cleaning to very complex
diagnostic criteria and drug interactions
They are generally not very well trained in nutrition and they are
constantly schmoozed by pharmaceutical companies. So they are
generally overly enamoured of drugs and acute interventions, and do not
know enough about nutrition, the immune system and prevention of
disease. There is a vast and at times bewildering array of
research and doctors absolutely cannot keep up with this. They
rely on guidelines developed by committees - and these are often out of
date and influenced by pharmaceutical companies.
Furthermore, many patients - unwisely - expect their doctors to give
them a pill or a vaccine or whatever to specifically fix their current
ailment.
Instead, doctors and patients should pay a lot more attention to nutrition and prevention.
Please ask your doctor to read this site, especially the sections on autocrine signaling in immune cells
#vitd-autocrine and the latest research on vitamin D and other nutrients regarding COVID-19
#lr .
2020-09-29 update: Please see this excellent video presentation at VitaminDUK.com :
1 BIG numbers – Analysis of 190,000 tests
Professor Michael Holick MD, Boston University - the world's foremost vitamin D researcher.
2 BIG view – Overview of 15+ trials
William Grant PhD, San Francisco - another long time vitamin D researcher.
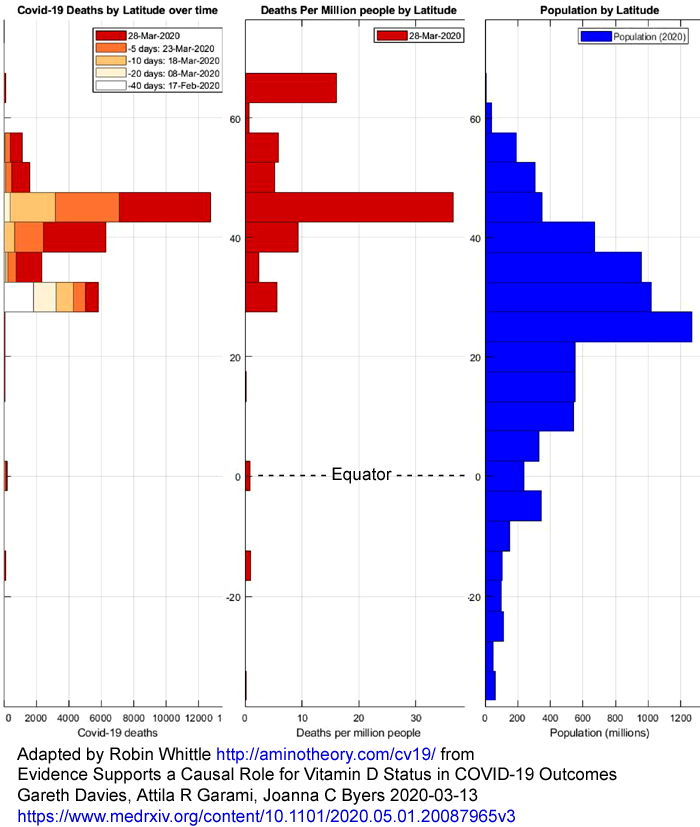
3 BIG data – Causal Inference from 240 locations
Gareth Davies PhD, physicist, UK.
4 BIG questions – Bradford Hill’s Criteria
David Grimes MD, gastroenterologist, UK. This is a great
presentation on all the criteria required to "prove" (in science,
establish the veracity of, beyond reasonable doubt) a medical
hypothesis - in this case that good vitamin D levels are essential for
good general health and for protecting against severe COVID-19 symptoms.
5 BIG answers – Next steps?
Rufus Greenbaum, citizen scientist, UK.
Vitamin D supplementation guide - especially concerning COVID-19
The
d3/ page links to the best research articles on desired vitamin D blood levels -
40 to 60ng/ml, and reproduces a diagram which shows the amounts of supplemental vitamin D3 which are needed to achieve
this, on average, for people with underweight, normal, overweight and obese body
types.
See also
https://VitaminDStopsCOVID.info/01-supp/
with vitamin D supplemental quantities as base and upper ratios of
bodyweight, for non-obese people and with a second pair of base and
upper ratios for those suffering from obesity. I derived these
from Ekwaru at al. 2014.
See also
3-reasons/ why
I want everyone in the world to have good nutrition for immune system
health. The first is general and simple. The second and
third are unique to the COVID-19 crisis.
#mn-xover
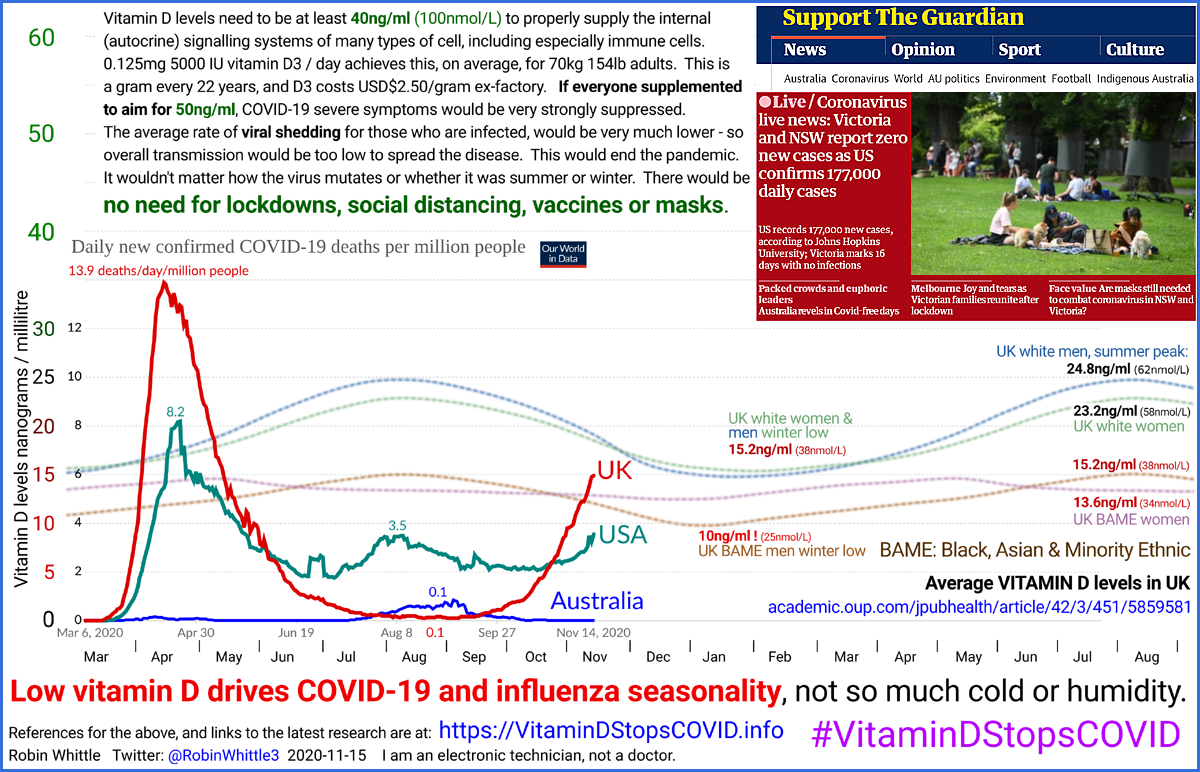
Mother Nature's crossover trial of summer and winter vitamin D levels
The infographics at the start of this page and at
https://VitaminDStopsCOVID.info
2020-08-28: Please see the 5th comment at:
which is
a good introduction to the material on this and other pages here.
2020-08-28, updated 2020-09-10:
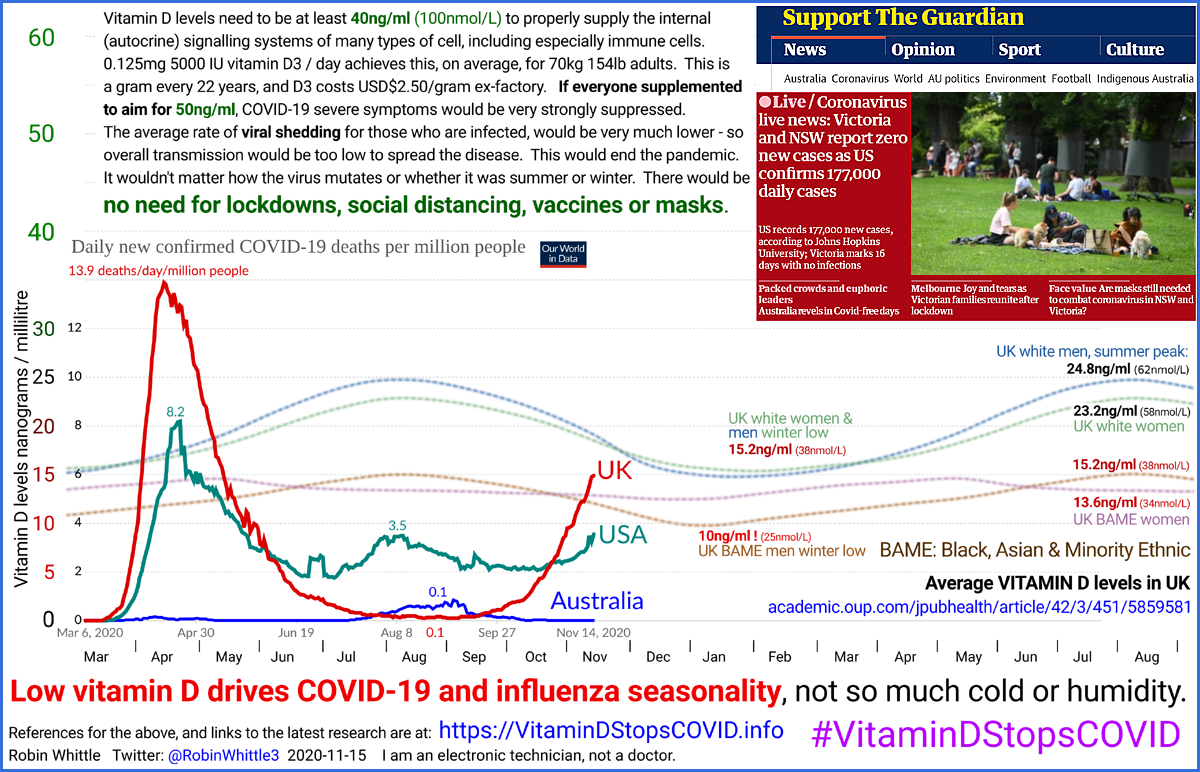
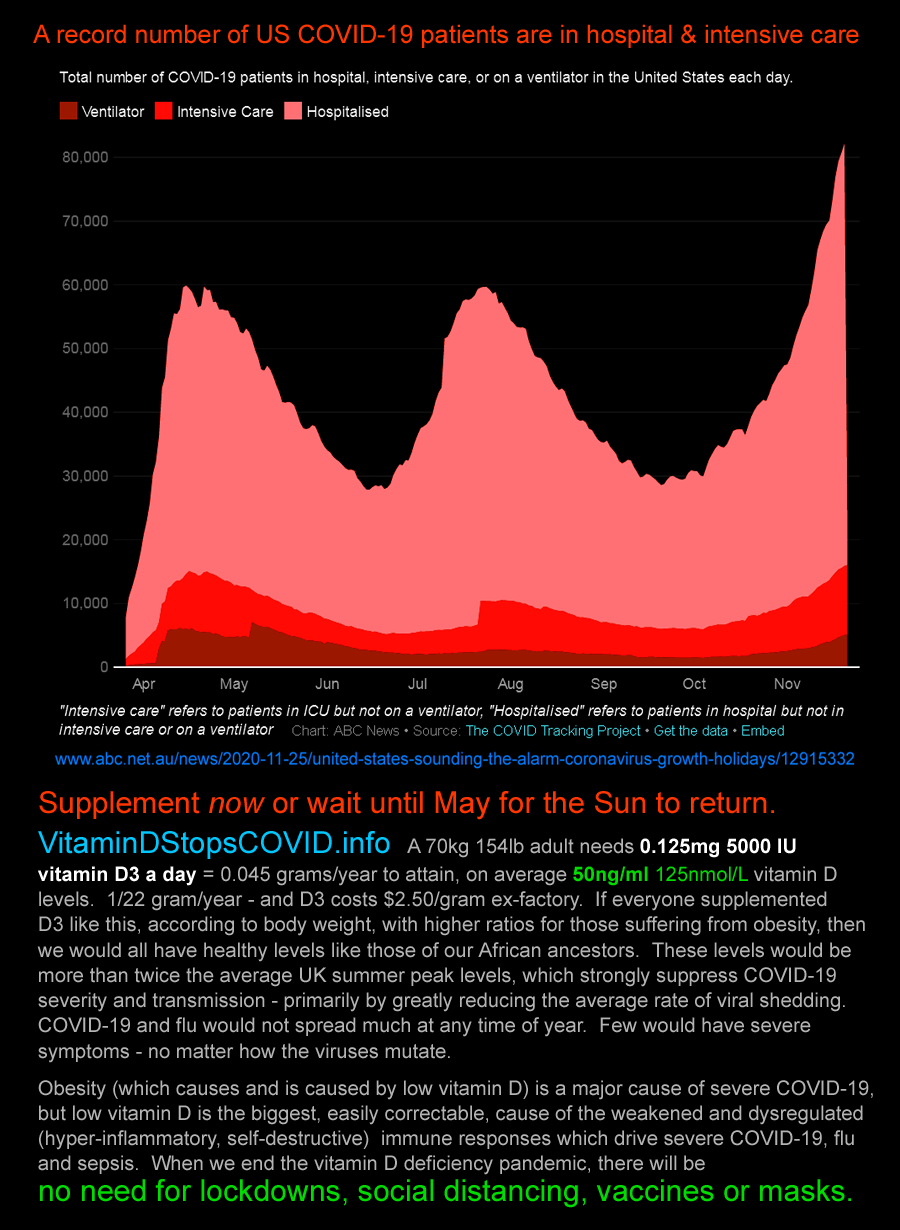
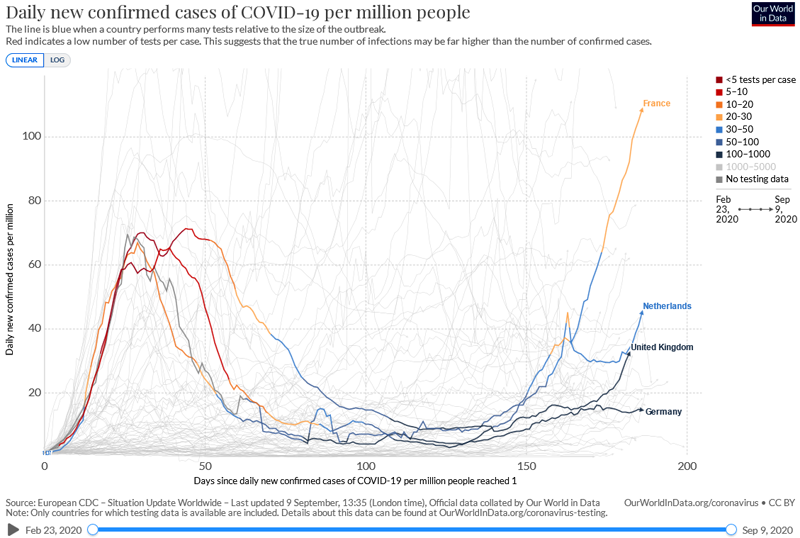
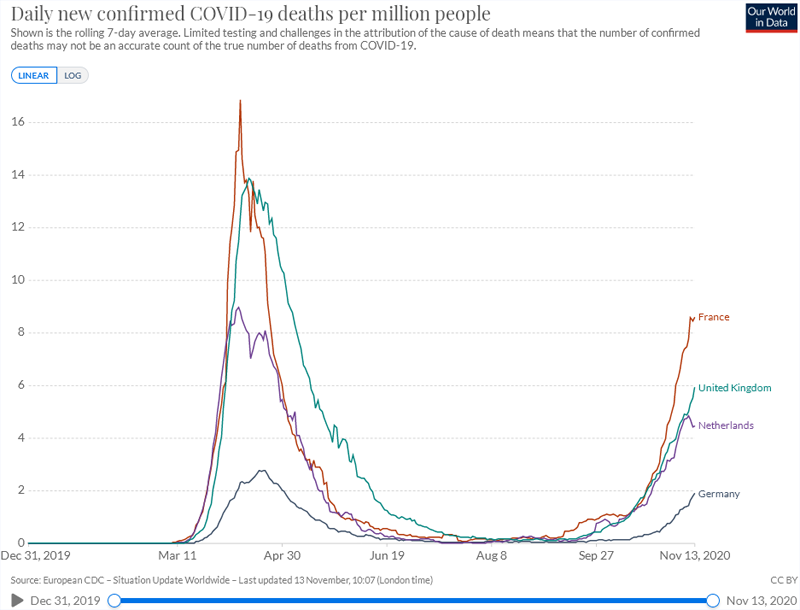
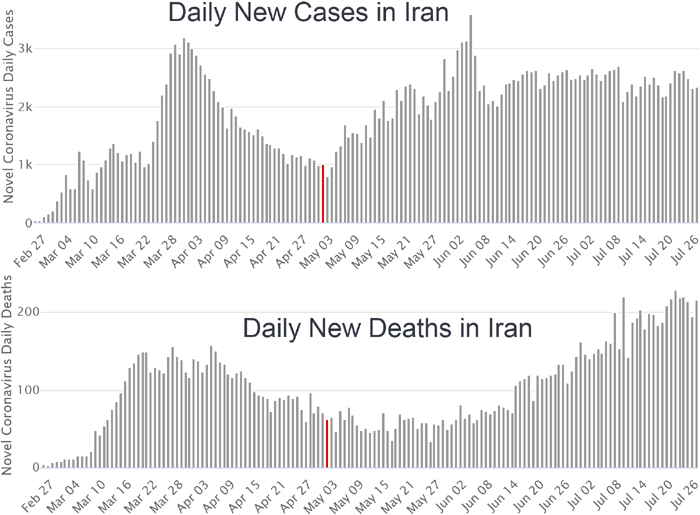
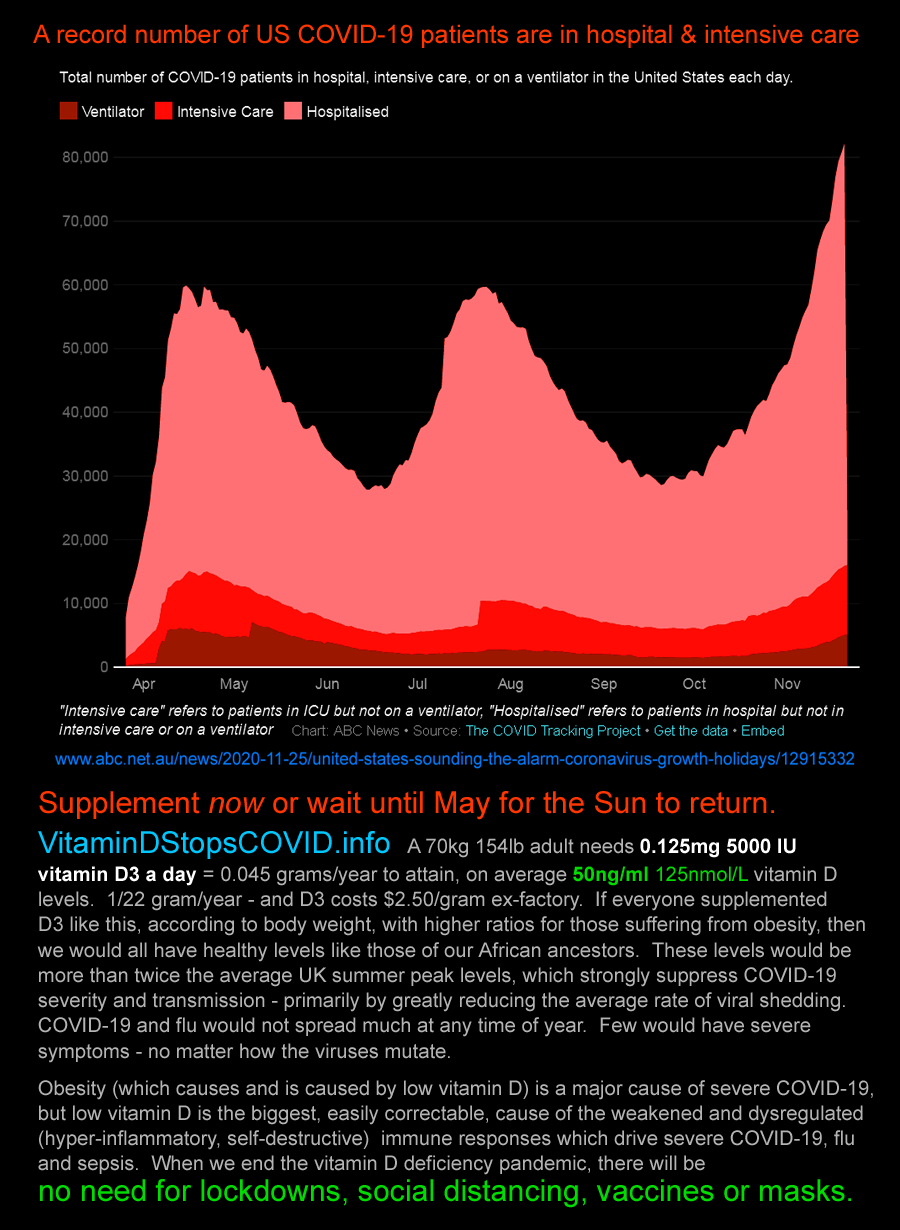
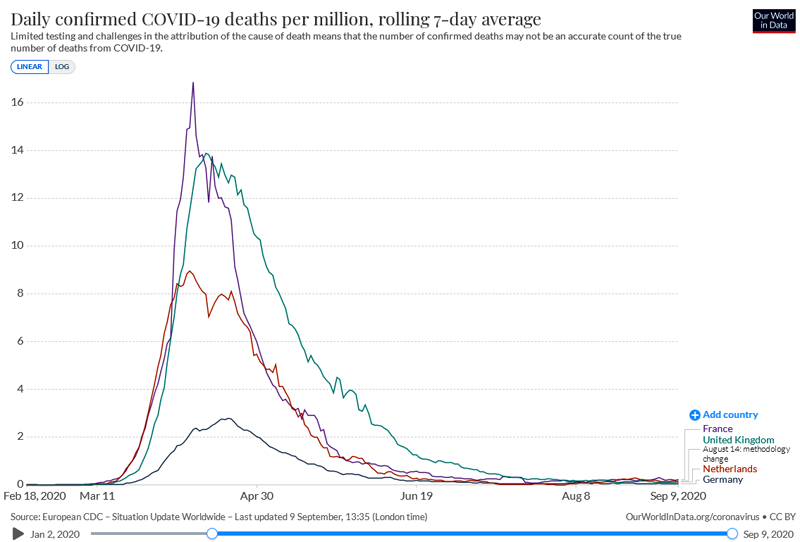
I argue against the common idea that the drop in new cases per day in
the UK and some other northern hemisphere countries, from about
April-May, is due to herd immunity. I argue that it is partly due
to lockdown, which is continuing, and mainly due to the summer peak of
vitamin D levels which somewhat reduces the chance of contracting the
disease for any given viral insult, but most importantly reduces the
severity of the disease AND reduces the amount of viral shedding, on
average. I propose that this lower level of shedding (which as far as I known has never been measured) greatly reduces
transmission and caused the drop in new cases per day per million
people, graphed below.
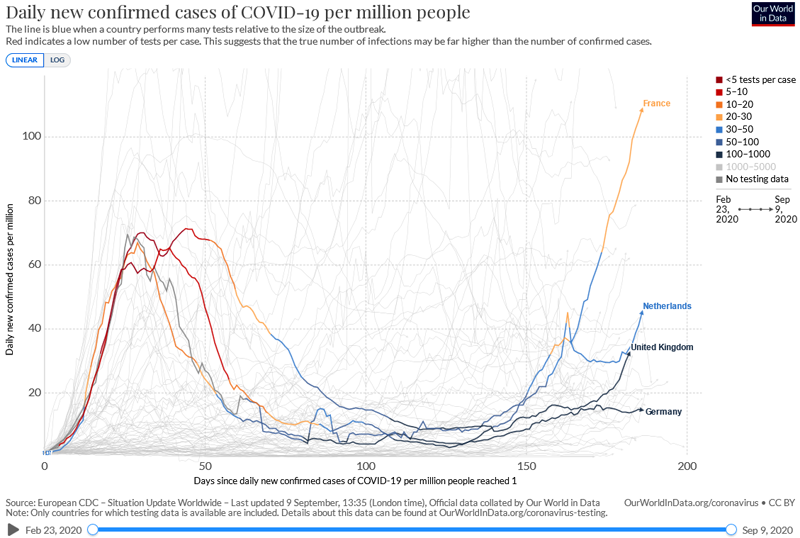 Link
Link
to the latest version of the above graph from Our World in Data - be
sure to move the right slider all the way to the right to the current
date.
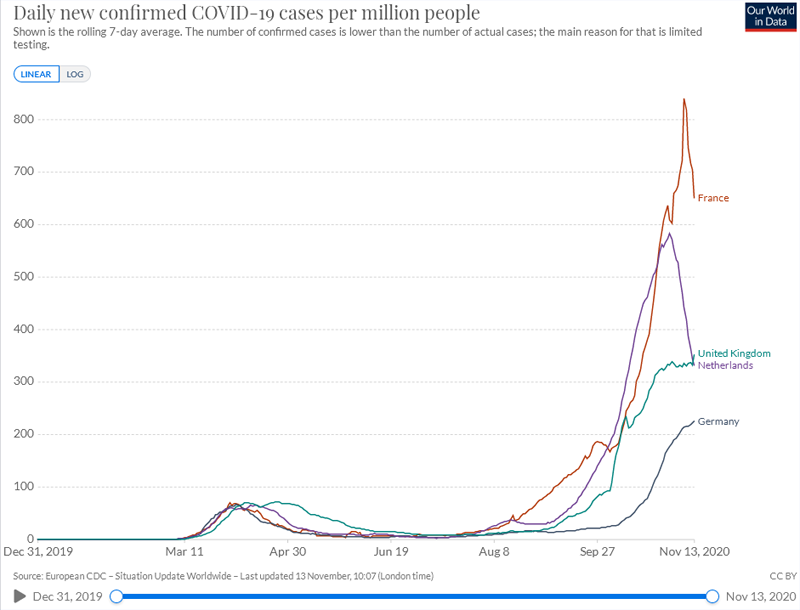
Here is what it looked like on 2020-11-13, this time all aligned by
date, rather than from the start of significant levels. The new
cases numbers are obviously higher than before, however there is more
widespread testing and the tests are not necessarily the same as those
in the past - they may be more sensitive.
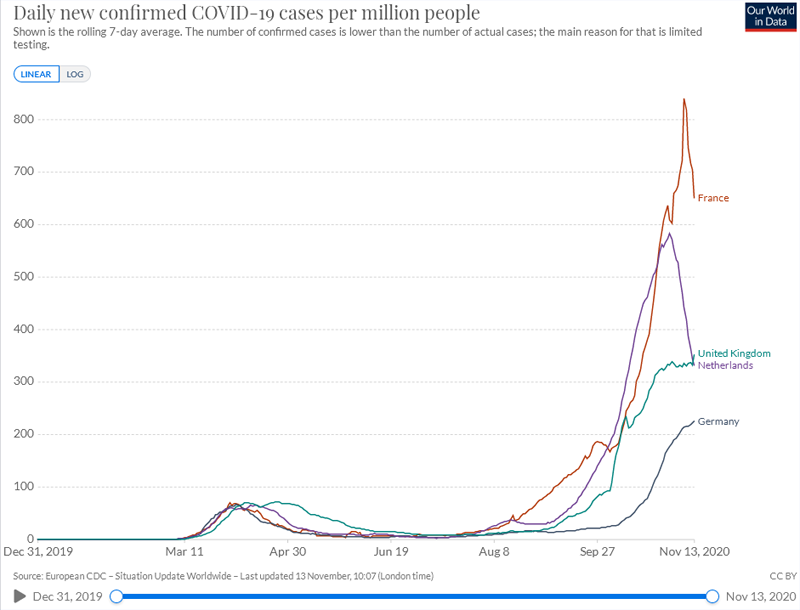 Link
Link
to the latest version. We see that "new cases" are rising again
in several these and some
other countries further north than about 35°. See the
infographic at the top of this page for UK hospitalisations, from the
government site:
https://coronavirus.data.gov.uk/details/healthcare .
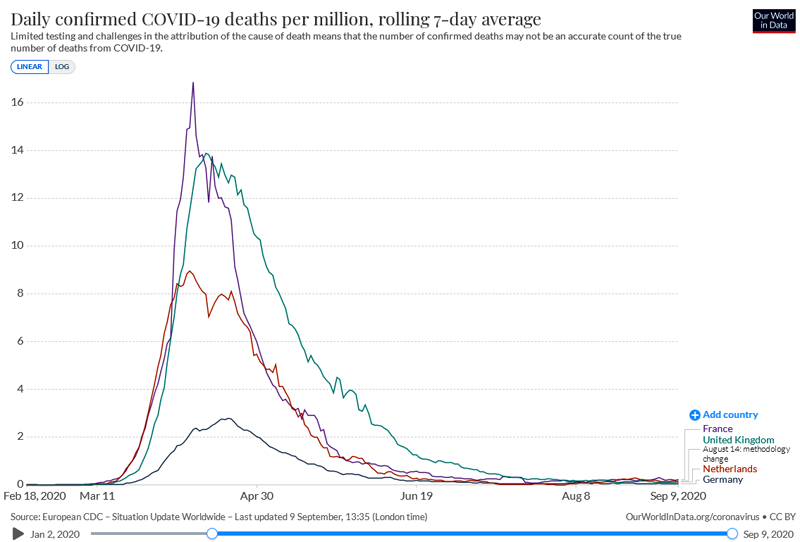
 Link
Link to the latest version of the above graph from Our World in Data.
Here are the deaths per million people on 2020-11-14, which are rising
alarmingly considering that relief from higher vitamin D levels from
sunshine won't come until about April. The number of real
cases in March to May was surely higher than shown in the two previous
graphs, as testing was less available and perhaps less sensitive than
it is now. Also, people are probably better cared for now than
then.
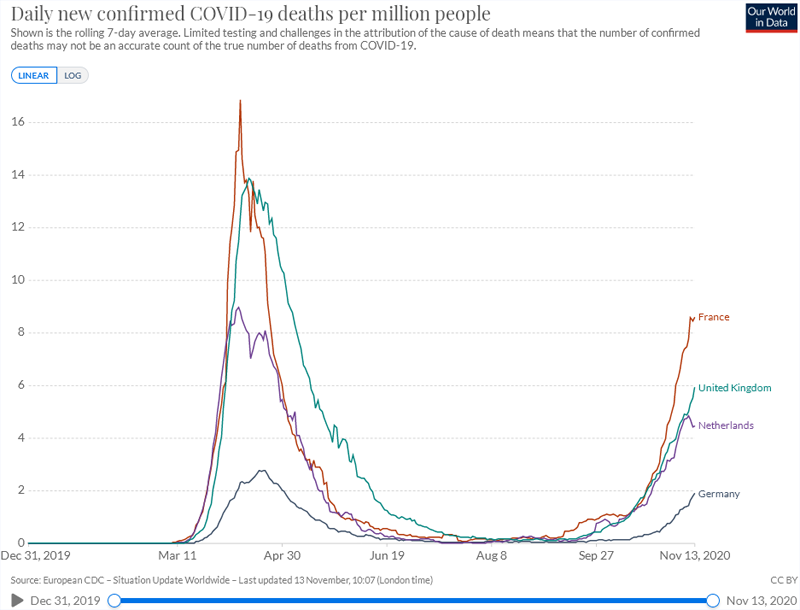
Link
to the latest version - be sure to move the right slider all the way to the right.
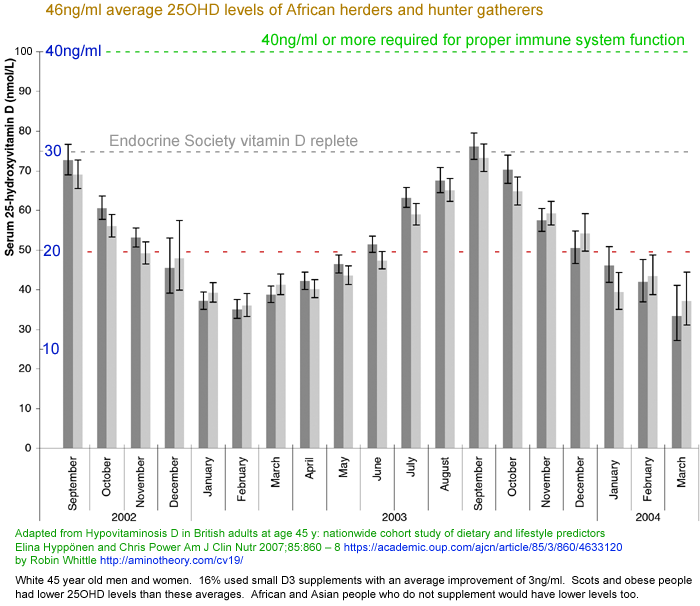
We are now entering a new phase of Mother Nature's crossover
trial, in which vitamin D is dropping - or will drop after September see
#2004-UK-vit-D below - in countries 40 to 60 degrees
north of the equator. So viral shedding, rates of infection and
(I assume) severity are - or will in or after September - all increasing as 25OHD vitamin D blood levels
descend again towards their winter nadir around February.
A possible explanation other than lockdowns and summer vitamin D levels:
It is possible that the upswing in daily “new cases” is partly or
wholly caused by increased use of antibody (and perhaps antigen) tests in the last month or
two. The original PCR tests detected viral RNA and so indicated current
or recent (weeks) infection. Assuming no false positives, antibody
tests are positive for people who were previously infected. A positive
antibody test for a person who was not previously PCR tested, or who
was and tested negative, may be counted as a “new case” even though
their infection may have been months ago.
For this pattern to significantly add to the “new cases” count,
significant numbers of such people – who are presumably no longer
symptomatic, and who may never have had more than mild symptoms – would
need to be presenting for an antibody test. To the extent that antibody
tests are widely deployed for such people and the results counted in
this way, the rise in “daily new cases” does not generally represent
people who were infected in the last week or so.
This explanation is advanced by biochemical engineer Ivor Cummings,
better known as
https://thefatemperor.com in this
2020-08-12 video:
Crucial Viewing – to truly understand our current Viral Issue #Casedemic https://www.youtube.com/watch?v=FU3OibcindQ
. He points to graphs of rising new cases with no matching rise in
deaths. I am unsure to what extent this explains the upswings in "new cases".
If summer vitamin D levels did suppress transmission significantly,
such as by reducing viral shedding, then the coming months - October to
December 2020 and to March 2021 - will show
this, because genuinely new cases will rise inexorably as average
vitamin D levels drop, (as will death rates) unless there is a return
to extreme lockdowns and perhaps in spite of those lockdowns.
While some extra vitamin D supplementation is presumably occurring now,
it is not enough to protect entire populations from winter declines in
vitamin D levels.
2020-08-31 update: BBC-2's Newsnight reports
https://www.bbc.co.uk/programmes/p08pz1fm
on a leaked
SAGE
(Scientific Advisory Group for Emergencies) report with a worst-case
prediction for 81,000 excess deaths directly attributed to COVID-19 and
27,000 excess deaths not related to COVID-19. Greg Fell, Public
Health Director for Sheffield said: "We know cases will rise into the
autumn and winter. There's no doubt about that." However,
there is no mention of vitamin D or the precise mechanisms which make
COVID-19, influenza or various common cold viruses (some of which are
also coronaviruses) seasonally more active in winter and spring.
He said that the reason the death rate remains low while new cases are
rising is that in the first wave, the mean age was in the mid to high
60s. (I assume he is talking about people who needed medical
care, but perhaps he means confirmed cases, which would be skewed by
low testing rates in younger people who felt they were not at risk of
bad outcomes.) Now the mean age is in the mid 30s to the early
40s. Fewer people need to be hospitalised and "almost zero" need
intensive care. (I don't have a clear idea of what is going on here or why the average age has dropped.)
#kp
The case for worldwide vitamin D supplementation
For links to the latest research into vitamin D, immunity and COVID-19, please see the
next section AND the new website
https://VitaminDStopsCOVID.info .
See also the section
#vaccines below where I argue that a
COVID-19
vaccine is absolutely the wrong approach. It doesn't even solve
the right problem. This virus is not the problem.
The problem is people's weakened and dysregulated immune systems - and
this already causes far more trouble than COVID-19 would cause even if
everyone in the world contracted the disease with their currently
generally weak and dysregulated immune responses.
The most concise, well-referenced,
business and moral case for an urgently implemented worldwide program
of vitamin D supplementation is
Karl Pfleger's
frequently updated essay. This was written and is maintained
entirely independently of this aminotheory.com material - so the vision
of supplementation it presents is not the same as what I am proposing.
While high vitamin D levels may protect somewhat against infection,
this is insignificant in the face of the highly contagious SARS-CoV-2
virus.
The first critical point is that
vitamin
D deficiency is the most important, easily correctable, cause of the
immune system weakness and dysregulation which drives COVID-19 harm and
death.
The second critical point is that
vitamin
D deficiency is the most important, easily correctable, cause of high
rates of viral shedding and so of rapid spread of SARS-CoV-2 infection.
A
worldwide program of vitamin D repletion can reasonably be expected to play a decisive and essential role in improving everyone's immune system health, so as to
render COVID-19 at most a nuisance, and (except perhaps for a some people with lung injuries or other severe health conditions)
no longer the serious, disastrous, cause of suffering, hospitalisation, harm and death which it is today.
Population-scale vitamin D supplementation can and should be
implemented sooner than any safe, effective, well-tested vaccine could
be widely deployed, with much greater safety , greater health benefits,
and lower cost.
You are reading a very long web page which has grown since late March. Here is my attempt at summarising
the
urgent need for worldwide vitamin D supplementation, aiming for all
babies, children, adolescents and adults to have 40 to 60ng/ml vitamin
D levels, with no great concerns that some people's levels will be twice these.
There is a growing body of epidemiological, clinical and cellular
evidence which shows that low vitamin D levels are a major cause of the
weakened and dysregulated (overly-aggressive, hyper-inflammatory,
self-destructive) immune responses which, in some people, cause the
severe symptoms of COVID-19, including the endothelial cell (blood
vessel lining) damage which causes the body to make the blood thick and
hyper-coagulative. This hypercoagulative state drives most of the
resulting damage, with microembolisms (tiny blood clots) forming in the
lungs, brain, heart, liver kidneys etc. along with heightened risk of
large blood clots in the brain (stroke) or the coronary arteries (heart
attack). Lasting harm and organ damage typically results from
this hypercoagulative state, which sometimes begins even in the
presence of relatively mild symptoms.
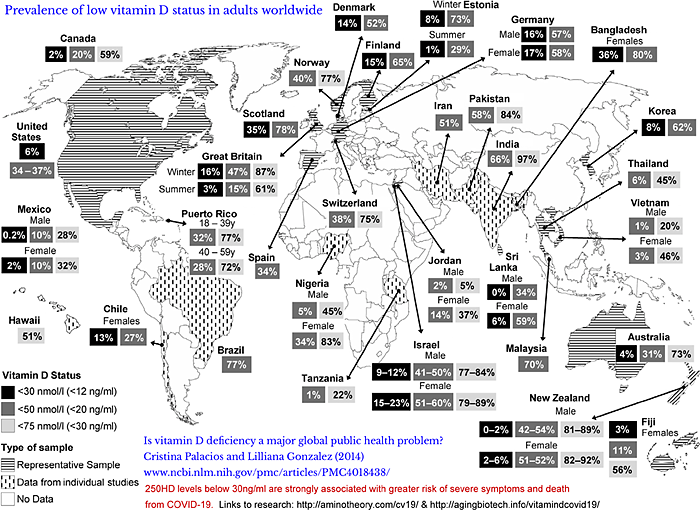
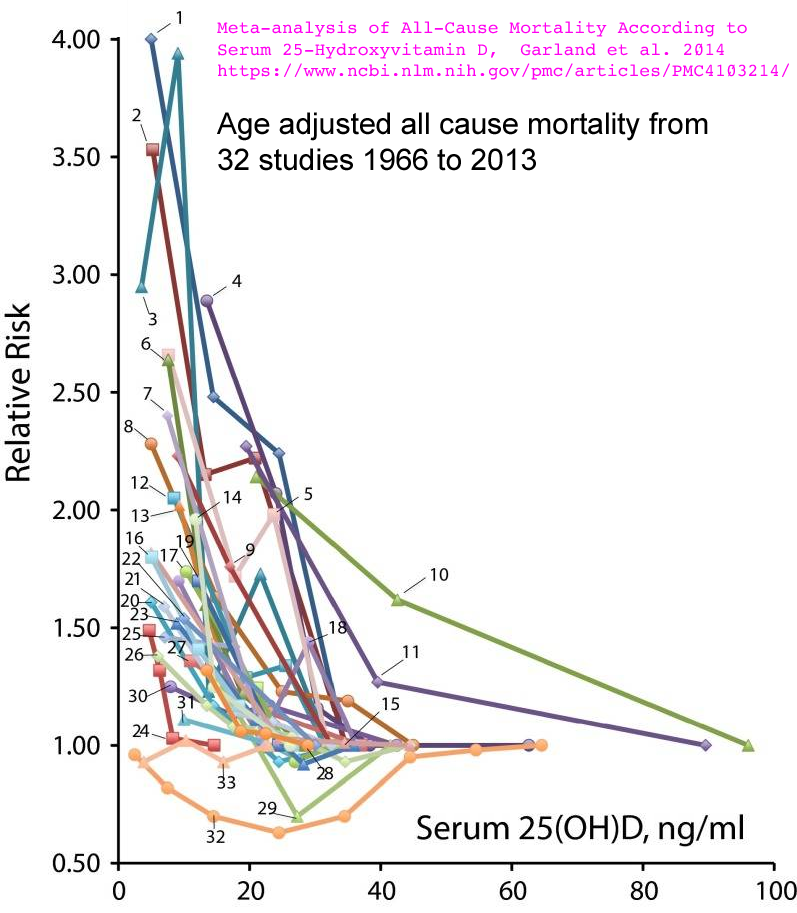
For decades, a growing body of research has documented the
global vitamin D deficiency pandemic. Since 2008 vitamin D specialist researchers and MDs have
recommended
that everyone should try to attain vitamin D blood levels (25 hydroxy
vitamin D, produced in the liver from ingested or UVB produced D3) of
40 to 60ng/ml
(100 to 150nmol/L) all year round. 100ng/ml is considered the the
high end of normal, but some people are perfectly healthy - indeed with
healthier regarding reductions in asthma and other diseases - with
higher levels. Toxicity - hypercalcemia which damages bone
and blood vessels - bone is possible above 150ng/ml but is most
likely to begin at higher levels still. Such levels cannot
be attained through sun or artificial UVB light exposure.
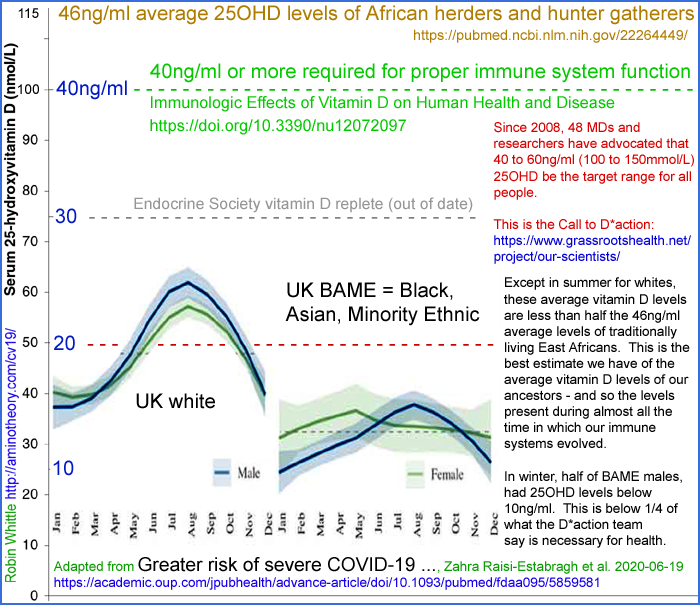
Without supplements most people's year-round average 25OHD levels are in the
10 to 25ng/ml range and are lower still in winter. The best estimate we have of the 25OHD levels of our ancestors is
46ng/ml - the average levels of traditionally living East
African Maasai herders and Hadzabe hunter gatherers:
https://www.ncbi.nlm.nih.gov/pubmed/22264449 . The internal (autocrine) signaling systems of many of our cells evolved to work with this supply of 25OHD.
As you can read below, some groups of people have 25OHD levels disastrously below
10ng/ml.
Yet UK government standards state that 10ng/ml is an adequate level and
many other countries, including the USA define vitamin D repletion as
20ng/ml 25OHD. The UK and US recommended supplemental D3 intake
for adults is 0.01mg (400IU) and 0.015mg (600IU), which are about a
10th of what normal weight adults, on average, need to attain
40ng/ml.
The Endocrine Society's standard for repletion is 30ng/ml.
Food - including fortified foods and drinks - and multivitamins contain
only small amounts of vitamin D. Pharmaceutical grade vitamin D3
(cholecalciferol) is produced industrially mainly in China and
India. The ex-factory 1kg lot price is around USD$2.50 a
gram. 0.125mg (5000IU) a day is sufficient to raise most normal
weight adults' 25OHD levels to at least
40ng/ml. At this rate, a gram lasts for 22 years. So raw cost of this healthy level of supplementation is
USD$0.12 a year.
D3 need only be taken every week or two, so it would suffice to supply
it as 52 capsules a year, each containing 0.875mg (35,000IU).
Babies and children need less, according to body weight.
Overweight and obese people need significantly more due to their
greater body weight and because D3 is absorbed by their greater
proportion of adipose tissue.
Ideally, all people would have ready and affordable access to their own
personal doctor who advises them according to the best research, and
who is able to order blood tests to monitor their 25OHD levels every
year or two. However, this is impossible for all 7.8 billion
humans, and the costs would vastly exceed those of the D3
supplements. Many doctors are either unaware of the best vitamin
D research and/or are constrained by government, professional
association, hospital and insurance rules and guidelines regarding
25OHD testing and the ideal blood levels and supplementation intakes
they can advise for their patients.
Dozens of chronic and acute diseases are caused by weak and dysregulated (over-inflammatory) immune systems, as listed below.
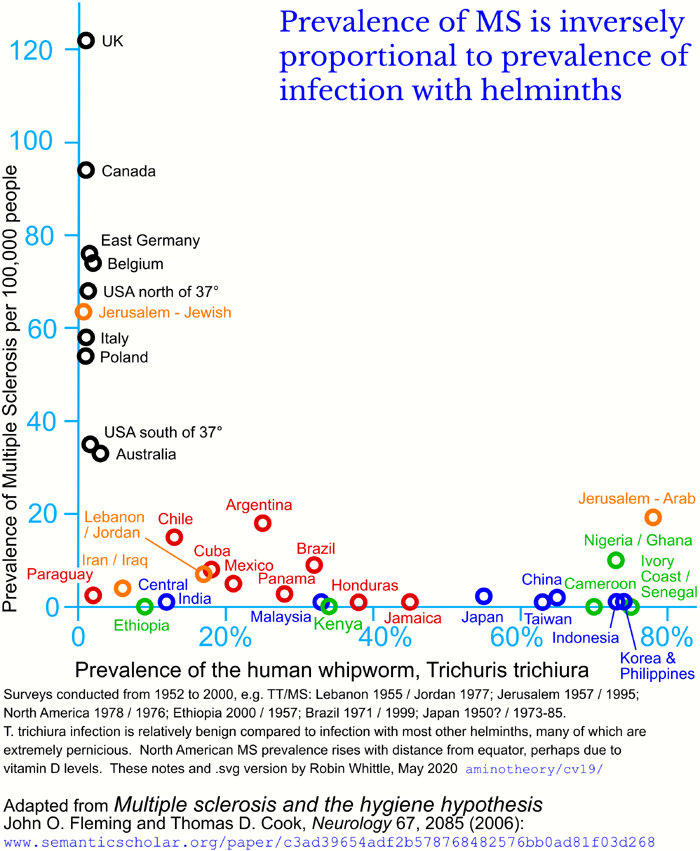
One primary cause of immune system dysregulation is - with considerable
genetic variation between individuals - that our immune systems evolved
to be more aggressively inflammatory than is desirable, because our
ancestors were all infected with helminths (intestinal worms), which
produce a variety of compounds which downmodulate many immune
responses. Now, with most humans being free of helminthic
infection, some of our immune responses are self-destructive. For
instance, patients with Crohn's disease (auto-immune destruction of the
intestines) go into remission when infected with the relatively benign
pig whipworm.
#helminthsgone . Some people, such as those with life-threatening asthma, infect themselves (
helminthic therapy)
to obtain relief. There is ongoing research into pharmaceutical
approaches to mimicking at least some of the helminths' downmodulatory
effects, but commercially available products for this are a long way
off.
The other primary cause of weakened and dysregulated immune systems is
nutritional deficiencies - and, arguably, an excess of salt.
Vitamin D deficiency is the best researched, most important and easiest
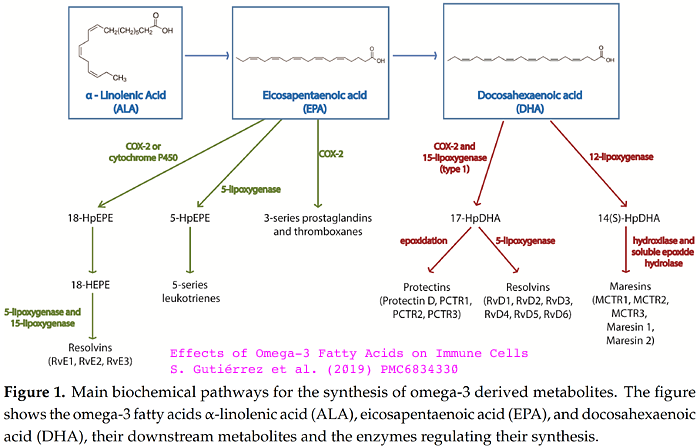
to correct of these. Inadequate omega 3 fatty acids (as found in
fish and algae oils) is probably the second most important, and can
easily be corrected - though the quantities needed and the annual cost
is much greater than for vitamin D.
Inadequate boron
#08-boron is also known to
drive overly inflammatory immune system dysregulation. Boron
supplementation is widely used to treat arthritis, and boron, as borax,
is appearing in some mass market multivitamins. However, despite
decades of research showing its importance to humans, and its routine
use in preventing bone and joint problems in pigs and other
agricultural animals, according to conventional (textbook and
nutritional guideline) understanding, boron has no role in the
nutrition of animals.
Boron, as borax, is readily available, inexpensive and very safe to use
in the 6 to 12mg per day range which would probably lead to repletion
(there are no standards for this, yet) and significant health benefits
over the typical 1mg daily intake of most adults.
Boron's half-life is ~22 hours, so small quantities need to be taken
each day. 12mg a day would require 36 grams of borax per year,
and it costs less than USD$0.01 per gram. Borax is a sodium
oxygen salt of boron. Large deposits of this mineral are mined in
Turkey and California, with relatively simple crystallisation
purification at the mine site,
Despite the vast amount of vitamin D research, many doctors remain
unaware of the benefits of repletion to at least 40ng/ml, or wary about
such levels because of outdated and overly cautious concerns about
toxicity. The pharmaceutical industry has no interest in
promoting vitamin D, since worldwide repletion would greatly reduce the
global burden of disease which drives most of its sales of high-profit,
patented, drugs. Boron research is generally unknown to doctors
and even to most vitamin D researchers.
Even in diseases where research has clearly established very low
vitamin D levels to be a distinctive - and no-doubt largely causative -
factor, including the childhood immune dysregulation disorder Kawasaki
disease
#2015-Stagi (now being triggered with much greater frequency by COVID-19), many doctors remain unaware
#kdarticles that vitamin D deficiency is involved, so they fail to test or replete their patients' vitamin D levels.
Potassium deficiency, especially in the context of excessive salt, is a
global problem which research shows beyond any doubt is the primary
avoidable cause of hypertension and stroke
kna/
. Potassium supplementation is challenging because of the
quantities involved - such as 2.5 grams potassium a day to
approximately double the normal intake. This is possible,
at the cost of around USD$100 a year, with potassium gluconate
solution, which has a very mild taste. However I have never
encountered a doctor who is aware of this. So many or most people
my age (I am a 1955 model) take expensive hypertension drugs, all of
which have significant ill-effects - and sometimes additional drugs to
counter those ill effects. Potassium supplementation and modest
avoidance of salt
solves the
problem of K / Na ionic balance in all cells of the body, removes the
primary causes of hypertension and stroke, and provides numerous other
benefits - no-doubt including immune system strength and regulation.
Iron is a well known nutritional deficiency, and many people are
deficient in vitamin C, magnesium and zinc. Here is a table
of the five nutrients whose common deficiency most contribute to immune
system dysfunction and general ill-health. A future website, to
be known as Five Neglected Nutrients, will cover these in greater
detail than is possible here.
Ideally we would replete all five, for all people on Earth, as a matter
of urgency - and that was the situation before COVID-19. Since
COVID-19 harm and death results only from a subset of the population
having weakened and dysregulated immune systems (in combination wit
genetic variation, obesity, advanced age and several comorbid
conditions)
it is absolutely
imperative that governments and doctors work together to replete
vitamin D and ideally some of the others, with an urgency which only
occurs in times of war.
Nutrient
|
Medical profession knowledge of mechanisms of the nutrient's benefits, and so of the problems caused by deficiency.
(Most doctors receive inadequate training in nutrition.)
|
Medical profession consensus on supplementation.
|
Practicality for global repletion in the coming months to render COVID-19 no longer a threat.
|
Vitamin D
|
Vast amount of research, yet not very well known except to a subset of doctors who are well aware.
|
General
disinterest and some controversy - with a small, growing, number of
doctors adamantly promoting vitamin D repletion for general health and
protection from COVID-19 harm and death.
|
Practical,
safe, inexpensive and absolutely vital for general health and for
reducing COVID-19 severe symptoms and the rate at which the disease spreads. New D3 factories are urgently
required.
|
Omega 3 oils
|
Good research on immune system benefits, though not very widely known.
|
General
disinterest and some controversy - again with some doctors in
favor. No controversy about safety - so should be used by all who
have it available.
Would surely help with COVID-19, but there is no research to quantify this.
|
Impossible
to quickly scale up fish or algae oil production to meet needs of grams
a day per 7.8 billion persons. 2g/day 6 billion adults = 4.4
million tonnes / year.
|
Boron
|
Good research, but precise cellular mechanisms not yet well understood.
Not recognised as a nutrient. Most doctors have never heard of it, although it is used to reduce or prevent arthritis.
See #08-boron .
|
Only a handful of doctors are aware of it.
Would surely help with COVID-19, but there is no research to quantify this.
|
Readily available as borax, very inexpensive, safe and easy to ingest in water solution.
However, doctor's general ignorance of this and widespread
misconceptions about its toxicity make boron supplementation
challenging in the short time frame we have to render COVID-19 no longer
a threat.
|
Vitamin C
|
Very well researched and recognised.
|
Controversy
about dosage, with some high dose protocols probably unnecessary for
most people, while providing benefits for some.
Dr Paul Marik's 10g/day IV vitamin C MATH+ protocol for ICU patients, including especially those with COVID-19, remains controversial despite obvious benefits.
|
Production
could be increased somewhat, but I suspect it would be best to keep
limited vitamin C in reserve for people who are COVID-19 positive so
they can use multi-gram quantities a day and hopefully stop the virus
from infecting their lungs.
|
Potassium
|
Excellent research on hypertension and stroke, but not widely known.
Fundamental importance to ionic balance of all cells is well established, but not widely recognised by doctors.
See kna/ .
|
Virtually
all doctors and, as far as I know, most researchers assume that
potassium supplementation is impossible due to the strong taste of the
salts. They do not know about potassium gluconate's mild taste.
Doctors are coached heavily in the dangers of excessive intravenous
potassium supplementation since the body can only handle limited
quantities at any one time. Overdoing it, including by drinking
excessive potassium gluconate at any one time, will raise blood
potassium too much before the cells absorb it and so cause potentially
deadly heart problems.
|
No prospect of ramping up potassium gluconate for global needs except over many years.
There are safety concerns with such supplementation being taken too quickly, so it needs to be spread throughout the day.
These problems - and many doctors being alarmed at the prospect of
patients drinking a potassium solution - mean that progress towards
global potassium repletion needs to be made cautiously and not at all
in the current crisis.
|
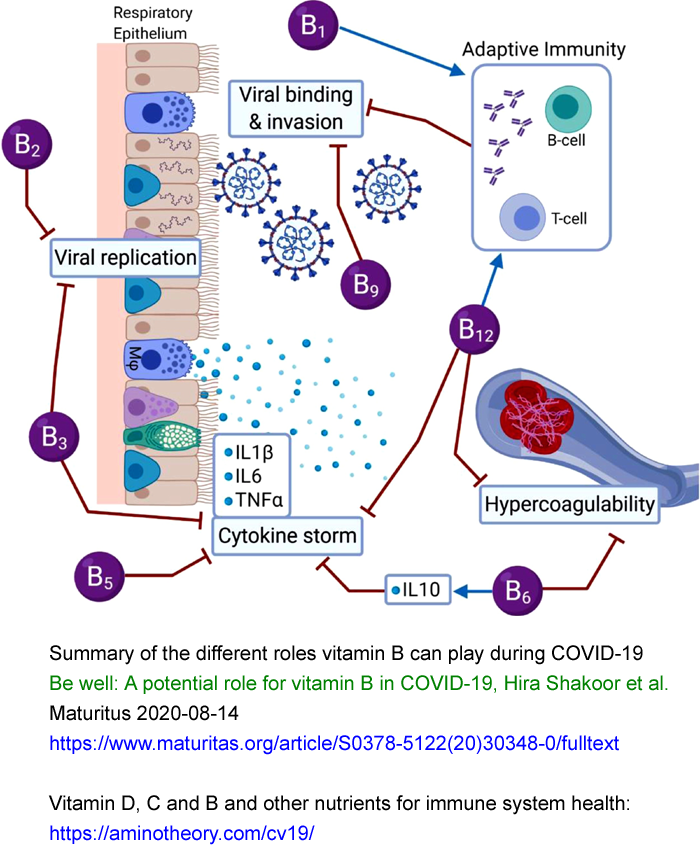
See also this article on vitamin B:
https://www.maturitas.org/article/S0378-5122(20)30348-0/ .
The best, post-COVID-19, review article on vitamin D recommends
40 to 60ng/ml 250HD
levels. It is co-written by Michael Holick MD, who has been
researching vitamin D since 1971, and is the foremost vitamin D
researcher, with Google Scholar reporting 129,193
citations of his articles:
Immunologic Effects of Vitamin D on Human Health and Disease
Nipith Charoenngam, Michael F. Holick 2020-07-15
Nutrients 2020, 12(7), 2097
https://doi.org/10.3390/nu12072097
|
From a 2019 article (24
citations):
Vitamin D is essential for internal (autocrine) signaling in may cell
types, including especially those of the immune system which both
attack pathogens and regulate such actions:
The
exact number of gene products controlled by vitamin D3 is unknown, but
the active hormone form of vitamin D3 was recently found to bind via
its receptor to 2776 distinct binding sites in a human cell line, many
of which were located near autoimmune and cancer associated genes.
|
Both these articles list diseases for which vitamin D is a significant
contributing cause (or at least of severe symptoms, as with
COVID-19). The two lists combined result in:
Alzheimer’s disease.
Asthma.
Atopic dermatitis.
Autoimmune diseases such as Cohn’s disease, inflammatory bowel
disease, multiple sclerosis, psoriasis, posoriatic arthritis,
rheumatoid arthritis and ulcerative colitis.
Cancers including breast, colon, prostate, sarcomas and skin cancer.
Chronic pain.
COVID-19 - hyperinflammatory response.
Dementia = neurodegeneration.
Depression.
Diabetes types 1 and 2.
Epilepsy.
Falls, fractures and muscle weakness.
Fibromyalgia.
Hypertension.
Muscle pain and proximal muscle weakness.
Osteoarthritis.
Parkinson’s disease.
Pregnancy complications including premature birth and death.
Respiratory infection.
Rickets (Failure to develop strong bones in childhood.)
Osteomalacia (Softening of bones, mainly in children and young adults.)
Osteoporosis (Low bone density, mainly in old age.)
Schizophrenia.
Seasonal affective disorder.
Sepsis.
Tuberculosis.
Urticaria.
Vitiligo.
Wheezing disorders.
So there has long been an urgent need for global vitamin D
repletion. COVID-19 makes it the most urgent and important
step humanity can take to combat the disastrous severe complications
which COVID-19 elicits in a substantial subset of the population whose
immune systems are weak and dysregulated.
Latest research concerning COVID-19, immune system regulation, vitamin D and other nutrients
This section has not been updated for a while. Please see:
These are sorted roughly with the most
significant articles first. Please see the dates if you are
looking for updates since you last viewed this list. If you
only read five articles, please read those listed first
[A],
[B],
[C],
[D] and
[E].
https://aminotheory.com/cv19/icu/#2020-McGregor [A]
I regard this as the most important COVID-19 article of all.
New summary 2021-03-09:
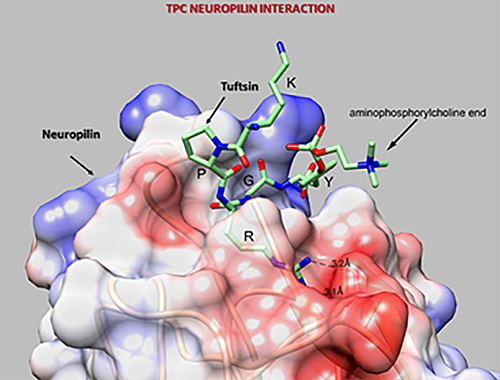
Th1 lymphocytes isolated from the lungs of patients with
severe COVID-19 symptoms have an autocrine (https://vitamindstopscovid.info/02-autocrine/) signaling pathway
which should be
activated by high levels of complement (WP), to turn these cells off their initial hyper-inflammatory
program which produces pro-inflammatory IFNγ (interferon_gamma WP
which has antiviral and anti-bacterial activity as well as stimulating
inflammation: cell destruction such as by natural killer cells WP) and instead cause them to produce the anti-inflammatory cytokine IL-10.
(The cells always produce both these cytokines, but this transition to
a shutdown, anti-inflammatory program, involves less IFNγ and a lot
more IL-10.)
However,
this anti-inflammatory pathway is not working in the Th1 cells from patients with severe COVID-19, due solely to insufficient 25hydroxyvitaminD3 = 25OHD = calcifediol for each cell's autocrine signaling system to function. (Until 2021-03-01 I mistakenly stated that the Th1 cells initially produced IL-17 - and that the experimenters restored the Th1's anti-inflammatory pathway by adding 25OHD in-vitro.)
This is a molecular and cellular explanation for why people with
low vitamin D have wildly dysregulated, overly-inflammatory (cell
killing), self-destructive immune responses. Such responses drive
sepsis, severe influenza, Kawasaki disease (KD WP), Multisystem Inflammatory
Syndrome (MIS discussion) and of course severe COVID-19. (See Paul Marik's explanation https://www.evms.edu/covid-19/covid_care_for_clinicians/ of how it is the immune response, not the virus, which causes the escalation to severe symptoms and death. See #2015-Stagi for research which shows KD children have very low 25OHD vitamin D levels.)
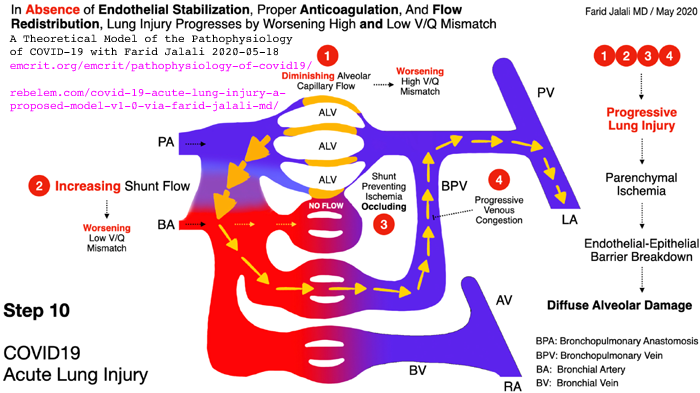
In severe COVID-19, severe inflammation in the lungs damages
endothelial cells (the inner lining of blood vessels and capillaries WP)
leading to hypercoagulative blood, causing microembolisms and larger
clots all over the body, which cause most of hypoxia, lasting harm and
death.
It is not known whether the cause of all
the hyper-inflammatory immune system dysregulation - which causes some
COVID-19 sufferers people to develop
severe symptoms - is primarily the failure of these Th1 lymphocytes to
switch from being pro- to anti-inflammatory,
or whether this endothelial cell destruction etc. is also driven to a
significant degree by similar failures in the autocrine signaling
systems of many other
types of regulatory and/or directly anti-pathogen immune cell.
However, the determination of
the exact mechanism of failure in Th1 cells, in the context of such failures likely
also occurring in other cell types, is an extraordinarily valuable
contribution which deserves to be very widely known.
Low
vitamin D levels (low circulating 25OHD, produced in the liver
from UV-B-generated and/or ingested vitamin D3 cholecalciferol) are
well known to reduce the effectiveness of numerous direct,
anti-pathogen, responses by the innate immune system cells and to
hinder the creation of antibodies for adaptive immune responses. These
immune functions of vitamin D 25OHD are due to it being needed, in the
circulation, at higher levels than are sufficient for bone health
(sufficient for the kidneys to produce their much lower concentration
of circulating - and so hormonal - 25OHD), to
supply the autocrine / paracrine (inside the cell / to nearby cells)
signaling systems of all types of immune cells. All types of immune
cell can express the vitamin D receptor - and this is for
autocrine/paracrine signaling - not for responding to the much lower
levels of circulating 1,25OHD which regulates
calcium-bone metabolism. https://vitamindstopscovid.info/02-autocrine/#02-nothorm .
See http://aminotheory.com/cv19/#2020-Fabbri [B] for why 40ng/ml or more 25OHD is required for these autocrine signaling systems to function properly. See also the Quraishi et al. graph https://vitamindstopscovid.info/02-autocrine/#04-quraishi
which suggests that innate immune cell responses which fight bacterial and perhaps fungal infections keep improving,
presumably due to faster and stronger autocrine/paracrine signaling, as
25OHD levels rise, up to about 55ng/ml.
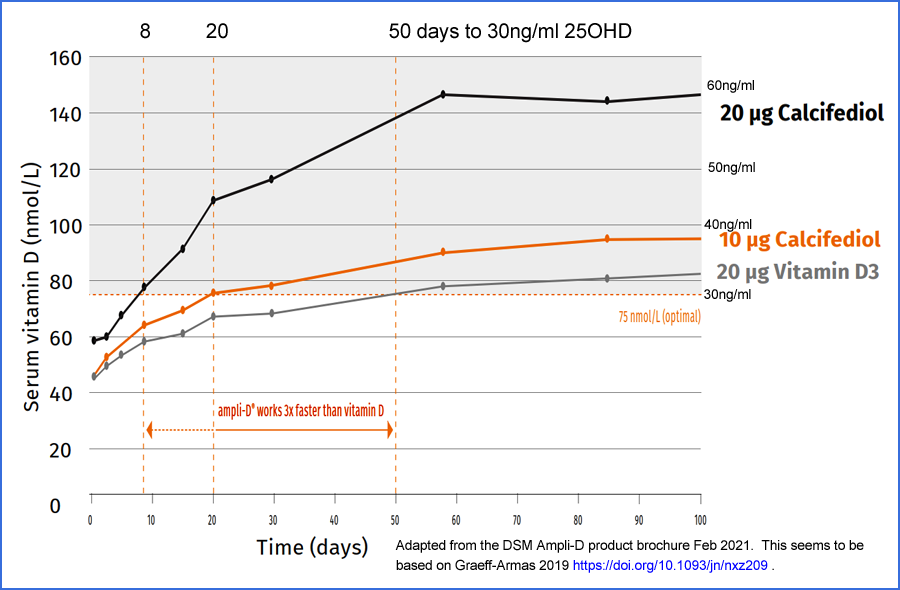
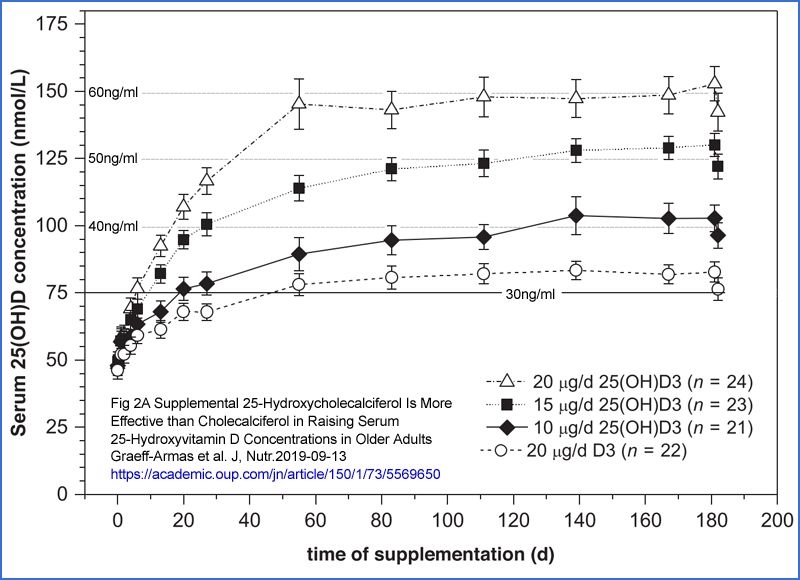
Please also see #25plusD3
for my suggestion of oral calcifediol (25OHD) plus D3 as the best
treatment for hospitalised COVID-19 patients, since this raises
circulating 25OHD to the levels needed for autocrine / paracrine
signaling in a few hours, rather than in the several days to a week
with vitamin D3.
For a more detailed summary of the McGregor et al. article, please see https://aminotheory.com/cv19/icu/#2020-McGregor .
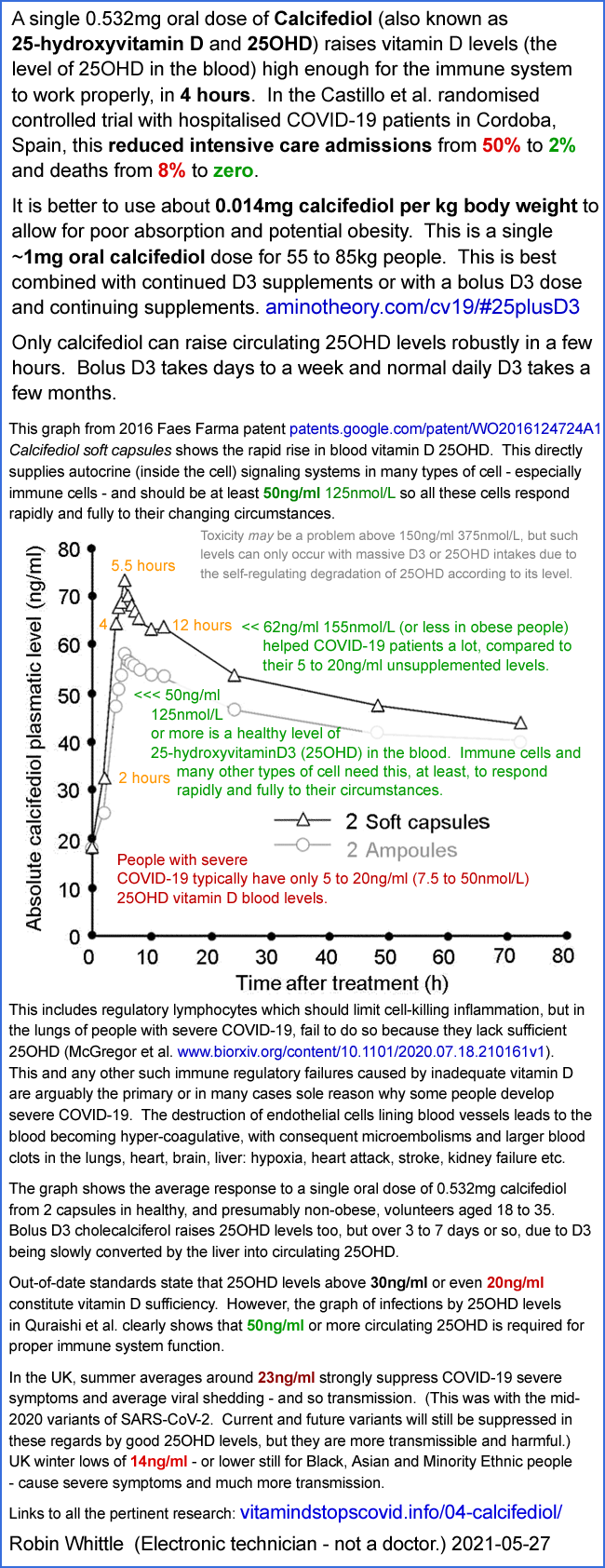
Very strong clinical evidence of the importance of rapidly raising
circulating 25OHD levels hospitalised COVID-19 patients can be found the Cordoba calcifediol (25OHD) RCT: Castillo et al. 2020: #2020-Castillo .
A Cordoba, Spain, vitamin D
supplementation trial for hospitalised COVID-19 patients used
fast-acting 25OHD calcifediol instead of they usual D3, which takes
some days to be converted to 25OHD in the liver. Without vitamin
D, 50% of patients needed intensive care and 8% died. With
vitamin D, only 2% (one of 50) needed intensive care and none died.
I think this is the most significant vitamin D supplementation COVID-19
trial and that it should lead doctors all over the world to implement
vitamin D3 supplementation programs for their patients and the general
public, as well as early supplementation with immediately available
25OHD calcifideol for patients entering hospital.
Update - a graph from a patent shows how oral 25OHD calcifediol as used in Cordoba raises blood 25OHD levels over
60ng/ml 150nmol/L within 4 hours, rather than 4 or more days as would bolus D3.
See also
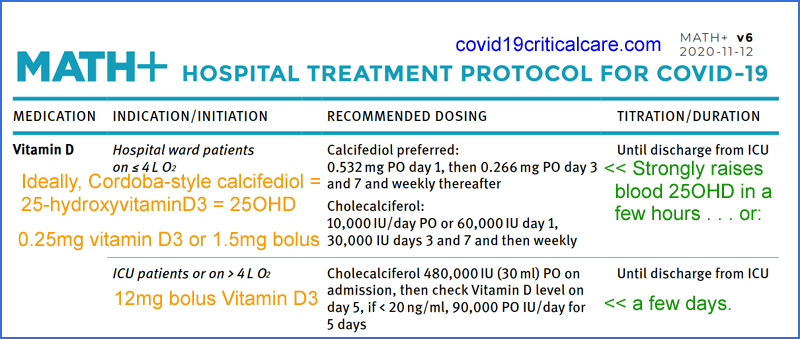
https://aminotheory.com/cv19/#25plusD3 for news about Paul Marik and Colleagues'
MATH+ Protocol now
(from 2020-11-12) recommending the exact same 25OHD dosing arrangements
as the Cordoba trial, and my suggestion that just the initial 25OHD
dose be done
with bolus D3.
https://aminotheory.com/cv19/#2015-Stagi [D]
Italian researchers in 2015 report that children with
Kawasaki Disease were, on average, "severely vitamin D
deficient".
The patients were 21 girls and 58 boys, average age 5.8 years.
Their average 25OHD levels were 9.2ng/ml, while age-matched
controls averaged 23.3ng/ml. In the patients who developed
coronary artery abnormalities, the average 25OHD level was 4.9ng/ml
(sd 1.36).
These children were struggling to live with vitamin D 25OHD in
their bloodstream 20% to 11% of what is normal (46ng/ml) for
traditionally living Maasai pastoralists and Hadzabe hunter gatherers in Africa - https://www.ncbi.nlm.nih.gov/pubmed/22264449
- the best estimate we have for the 25OHD levels of our
ancestors, in whom our current immune systems evolved.
https://aminotheory.com/cv19/#kdarticles
In June I found 18 articles on Kawasaki disease and
COVID-19. None of them mentioned vitamin D. It seems that
many or most doctors cannot imagine that vitamin D deficiency is
an essential causative element in KD, even though they should
all know that vitamin D deficiency causes immune system
dysregulation and that KD is immune system
dysregulation.
https://aminotheory.com/cv19/#2020-Afshar [E]
Iranian MDs in Dubai, UAE, recommend D3 supplemental
intakes as a ratio of bodyweight, with ratios in the range I derived
from the work of Ekwaru et al. 2014: https://vitamindstopscovid.info/01-supp/ .
They state that 40ng/ml 25OHD should be the threshold of deficiency and that the normal (they mean healthy) range should be regarded as 40 to 100ng/ml (100 to 250nmol/L. COVID-19 patients with 25OHD levels above 40ng/ml spent no more than 3 days in hospital and did not require intensive care.
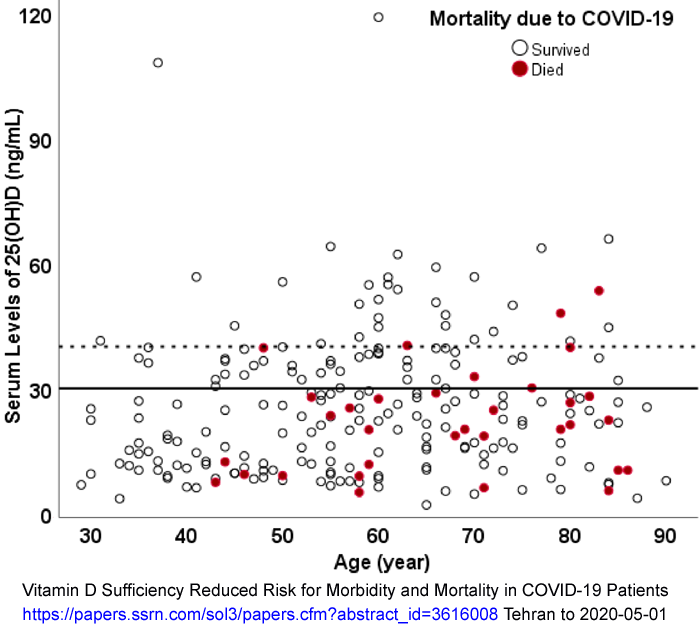
Iranian research finds respiratory patients who died of COVID-19 had only 8.2ng/ml while those who did not have COVID-19 averaged 30.2ng/ml.
https://aminotheory.com/cv19/#2020-Rastogi
2020-11-15: In hospitalised COVID-19
patients who are asymptomatic or have (initially at least) only mild
symptoms, and who have no comorbities and 25OHD levels below 20ng/ml, a
7 day (or longer if required to reach 50ng/ml 25OHD) program of bolus dosing: 1.5mg 60,000 IU vitamin D for 7 days (10.5mg
420,000 IU over 7 days) resulted in 62.5% of the supplementation group
clearing the viral infection by 21 days, compared to 20.8% of the
unsupplemented patients.
https://aminotheory.com/cv19/#25plusD3
2020-11-15: My suggestion for combining
a bolus D3 dose regime, such as that of Han et al. with a Cordoba style
(Castillo et al.) ~0.5mg 25OHD calcifediol dose given at the earliest
opportunity. Both have been shown to be highly effective and
safe. The two complement each other, so the combination should be
even more effective - and just as safe. I call this the
25plusD3 protocol
for COVID-19, severe influenza and
sepsis. This is the suggestion of an electronic technician.
It will be a real protocol when some MDs and/or researchers support it.
See also my proposed
Vitamin D supplemental intake as a ratio of bodyweight :
https://VitaminDStopsCOVID.info/01-supp/ .
2020-11-20: An Indian hospital observational study
of the correlation between low vitamin D levels and COVID-19 severity
and death, using two groups: those who were asymptomatic at admission
and those who were admitted to intensive care at admission.
https://aminotheory.com/cv19/#2020-Panagiotou
In Newcastle upon Tyne, hospitalised COVID-19 patients had
low vitamin D levels on admission. Some of the predominantly
white patients had levels below the 3.2ng/ml detection limit!
Those assigned initially to the ICU had lower levels than
those initially assigned to the general wards.
Israeli researchers find a modest difference in average 25OHD
levels between COVID-19 PCR positive patients who need
hospital treatment and those who don't. This is much more
statistically significant than the difference found in the
Newcastle upon Tyne study.
https://aminotheory.com/cv19/#2020-Maghbooli
Iranian researchers, with Michael Holick as co-author, report
highly significant correlations between "vitamin D
insufficient" < 30ng/ml 25OHD and "sufficient" >=
30ng/ml levels in respect of symptom severity, inflammatory
biomarkers and death.
https://aminotheory.com/cv19/#2020-Baktash 2020-08-29
Researchers in Slough, west of London, find elderly COVID-19 patients have median 25OHD levels of only 10.8ng/ml.
https://aminotheory.com/cv19/#2020-Shakoor 2020-08-29
Vitamin B1 thiamine, B2 riboflavin, B3
nicotinamide / niacin, B4 pantothenic acid, B6 pyridoxine, B9 folic
acid / folate and B12 cobalamin play important roles in the immune
system and so are important in reducing COVID-19 severity.
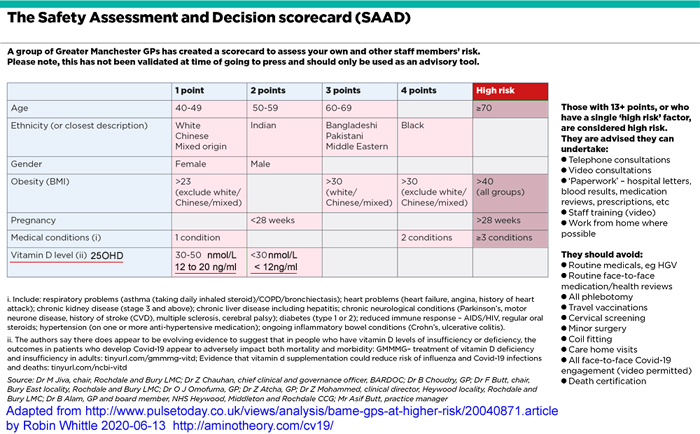
https://aminotheory.com/cv19/#SAAD
UK BAME doctors recognise 25OHD below 20ng/ml as a
risk factor for severe COVID-19 symptoms.
https://aminotheory.com/cv19/#haplotypes
A haplotype on chromosome 3 confers a high risk of severe
COVID-19 symptoms. It is apparently inherited from
Neanderthals, rare in Africans, common in Europeans and most
prevalent in Bangladeshis.
https://aminotheory.com/cv19/obesity/
- Excessive numbers of adipocytes (fat cells), such as in the
abdomen and in the fatty lining of the heart.
- These adipocytes expressing ACE2 on their surfaces, so
making them able to be infected by SARS-CoV-2.
- These adipocytes creating pro-inflammatory signaling
molecules, worsening the cytokine storm of overly-aggressive,
dysregulated, immune response which causes severe COVID-19
symptoms.
- Ectopic adipocytes in
the lungs, other organs and muscles.
https://aminotheory.com/cv19/icu/#2020-Bilezikian
A 2020-08-04 review article on Vitamin D and COVID-19 observations and mechanisms.
Here are some brief notes on research I intend to write about more when I have time:
2020-08-07
Linda L. Benskin's extensive review:
A Basic Review of the Preliminary Evidence that COVID-19
Risk and Severity is Increased in Vitamin D Deficiency
This includes unqualified references to fake articles by Alipio,
"Raharusun" and "Glicio". I notified the author before
publication, but the references are still there. See
https://researchveracity.info/alra/ .
News and updates
2020-07-14: If you are
seriously interested in vitamin D and COVID-19 - and more broadly in
Nutrition for Immune System Health - please consider subscribing to this
private email discussion list, with web-based searchable archives. This is the
NISH list at groups.io:
This is intended for doctors, nurses, researchers, health authority
advisers etc. as well as people such as myself with no formal
qualifications or direct involvement in healthcare. It is for
people who actively seek out, evaluate and discuss the latest research
and wish to work with others to facilitate research and understanding
of the likely role vitamin D supplementation has in reducing the risk
of COVID-19 severity. (Vitamin D supplements will not
significantly affect the risk of infection but will probably reduce the
rate of viral shedding, and so the chances of infecting others.)
Please see these excellent pages listing the
latest vitamin D and COVID-19 research:
http://agingbiotech.info/vitamindcovid19/ and
https://github.com/GShotwell/vitamin_d_covid . The authors of these pages are keeping up with developments faster than I can.
The first of these, by
Karl Pfleger, is much more than a list of research articles. It is a
detailed, coherent, argument for vitamin D supplementation
for many well researched reasons of enormous importance to health, with
COVID-19 making this need even more crucial and urgent.
(However, it is tricky to print:
Neither Firefox or Chrome
would print it. I had to select the whole page, copy it into
Word, make a narrower right margin and then resize come graphics before
I could print it.)
2020-07-22:
Th1 lymphocytes isolated from the lungs of patients with
severe COVID-19 symptoms have an autocrine (internal to the cell
W) signaling pathway which
should
be activated, to turn the cells off their hyper-inflammatory program
and instead make them produce the anti-inflammatory cytokine
IL-17. However, this
anti-inflammatory pathway is not working, due to lack of vitamin D. Please see
icu/#2020-McGregor for a summary and a link to the research article.
2020-07-25: Please see the
Newcastle upon Tyne (northern England) article
#2020-Panagiotou
below. It is the first report I read showing the
correlation between
low vitamin D levels in hospital patients and more
severe COVID-19 symptoms.
Also, an Israeli article
#2020-Merzon
reporting lower 25OHD levels for COVID-19 PCR positive people who need
to be hospitalised vs. those with milder or no symptoms. Neither
of these articles reports a dramatically strong association, but in the
scheme of things, with millions of people being infected, the
difference between low and moderate levels of vitamin D makes a big
difference, and raising the 25OHD levels of the population, before
infection, to something healthy, such as 40 to 60ng/ml would surely
result in a still greater reduction in symptom severity. The
Israeli sample is larger and the correlation is much more significant
(p < 0.001) then in the Newcastle sample (p = 0.3).
In the UK,
NICE have released their report which states there is no reason to believe that low vitamin D levels are causing
severe COVID-19 symptoms:
COVID-19 rapid evidence summary: vitamin D for COVID-19, Evidence summary [ES28] 2020-06-29:
This is obviously mistaken. I plan to write a response here, but
I have to give priority to paying work. Dr David Grimes has a
critique of the NICE report (but I consider the Filipino and Indonesian articles he mentions are fake:
#2020-Alipio).
#Fauci
2020-09-11: In a
report on a 2020-09-10 Instagram
interview (viewed by 1.7 million two days later) with
Dr Fauci, he states that he takes vitamin D and vitamin C:
If
you're deficient in vitamin D, that does have an impact on your
susceptibility to infection. I would not mind recommending, and I do it
myself, taking vitamin D supplements. The other vitamin that
people take is vitamin C because it's a good antioxidant, so if people
want to take a gram or so of vitamin C, that would be fine.
|
#haplotypes
I have only briefly looked at this article
The major genetic risk factor for severe COVID-19 is inherited from Neandertals https://www.biorxiv.org/content/10.1101/2020.07.03.186296v1 which suggests that a Neanderthal gene haplotype [
W]
drives an overly-inflammatory response which is known to cause severe COVID-19
symptoms, and that this haplotype is much more common in some races (though they
do not use this term). This haplotype is rare in Africans, moderately prevalent in Europeans,
and common in some South Asian populations:
The highest frequency
occurs in Bangladesh, where more than half the population (63%) carries
at least one copy of the Neandertal risk variant and 13% is homozygous
[has both of their chromosome 3s carrying it] for the variant.
|
This does not relate directly to vitamin
D (as far as I know - though
perhaps
the haplotype mediates its ill-effects partly via low vitamin D
levels), but when considering low vitamin D as a cause of severe
COVID-19
symptoms, which is very common in people with brown or black skin, who
live far from the equator, we should consider that genetic factors such
as this may also play a role.
The above URL also has extensive comments on the article. The
article in which this haplotype is identified as a risk factor in
patients in Italy and Spain is: Ellinghaus et al. (over 100
co-authors):
https://www.nejm.org/doi/10.1056/NEJMoa2020283 .
2020-07-02: I have been unable to
disprove my hypothesis that
two widely-cited non peer reviewed articles
concerning vitamin D and COVID-19, from the Philippines and Indonesia, are invalid. - and I found lots of evidence to support it. Likewise a third article from India. See my new site:
for a detailed account of why I believe these articles are
fabricated. Please do not take my word for it - read the above
account and make up your own mind. I am not an authority.
Vitamin D basics:
See also a concise introduction to the three vitamin D compounds, D3 25OHD and 1,25OHD at
https://VitaminDStopsCOVID.info/#d .
Since 2008, four dozen medical doctors and researchers have been advocating for
40 to 60ng/ml
(100 to 150ng/ml) 25OHD vitamin D levels to be recognised as necessary
for health in general - and particularly regarding the immune
system. This is the
Call to D*Action:
A recent review also supports 40 to 60ng/ml 250HD levels:
Immunologic Effects of Vitamin D on Human Health and Disease
Nipith Charoenngam, Michael F. Holick 2020-07-15
Nutrients 2020, 12(7), 2097
https://doi.org/10.3390/nu12072097
|
Also, Barbara A Gilchrist's 2008 article
Sun exposure and vitamin D sufficiency
on why sun exposure of artificial ultraviolet light capable of raising
vitamin D always involves DNA damage and so increased risk of
cancer. Exposure to about 1/3 the UVB light required to produce a
little sunburn is all that is required each day to maximise vitamin D
production in the skin. In general, it is best to avoid sun or
other UVB exposure and instead rely on nutritional supplements, since
there is not enough vitamin D in food to achieve vitamin D
repletion.
She argues for a lower target than 40 to 60ng/ml - but that was before 2012
research
which provides the best estimate we have for the 25OHD levels of our
African ancestors - the level which our immune systems evolved to work
with. The average vitamin D level of traditionally living East
African Maasai herders and Hadzabe hunter gatherers is
46ng/ml (115nmol/L):
https://www.ncbi.nlm.nih.gov/pubmed/22264449 .
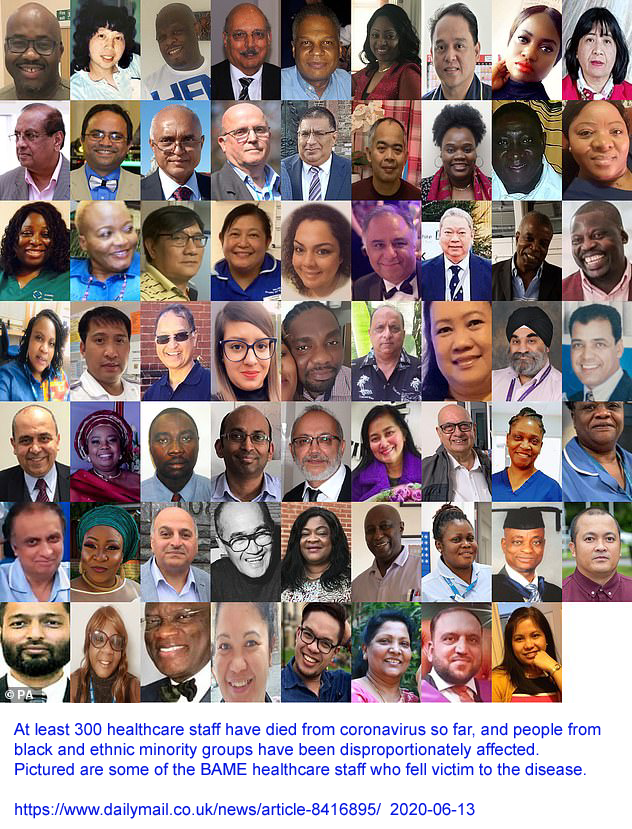
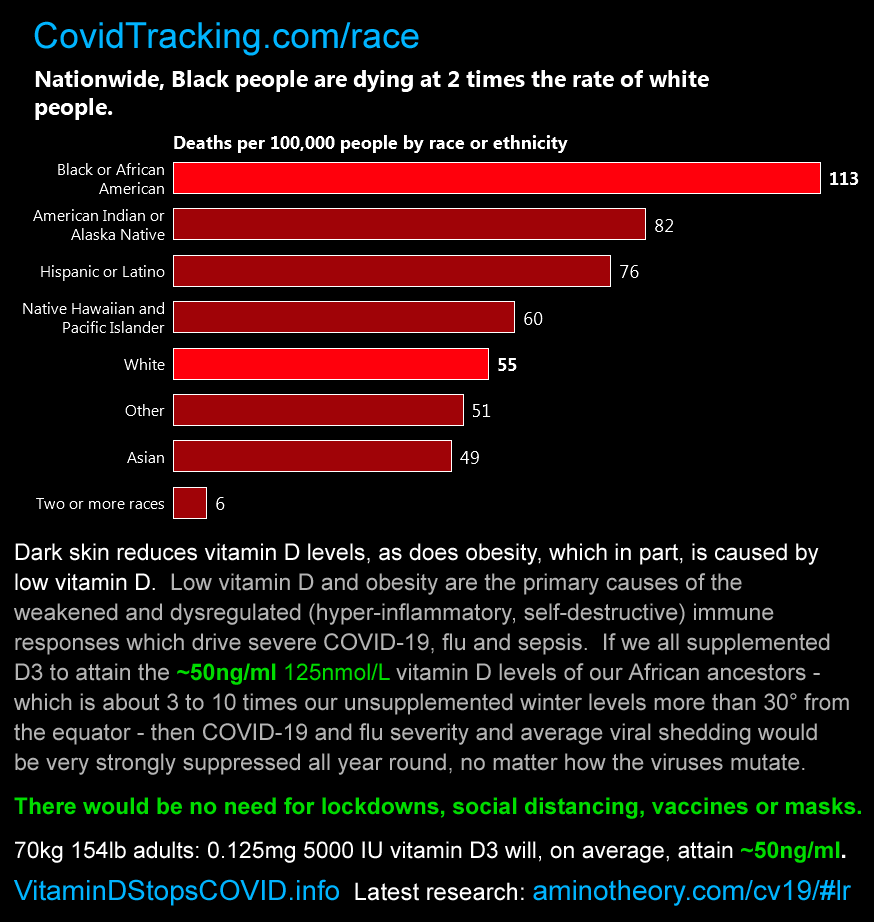
As you will read below, there is a relationship between low
vitamin D levels and severe symptoms,
lasting harm and death among adults with COVID-19. This is
surely a significant reason contributing to the greater toll of harm
and death suffered by people with dark and black skin
especially
when they are living far from the equator. The same is true of
children who suffer from Kawasaki disease, which can be triggered by
numerous viral and bacterial infections, including especially
COVID-19. Italian research
#2015-Stagi
shows they have very low vitamin D levels: 9.2ng/ml - and 4.9ng/ml for
those with coronary artery artery damage. Most doctors have been
unaware of this important research.
One of the Call to D*Action researchers, William B. Grant PhD, wrote an
article in 2018 about what he - and I guess his colleagues - perceive
as a series of unfair actions and biases frustrating their efforts to
have official guidelines about vitamin D supplementation doses and
desired 25OHD blood levels revised to match what is now known about
vitamin D and health, especially immunity:
I think that "orthomolecular" is an awkward term for a field in which
nutrition is given greater prominence for disease prevention and
perhaps cure than is common in Western medicine. While there may
be some arguments in this field which I consider not properly based on
observations or experiments, the fundamental tenet is obviously
sound.
In electronic engineering, the equivalent tenet would be "Battery
voltages, external power voltages and all internal power supply
voltages must remain with specified ranges before the equipment can be
expected to perform reliably".
"Orthomolecular" medicine is only necessary because Western medicine - as practiced by many, probably most, but not all doctors - has such blind-spots regarding nutrition, and such a keen eye for using drugs instead.
#vitd-autocrine
Vitamin D in autocrine and paracrine signaling
2020-11-23: Please see this new, illustrated, page on the new website:
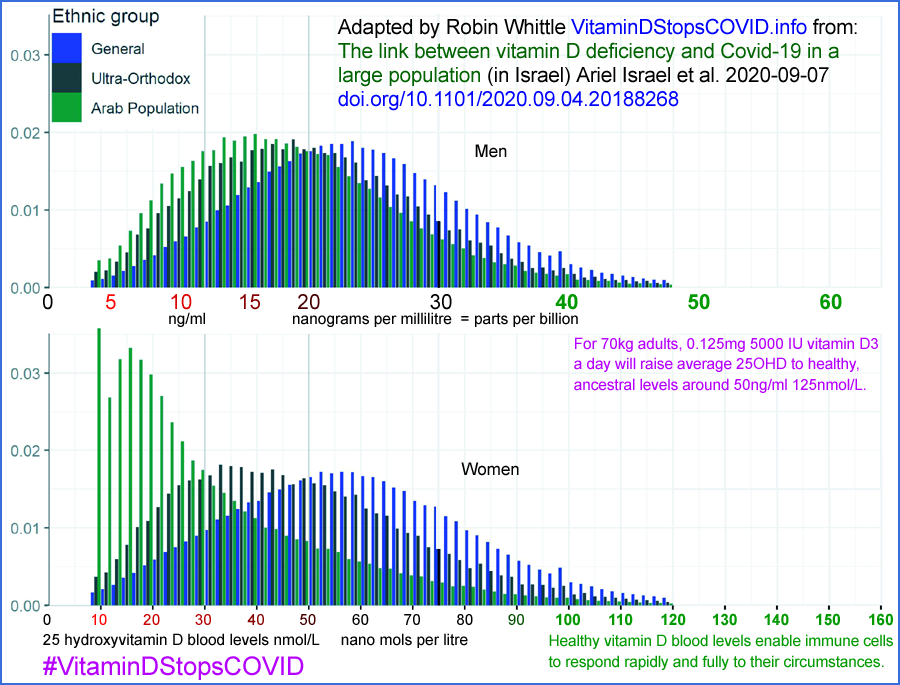
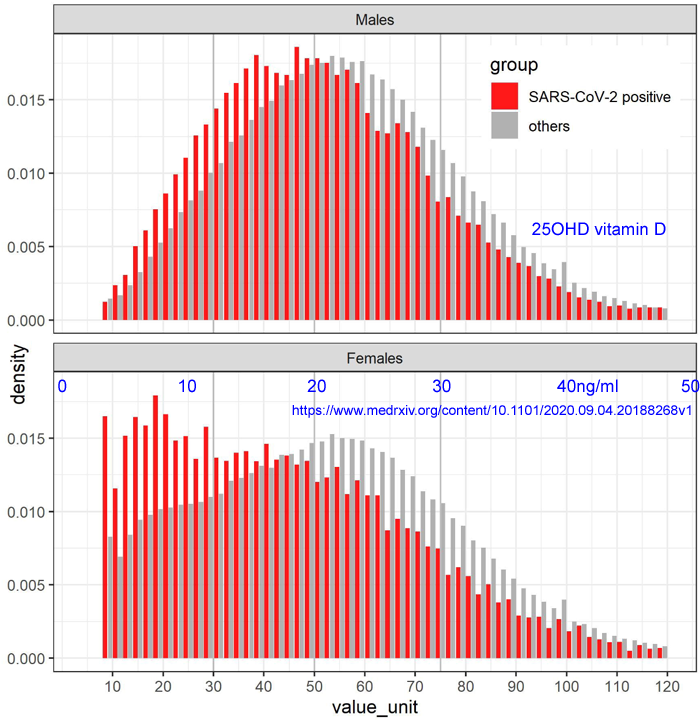
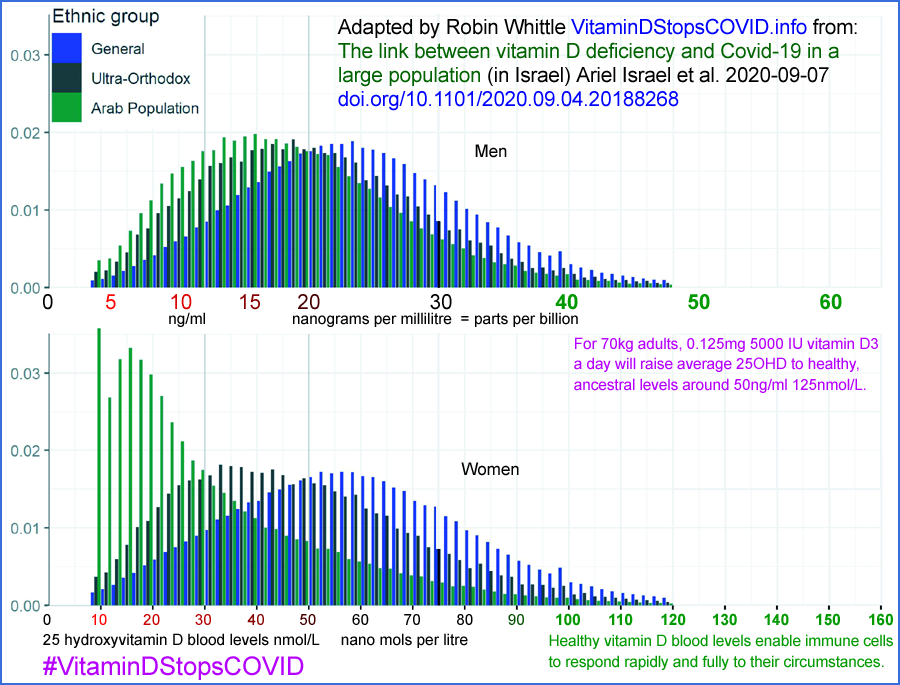
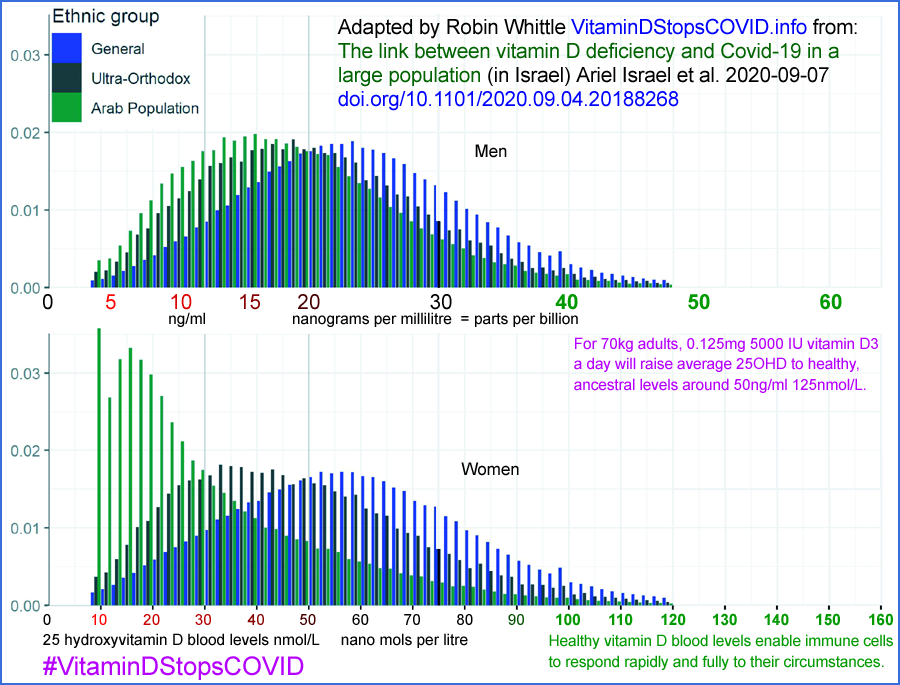
Vitamin D and COVID-19 in 4.6 million Israelis:
From:
here are graphs depicting the distribution of 25OHD levels in
Israel. The top graph is for men and the bottom for
women. The red bars are the proportion of the population
with that narrow range of 25OHD levels who test positive for COVID-19
and the grey bars are for those who do not.
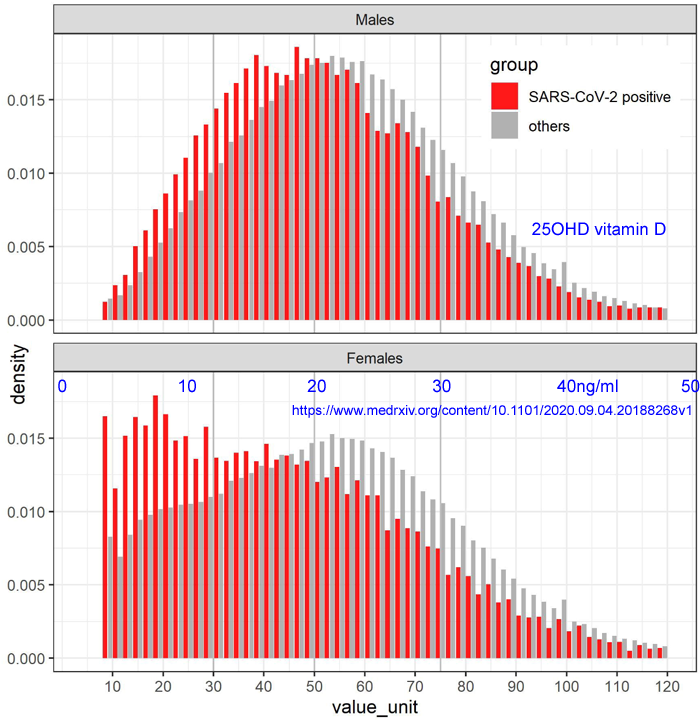
If you see Fig 1 of that article, it is clear that the excessive (compared to men) number
of women with very low (below
15ng/ml) 25OHD levels is due entirely to
Arab women. (Ultra-Orthodox men and women both tend to have lower 25OHD
levels, but there is an extreme peak towards the low end for Arab women
only.) This is clearly due to clothing coverage preventing sunlight from reaching almost all their skin.
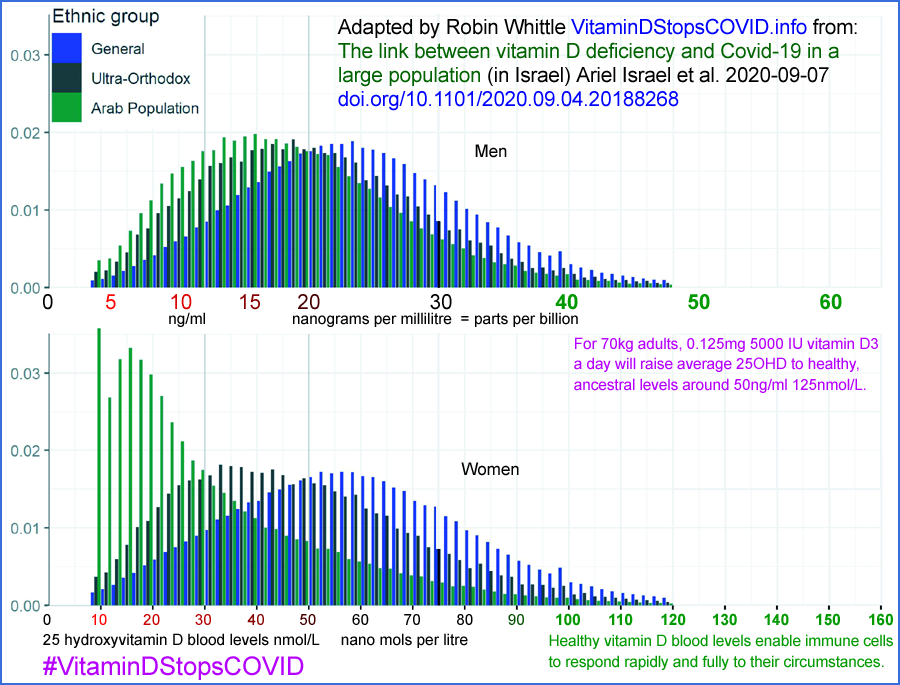
(This indicates, by the way,
that low vitamin D leads to a marginal increase in risk of being
infected for any given viral load. However a complete analysis shows that
the total effect seen in this regard (the peak of red bars being for
lower 25OHD levels than for the grey bars) is also due to these
individuals generally mixing with like individuals with lower vitamin D
levels, and so, it is reasonable to expect, higher rates of viral
shedding than for high 26OHD levels. Also, larger families, less
respect for lockdown, masks etc. may be higher in the Ultra-Orthodox
people and perhaps the Arabs, and both these groups tend to have lower
25OHD and so, I assume, greater rates of shedding and so are more
likely to infect the people they mix with. So I expect the proclivity
of low 25OHD to lead to greater chance of infection for any given viral
insult is likely to be even less than the small effect indicated in these graphs.
Very few of these people have 25OHD levels of
40ng/ml or above.
The average is about half this. For Arab women, the average (Fig 1 in
the above article) the average is even lower. Table 2 shows 59.1% of
Arab women in Israel have average 25OHD less than 30nmol/L, which is
just
12ng/ml. These are
terribly low levels. The best figures are
for ordinary Israeli men: 34% below
20ng/ml, 24% above
30ng/ml and the
rest, 42%, between
20 and
30ng/ml.
See below
#2020-UK-vit-D-BAME for a UK chart showing even lower average levels, and still lower levels coming out of winter.
Despite the tens of thousands of words on this page, the situation looks real simple to an electronic technician like me:
- One human operating requirement is enough vitamin D3 to provide
at least 40ng/ml 25OHD. Without this, hundreds and probably
thousands of types of cell cannot work properly.
- Most people do not get enough D3 to achieve this, even in Israel
which has few people with black or really dark skin, and which is only
about 31° from the equator .
- To a technician, this is much the same as most people on the
planet running around with flat batteries. So for heaven's sake
lets charge them! 45mg of D3 a year, for an average
weight adult, will do the trick. There are other deficient
nutrients as well, but vitamin D is the big one, with such a small,
inexpensive, safe, quantity needed for repletion.
Other pages here
icu/
|
Doctors! Be sure to see
the sections on this page on the Marik Protocol and the closely related MATH+ Protocol
for ICU treatment of COVID-19 patients. It results in higher
survival rates than the techniques used in most hospitals today.
This page also has more detailed discussion of COVID-19 endothelial
pathology in the lungs and the importance of good vitamin D levels to
ensure our immune responses are both strong and well regulated.
|
obesity/
|
Fat cells (adipocytes) in
obesity are known to increase inflammatory responses and so worsen the
cytokine storm which characterises COVID-19 with severe symptoms.
This is true of visceral adipocytes around the heart and other organs
in the abdomen. Ectopic
(growing where they shouldn't) adipocytes in the lungs are also a
problem. Furthermore, adipocytes may express the ACE2 receptor
and so be subject to infection by SARS-CoV-2.
Obesity is perhaps the biggest single risk factor for severe COVID-19
symptoms, and so for death or lasting harm from microembolisms and
resulting organ damage for those who survive. On one hand, it
could be argued that repleting all relevant nutrients to ensure good
immune function - including vitamin D to achieve at least 40ng/ml 25OHD
- will help immune system function in general, but that these excess
adipocyte problems will remain. On the other hand, as far as I
know, the problematic behaviour of these adipocytes is generally only
observed in patients whose vitamin D levels have been low for years,
and remain low. So there's a chance that with nutrient repletion,
their potentially destructive role in the immune response will be
significantly less than is normally the case.
|
d3/
|
Links
to the best research articles on desired vitamin D blood levels and
what amounts of supplemental vitamin D3 are needed to achieve
this, on average, for underweight, normal, overweight and obese body
types.
Links to (and in the future
discussion of) the most pertinent research on the vexed question of
vitamin D toxicity - in general and for individuals with particular
genetic makeups, particular tumors or granulatomous diseases such as
sarcoidosis.
|
| 3-reasons/ |
Three reasons I want everyone in
the world to have good nutrition for immune system health, to greatly
reduce the chances of their immune responses being weak and/or
dysregulated.
|
crisis-diy/
|
(I haven't written this yet.) If demand
for pharmaceutical vitamin D greatly exceeds supply (as I expect it
will once most people recognise they need substantial supplements to
stop their immune system causing harm and death when responding to the
SARS-CoV-2 virus), what are we going to do for people who cannot get
the supplemental D3 they need or good, high-elevation sun exposure most
days? Firstly, access some of the vitamin D3 used for
agricultural feed, which is where about 75% of D3 production
goes. Secondly, use boron - which is worth using anyway for its
anti-inflammatory and other immune-system benefits. Thirdly, find UV
light sources which can drive D3 synthesis in our skin - this is
tricky.
Finally, build vitamin D3 factories in our own countries -
skunkworks-style as in war-time, since our lives depend upon it.
Regarding this, for now please refer to this excellent description of
industrial production of vitamin D3 cholecalciferol by Arnold L. Hirsch in 2010 : https://sci-hub.se/10.1016/B978-0-12-381978-9.10006-X .
|
prisons/
|
About 10 million people
are confined in prisons and jails. They and the
prison staff are at high risk of COVID-19 infection. While (in
the USA, so far, 2020-06-22) rates of prison harm and death per confirmed case from
COVID-19 are
generally lower than in the outside world, this is primarily due to few
prisoners being over the age of 60. The number of confirmed cases
is generally higher - which may be partly due to better testing in
prisons.
The rate of harm and death
for younger prisoners may be higher than in the outside world - in part
because prisoners in general have even lower vitamin D levels than free
living people.
There is an urgent need to give all these people
substantial vitamin D supplements - and more generally the full range
of vitamins, minerals and omega-3 fatty acids. The health and
other benefits have already been shown to far exceed the small cost of
providing these - and COVID-19 infection is close to inevitable
in the months to come.
|
kna/
|
Decreasing sodium (salt)
consumption and boosting potassium intake - including with supplements
in the form of potassium gluconate solution drinks - reduces the
incidence of high blood pressure and stroke.
|
fever/
|
Links to research
articles indicating that in general, with certain exceptions, fever (at
least in the initial stages) should not be lowered because it is an
important part of the body's defense against viral and bacterial
infection. Also links to some research which may indicate there
is little harm and perhaps some benefit of lowering fever with COVID-19
with particular drugs.
|
Contents of this long page
| #intro |
Introduction.
|
| #othersites |
Some other sites of interest.
|
| #cv19vitd |
Recent articles concerning COVID-19 and vitamin D. |
| #2015-Stagi |
Severe vitamin D deficiency in Italian children with Kawasaki disease. |
| #pandend |
Ending the global vitamin D
deficiency pandemic by aiming for at least 40ng/ml 25OHD. This is
the only way we can ensure that COVID-19 causes far less harm and fewer
deaths.
|
| #cvkd |
COVID-19 induced Kawasaki disease in children and babies AKA Paediatric multisystem inflammatory syndrome. |
| #uk-bame |
Discussion of the high rate of
harm and death to black, Asian and minority ethnic people in the UK has
generally not mentioned their very high rates of vitamin D deficiency.
|
| #pep-talk |
Pep-talk for doctors regarding
the need for robust vitamin D supplementation to protect against severe
COVID-19 symptoms. Written specifically for BAME doctors, but
really to all doctors - and not just because of COVID-19.
|
| #2020-Baker-a |
Articles concerning vitamin D
supplementation to protect against harm and death from COVID-19,
including research which shows that 40ng/ml or more 25OHD is required
for proper immune system functioning. Also a list of other
articles of interest I have not read or written about yet.
|
| #low-verylow |
Irish doctors debate whether to use low or ridiculously low doses of vitamin D3. |
| #21authors |
21 authors advise very low levels of D3 supplementation, aiming for a minimum 25OHD level of only 10ng/ml. |
| #weak-sys |
COVID-19 pathology - weak and dysregulated immune systems. The icu/ page has all the details.
|
| #helminthsgone |
Weak and dysregulated, over-inflammatory, immune responses are
caused by lack of helminths, individual genetic variation, dietary
excesses and several common nutritional deficiencies. |
#vaccines
|
A safe, effective, reasonably
long-lasting vaccine to protect against COVID-19 may never be
devised. Even if it is, it will take a long time and be much more
expensive and risky than vitamin D and other nutritional supplements
which will actually, to a substantial degree, solve, the immune system
weakness and dysregulation which drives COVID-19 severe symptoms.
|
| #disclaimer |
I am not a doctor etc. About these pages. Contact and copying information.
|
| #plan |
Global plan for better nutrition
for immune system health, and for better guidance regarding
fever. Written for people who are fusspots for detail.
|
| #msg |
This section is older, and not
so recently updated. It is based on the email I sent out to
doctors, researchers etc. starting on 22 March 2020. This has a section on boron: #08-boron .
|
#intro
Introduction
For an introduction written in late August, please see the 5th comment at:
https://quillette.com/2020/08/27/covid-19-returns-to-new-zealand/ .
In general, people infected with COVID-19 only suffer serious harm, or are killed,
due to their
immune system being weak and/or being dysregulated - their immune response is overly-aggressive, proinflammatory, generally ineffective against the virus and most importantly,
damaging to the self.
The same is true of influenza, but COVID-19 is much worse because it is
highly infectious and - when the dysregulated immune
system allows the virus to infect the lungs - the loss of ACE2
receptors there raises angiotensin II, which causes vasoconstriction of
the pulmonary capillaries and a highly coagulative state, which leads
to micro-embolisms and larger blood clots there and in other parts of
the body. Both the vasoconstriction and the clots reduce the
ability of the lungs to exchange oxygen and carbon dioxide.
Without hospital care, including oxygen (though ideally not mechanical
ventilation, which tends to make things worse), the patient will be
seriously injured or killed through lack of oxygen.
Direct viral and/or dysregulated immune responses damage endothelial
cells in the lung - and presumably elsewhere - and the body responds to
this blood vessel damage by making the blood hypercoagulative.
This hypercoagulative state drives most of the harm which results, with
micro-embolisms and/or larger blood clots anywhere in the body,
including the lungs, brain, spinal cord, heart, kidney and liver.
This can lead to death via stroke, heart attack and kidney failure.
There are evolutionary reasons why our immune systems are dysregulated
- as explained below, we (in developed countries) lack the helminths
(intestinal worms) our ancestors had. Our immune system evolved
to counter helminthic downmodulation of many immune responses.
Without helminths, many of our immune responses are overly-inflammatory
and self destructive.
There is also considerable genetic variation between individuals.
Finally, common nutritional deficiencies and excesses both weaken our
immune system, and reduce its ability to regulate its potentially
excessive actions. The focus of this web page, and others which
lead from it, is to correct these nutritional problems - most
importantly by way of vitamin D3 supplements. If all humans do
this, then our general health will improve in many ways, and COVID-19
will cause us little trouble.
This is the
only way we can deal with the threat of harm and death from COVID-19,
and likewise with the rising incidence of numerous chronic and acute
health problems which result from our generally weakened and
dysregulated immune systems.
We can't stop the spread of the SARS-CoV-2 virus which causes COVID-19
illness. Antivirals have never stopped the spread of any
virus. The common hope or expectation that a vaccine could stop it, by being
proven effective and safe, and administered to most people in the
world, is unlikely in any time frame - and impossible to achieve in
the next few months or year.
It is likely that drugs will be developed which reduce the ability of
the virus to replicate, and so cause serious symptoms. These will
be welcome, but are unlikely to be tested and made available en-masse
any time soon. It makes no sense to be using drugs like this
while it is easier, safer and less expensive to improve our immune
system's strength and ability to regulate itself by correcting
nutritional deficiencies.
We cannot continue to contain the spread of the virus by lockdowns,
social distancing etc. These measures have unsustainable social,
economic and health costs. For now, we should certainly try to
slow its spread - but only when most people's immune systems are
working properly will it be possible to relax these constraints, and so
let the virus spread without causing much harm or death.
Giving humans their proper operating conditions - at least regarding
nutrition for general health and strong, well-regulated immune systems
- is necessary for numerous other reasons (reducing asthma,
neurodegeneration, inflammatory bowel disease, diabetes etc.) and is
urgently needed so we can cope with COVID-19 without the twin disasters
of widespread harm and death (as is occurring now) and of all the
so-far uncounted costs, harm and death which results from lockdowns.
Even children can be affected, with the coronavirus causing their
dysregulated immune system to attack the self in a pattern similar to
that of Kawasaki disease. In pre-COVID research
#2015-Stagi,
it was shown all
children with this disease were severely vitamin D deficient. The
children with the lowest vitamin D levels had the worst outcomes -
their vitamin D levels averaged about 1/10th of the levels of African
herders and hunter gatherers.
So when children are now, tragically, harmed and killed by COVID-19 in ways which resemble Kawasaki disease, it
is reasonable to assume that this is only occurring due to their
extremely low vitamin D levels (no-doubt combined with genetic and
other factors) - and (in the absence of evidence to the contrary) that their parents and treating doctors were
unaware of the need to provide them with adequate vitamin D
supplementation.
There is no reason to believe that there ever
will be
a vaccine which is effective against COVID-19. Immunity to coronaviruses after infection -
or which
might be elicited by a vaccine - may only likely to last a few
years. Vaccines can cause much worse symptoms in some or
many people when the antibodies they raise attach to the virus and are
recognised by receptors other than ACE2, which enables the virus to
infect other types of cells. (Contrary to this gloomy outlook,
see the research mentioned in points 1, 2 and 3 of this
nymag.com article: people who test positive a second time are
not
infectious; SARS-CoV antibodies seem to be effective up to 17 years
later and a SARS-CoV antibody is effective, in vitro, against
SARS-CoV-2.)
SARS-CoV-2 will continue to mutate. We all have to live
indefinitely with current and/or future strains. Fortunately,
this virus does not cause serious trouble for people with properly
functioning immune systems. Other viral diseases do - for
instance smallpox, or ebola. We will be in serious trouble - no
matter how good our nutrition and strong our immune systems - if a novel virus emerges which is as
deadly as these whilst also being highly infectious.
Unfortunately, for various reasons - most of them spurious -
most
(but not all) doctors are excessively wary of nutritional
supplements. This wariness is part of the reason we have such
widespread vitamin D deficiencies. The official vitamin D
guidelines are recognised by many researchers and some doctors as being
woefully inadequate in terms of desired 25OHD levels and regarding
maximum safe dosages of vitamin D3.
This global problem of inadequate nutrition will only be solved by
people choosing to take supplements regularly. Ideally this would
happen as a result of most or all doctors recognising that their
guidance, which lead to the current disastrous situation, was wrong and
that they need to accept and promote the regular use of nutritional
supplements in quantities sufficient to make most people replete -
generally without the need for medical supervision and blood tests,
which are more expensive than the supplements themselves.
For instance, an adult taking 4000IU a day of vitamin D3 needs a gram
every 27 years. The ex-factory, kilogram lot, price of
pharmaceutical D3 is USD$2500. At that rate, the annual cost is
USD$0.09 per year. All that is needed is a capsule or tablet a
week, so 5,200 such capsules, with a total D3 cost of USD$10, and I guess USD$100
manufacturing cost, would be good for one adult for 100 years.
For various reasons - not all of them good -
doctors are extremely resistant to changing their thinking.
In order to avoid a catastrophic continuation of the current harm and
death, they will need to change their minds
fast
- since I can't imagine most people, with the support of their
governments (to handle the logistics of obtaining and distributing the
nutrients), achieving this level of supplementation without the support of most doctors.
Even if COVID-19 disappeared, we still need to give all humans their proper operating conditions as a matter of
urgency, since the same nutritional problems, against a background of
genetic variation, drive the growing burden of chronic and acute
disease, including: diabetes, neurodegeneration (Alzheimer's,
Parkinson's diseases etc.), hypertension, stroke, multiple sclerosis,
inflammatory bowel disease (Crohn's disease and others), sepsis,
osteoporosis and so on.
Here is a chart depicting vitamin D blood levels in relation to body
weight and D3 dosage. The Kawasaki disease figures come from
research before COVID-19 elicited a similar, deadly, condition in some
children, especially in the UK. You can read below
#2016-Caprio research which indicates that
40ng/ml is the minimum 25OHD level for proper immune system functioning. Yet some experts
#21authors advise the public that they should supplement to attain merely
10ng/ml. This is very close to the 9.2ng/ml average 250HD levels of children with Kawasaki disease
#2015-Stagi .
See the
d3/ page where this is part of the guide to vitamin D supplementation. This graph is my adaptation of the original from:
Here is a world map which depicts some estimates of vitamin D
deficiency, where deficiency is defined as 25OHD levels in the blood
below 30ng/ml. However, the best research indicates we
should be aiming for 40 to 60ng/ml. as shown in the chart
above. So by that, realistic, standard, the prevalence of
vitamin D deficiency is much greater than depicted in the following map.
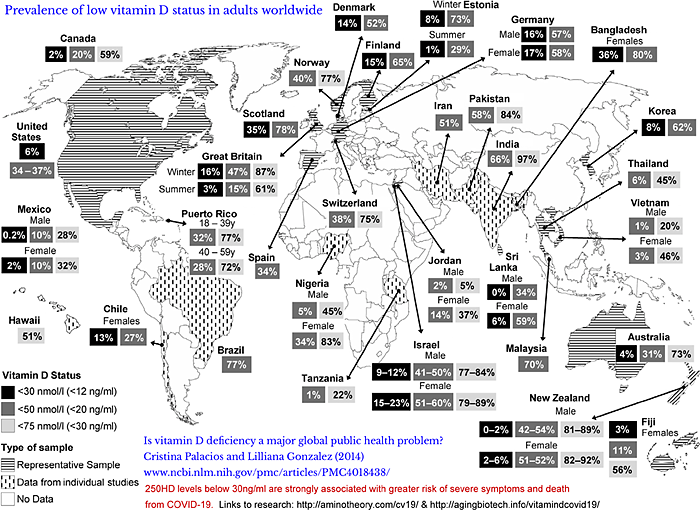
The light grey percentages are for
people with less than 30ng/ml, which is the threshold of vitamin D
sufficiency adopted by the Endocrine Society and some other
organisations. Below you can read research from the Philippines
and Indonesia which indicates that the risk of severe symptoms and
death from COVID-19 is very much greater for people whose levels are
below 30ng/ml than for those with higher levels.
Although these figures are incomplete, and based on research at least 6
years old, it is easy to see what that vitamin D deficiency is a
profound problem in most, if not all countries. Jordanian men are
doing pretty well, but not Jordanian women or any of the other
populations surveyed. Among the most alarming results are women
in Bangladesh (80% below 20ng/ml, the UK with 47% below this in winter,
and 78% of Scots below 20ng/ml - and 35% below 12ng/ml.
So about 1/3 of Scots have about 1/4 of 46mg/ml average vitamin D blood
levels of traditionally living African herders and hunter-gatherers (
https://www.ncbi.nlm.nih.gov/pubmed/22264449). Everyone's immune system evolved to work with these 40 to 60ng/ml
25OHD levels.
The next chart depicts seasonal
variations in vitamin D levels in the UK. See below for another
chart which separates out White and BAME levels.
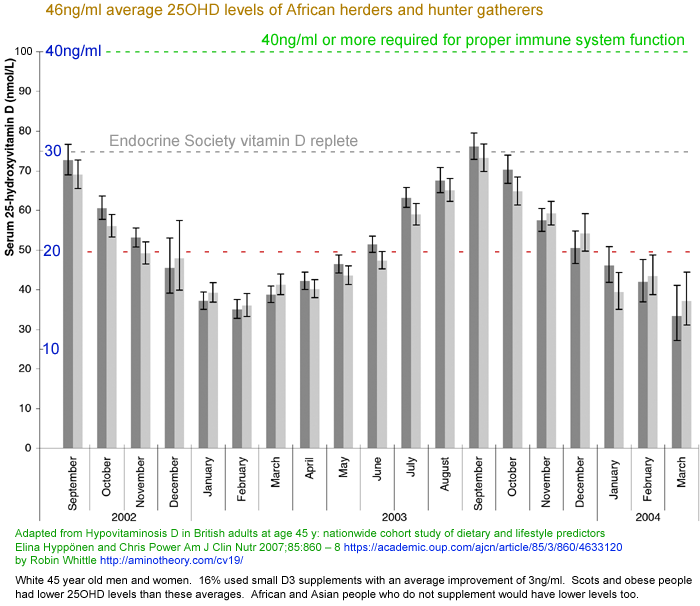
Larger version
1868x1616 . This is from:
The graph shows month-by-month average 25OHD levels in white men and
women in the UK, all aged 45. Most of the time the 25OHD levels
of most people fall under the 30ng/ml threshold below which the
Endocrine Society defines vitamin D insufficiency or deficiency.
16% of these people used modest ~200IU supplements which raised their
levels 3ng/ml on average. This contributes only about 0.16ng/ml to
the average - so the graph is very close to the averages of
non-supplementing individuals. Vitamin D from food made only a
slight contribution to these levels.
Scots and the obese had lower levels than average. African and
Asian people who do not supplement would have significantly lower
levels. None of these averages come close to the 40ng/ml
minimum level required for proper immune system functioning - according
to several research articles cited below, including:
#2016-Caprio &
#2020-Baker-a and to the Scientists' Call to D*Action
link, which was originally made in 2008.
The initial phase of COVID-19 infection, harm and death in the UK
occurred in March to May 2020 - when 25OHD levels were close to their
lowest.
Here is another graph of seasonal
vitamin D levels in the UK, with separate curves for men and women,
white and BAME (black, Asian, minority ethnic) - which means UK
residents with black or brown skin.
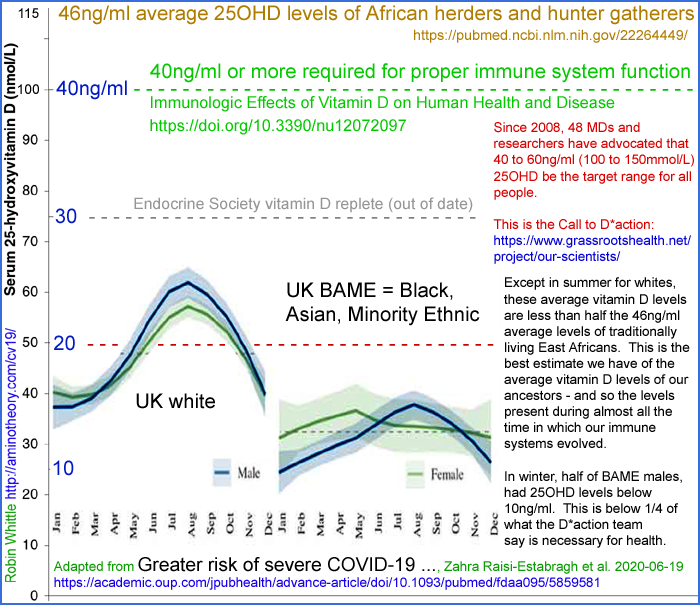
Larger version
1453x1255
. If these graphs don't make you gasp at the tragedy of harm and
death resulting from easily correctable nutritional deficiency, then
you
are not paying attention. This is from:
The data is from 4,510 people, 1,326 of whom were SARS-CoV-2 RNA
positive. Despite the article's title, I found nothing in
it regarding COVID-19 severity. No-one is seriously suggesting
that robust vitamin D supplements will significantly affect the chance
of being infected with the SARS-CoV-2 virus. The lower vitamin D
levels of BAME men compared to women coming out of winter probably
contributes to their higher incidence of severe symptoms and death
compared to BAME women.
There is no numeric mention of the averages for white and BAME people,
but the dotted lines evidently show these: 48 and 32 nmol/L
respectively. Divide by 2.5 to get ng/ml:
- UK white average vitamin D level: 19.2ng/ml = 42% of the presumed average of our African ancestors.
- UK BAME: Black (Caribbean, African, any other Black background),
Asian (Indian, Pakistani, Bangladeshi, any other Asian background),
Chinese, Mixed (White and Black Caribbean, White and Black African,
White and Asian, any other mixed background) and ‘other’. Average vitamin D level: 12.8ng/ml = 28% of the presumed average of our African ancestors.
These BAME figures are averages for multiple ethnic groups. It is
reasonable to assume the Africans, with the darkest skin, have still
lower average 25OHD levels. Now consider UK African males, coming
out of winter, take the 20% of these with the lowest vitamin D levels
and I guess you would find hundreds of thousands of men with 25OHD
levels 6 to 9ng/ml. Now consider all you read below and on the
icu/
page about 40ng/ml being the minimum vitamin D level required for
proper immune system functioning, and how weakened and dysregulated
immune responses (of which low vitamin D is the primary easily
avoidable cause) are the cause of harm and death with COVID-19.
This research also shows alarmingly low vitamin D levels among South Asians in the UK.
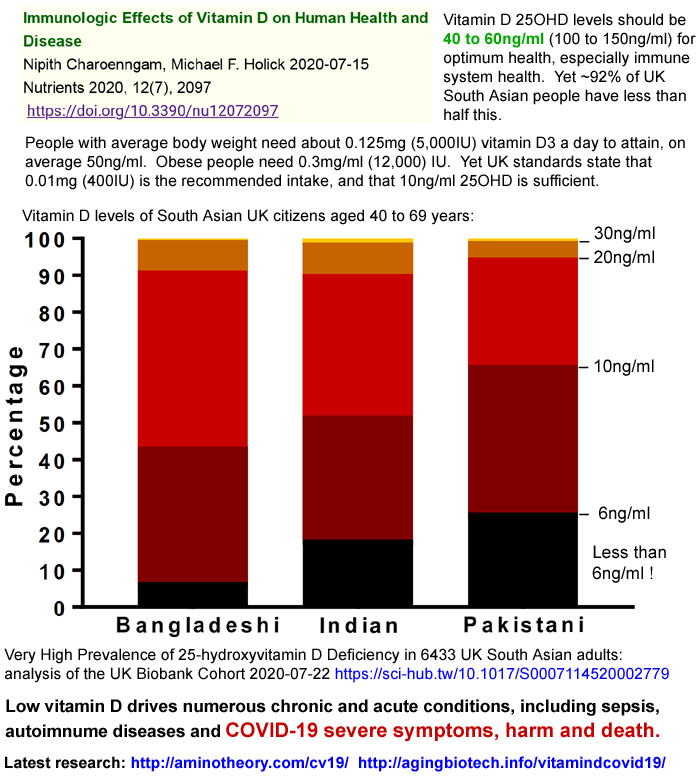
Yet the researchers recommend only 0.01mg (10 micrograms = 400IU)
vitamin D3 a day, in the hope that this will raise 25OHD levels above
25ng/ml - about half of what is recommended for immune system
health. These disastrously low vitamin D levels are
averages. In winter, in men, in the overweight and obese, and in
those living in Scotland, the averages are lower still, and about half
the people have less than the averages.
More on COVID-19 severe symptoms of BAME people in the UK below:
#uk-bame .
Most people the world over are vitamin D deficient. This is
especially so of people who spend most of their time indoors, or
protecting themselves from sunburn (as they should) and all the more so
of people with brown and dark skin who are living far from the equator.
For instance (
BMJ response),
Somalis make up 0.84% of the population of Stockholm County, but but of
the 15 deaths to 2020-03-24, 6 were Somali. This is a death rate
48 times that of non-Somalis.
#othersites
Other sites concerning Vitamin D, the immune system and COVID-19
Karl Pfleger's article Low Vitamin D Worsens COVID-19 Immediate eradication of inadequate vitamin D levels is needed links to and discusses many research articles including some not mentioned here.
https://github.com/GShotwell/vitamin_d_covid
Gordon Shotwell's excellent list of research articles.
An extensive, long-established sites concerning vitamin D and other nutrients:
https://vitamindwiki.com . This is the work of retired electronics engineer and now vitamin D
researcher Henry Lahore. Vitamin D Wiki has
many pages mentioning boron. See also
the pages on the APOE4 allele which is a risk factor for Alzheimer's disease and numerous other conditions [
W]
due in part to it reducing the level of omega 3 fatty acids in the
brain. However, it boosts 25OHD levels, which is generally a
benefit.
(I have been informed by Henry Lahore that the site
www.vitad.org is an unauthorised, illegal, not updated, copy of vitamindwiki.com.)
Some pages at VitaminDWiki:
https://www.grassrootshealth.net
This is a long established vitamin D
advocacy organisation, whose International Scientists Panel includes
many of the most prominent vitamin D research article authors. Since 2008 they have
advocated
(the Call for D*action) for 40 to 60ng/ml 25OHD to be regarded as the optimal vitamin D level -
well above most of the standards which persist to this day.
They offer
test kits for vitamin D, omega-3 fatty acids and other nutrients, since there is 25OHD levels
vary
greatly between individuals using the same supplementation
amount. (Some of that variation will be due to their weight and
whether or not the supplement is taken with a fatty meal. So I
think the graph there, with its extremes from large samples, depicts
more variation than would be expected if a person scales their D3 dose
to their body weight, and takes it with a fatty meal.)
https://www.powerofd.org
Dr Ken Redpath and colleagues do a
great job of promoting robust vitamin D supplementation, especially for
people in the USA with brown or black skin.
The main page and an
interview emphasise the importance of aiming for
40 to 60ng/ml
. However, both these refer to a graph by Lorenz Borsche
purportedly of data from a supposed Indonesian researcher "Dr
Raharusun". The graph depicts no deaths with patients whose 25OHD
(vitamin D blood levels) are 34ng/ml and most of the patients dying if
their levels were below 27ng/ml.
The sharpness of this relationship is completely unrealistic. As you can read
here, the supposed author does not exist. The research never took place. The "data" is completely
fake
and so is the graph. I wrote to Dr Redpath and his
scientific advisors about this on 2020-08-20 and three weeks
have passed without a reply or the misleading information being removed.
Rufus Greenbaum has been advocating
better vitamin D nutrition in the UK since at least 2011.
Sometime in the future - a new website
I plan a more extensive and better organised site
5 Neglected Nutrients,
concerning five nutrients which most people do not get enough of,
causing not just potentially deadly responses to COVID-19, but lifelong
problems with the
immune system, hypertension, stroke, bone and dental health:
- Vitamin D.
- Boron.
- Omega 3 fatty acids.
- Vitamin C.
- Potassium.
Further down this page you will find information on these.
Research in the last few decades shows
that boron has numerous functions regarding proper immune system
regulation and bone health. The mechanisms by which it works in the
body are not well understood and most doctors do not regard it as an
essential nutrient. However, it is inexpensive, safe (below 20mg/day) and in doses such as 6 to 12mg a day helps reduce
arthritis and problems caused by inadequate vitamin D.
Modern diets typically provide only about 1mg boron a day. Like
vitamin D, it improves immune system regulation by reducing the
overly-aggressive, pro-inflammatory response, which drives the cytokine
storm response some people have to COVID-19.
#2020-Davies
Recent articles concerning COVID-19 vitamin D and other nutrients
#2020-Castillo
Spanish Cordoba vitamin D (calcifediol = 25OHD) intervention
trial provides dramatic reduction in COVID-19 severity and deaths
This study from Cordoba, Spain is a highly significant:
Effect
of Calcifediol Treatment and best Available Therapy versus best
Available Therapy on Intensive Care Unit Admission and Mortality Among
Patients Hospitalized for COVID-19: A Pilot Randomized Clinical study
Marta
Entrenas Castillo, Luis Manuel Entrenas Costa, José Manuel Vaquero
Barrios, Juan Francisco Alcalá Díaz, José López Miranda, Roger
Bouillon, José Manuel Quesada Gomez. Journal of Steroid
Biochemistry and Molecular Biology (Prepress accepted 2020-08-24)
https://www.sciencedirect.com/science/article/pii/S0960076020302764
|
This is a randomized, open label,
double masked vitamin D intervention trial involving hospitalised
COVID-19 patients. Instead of supplementing with vitamin D3
cholecalciferol, which must be converted over a few days or so in the
liver to circulating 25OHD (AKA calcifediol & calcidiol), the
patients were supplemented with oral 25OHD which goes straight into
circulation. See my illustrated tutorial on autocrine / paracrine signaling
https://vitamindstopscovid.info/02-autocrine/ for why at least
40ng/ml 25OHD (as measured in vitamin D
blood tests) is required for proper operation of the autocrine (within
the cell) signaling systems of many kinds of immune system cell.
So this is a much faster way of raising people's 25OHD level, without relying on liver function.
See below
#25plusD3 for a
graph which shows how fast and approximately how high this use of 25OHD calcifediol raises blood 25OHD levels
76 patients admitted to hospital with confirmed COVID-19 were randomly split into two groups:
26 patients in the control group received no 25OHD calcifediol.
50 patients in the vitamin D supplementation group received 0.532mg 25OHD calcifideol on day 1, 0.266mg
on days 3 and 7, and then 0.266mg every week until
discharge. (25OHD calcifediol very approximately twice as
effective at raising blood 25OHD levels than D3 for any given mass of
the two compounds. There is no widely accepted conversion ratio
by which to estimate the equivalent D3 amount in IUs.)
All patients received hydroxychloroquine and
azithromycin. Here are the results:
|
Patients
|
Did not need intensive care
Number Percentage
|
ICU
|
Died in ICU
|
Control
|
26
|
13 50%
|
13 50% |
2 8% |
Vitamin D
|
50
|
49 98% |
1 2% |
|
Initial and later 25OHD blood levels were not measured. However the
authors mention that greater than or equal to
40ng/ml is "a guide to the
serum levels of 25OHD3 to be achieved in our trial .". They also
mention that in late winter and early spring, the average 25OHD level of adults in the Cordoba region is
16ng/ml.
Cordoba is 37° from the equator, as is Melbourne Australia, Auckland,
Seoul, San Francisco, Washington DC and Athens. This is a lot
closer than the northern USA, Canada, Ireland, the UK, Germany and
Poland
The randomisation produced a greater proportion of hypertensive and
diabetic patients in the control group, but the authors state that
their analysis shows that the protective effects of the calcifediol
supplementation remained significant. Age, sex and other
comorbidities were in general much the same in the two groups.
The only significant comorbidity not recorded was obesity. The
validity of these very positive results is supported by a separate
analysis by Irwin Jungreis and Manolis Kellis.
If the control group outcomes are extrapolated to the 50 other
patients, we would expect 26 of these 50 to have needed intensive care
if not for the vitamin D supplementation and that 4 of them would have
died. This analysis of the Cordoba trial considers critiques such
as the control group having somewhat more comorbidities, but still
finds the results compelling:
This is the first vitamin D hospital
intervention trial to show such such success in reducing symptom
severity and deaths. Two major features of it are the use of
substantial initial doses (though not as much as the several hundred
thousand IU D3 doses used in other trials mentioned here) AND the use
of
direct-acting 25OHD calcifideol.
The height and immediacy of this oral 25OHD calcifediol treatment had extraordinary benefits for these patients.
COVID-19 patients who need hospital care are in serious trouble.
There's no time to be waiting for their likely distressed liver to
convert D3, so I think it is absolutely valid to use 25OHD instead.
With stark success like this, I think there can be no justification for:
- Further vitamin D hospital trials with a control arm.
We know from this and others trials that higher vitamin D levels are
associated with (and are presumably the cause of) less severe COVID-19
symptoms and fewer deaths AND we have numerous theoretical reasons for
expecting this to be the case.
In this trial 12 or all 13 of the control patients who needed intensive
care probably would not have if they had been given, in total, about
1mg of 25OHD calcifediol in their first week, and just a quarter of that each
week thereafter. Likewise, two people died in this trial
who probably wouldn't have died if they had recieved these
supplements.
The researchers had good reason for believing their intervention would
save lives. I expect they ran the trial with a control arm with
heavy hearts knowing that they would not be giving the best treatment
to some of their patients. They chose to make the control
arm 34% rather than the traditional 50%.
I expect that the researchers conducted this trial for the benefit of
millions of people who will contract COVID-19 in the future - to show
beyond reasonable doubt that robust, especially directly absorbed,
vitamin D supplementation reduces harm and suffering and saves lives in
a hospital setting, so that doctors can proceed with confidence to
treat people this way, rather than calling for further randomized
controlled trials, review papers for such trials, etc. etc, while
patients suffer and die for want of two or so cubic, millimetres of
vitamin D.
(Brenner and Schöttker
also argue there can be no justification for delaying treatment
awaiting further trials, and that 87% of COVID-19 deaths are caused by
vitamin D deficiency.)
- Hospital treatment with ordinary D3 whenever 25OHD calcifediol is
available. Time is precious and the D3 takes a few days to
deliver its benefit.
I believe that the sacrifice made by
the patients in the control arm should be honored by all doctors, in
all countries, by rapidly implementing vitamin D supplementation
programs in hospitals, and more importantly in the general population
to reduce the chances of them needing to go to hospital at all.
In the next few sections - especially
#25plusD3 - I discuss the idea of combining this ~0,5mg 25OHD calcifediol once-off treatment with bolus D3.
#2020-Afshar
Iranian MDs in hospital in Dubai: ratio-based vitamin D
recommendations, bolus doses and 25OHD levels above 40ng/ml resulting
in COVID-19 hospital stays of no more than 3 days, with no need for
intensive care and no deaths
I regard this article as being at least as important as the other
three most important articles in the whole vitamin D, COVID-19 field
- McGregor
et al. (ex-vivo research into hyperinflammatory Th1
lymphocytes because their autocrine signaling systems fail due to
lack of 25OHD), Castillo et
al. (Cordoba 0.532mg 25OHD calcifediol) and Stagi et al. (Kawasaki disease).
This short article is packed with interesting items - I urge
everyone to read it. Highlights include:
- Ratio-based dosing at 70 to 100 IU D3/day per kg bodyweight.
(I derived
base ratios of 72 and 100 IU/day/kg for non-obese and obese
people, respectively, with upper ratios twice this.)
- 500+ neuro-opthamology patients supplemented like this since
2010 all attained at least 40ng/ml (unsupplemented, 95% are
below 35ng/ml) with none over 90ng/ml and no toxicity.
- 21 patients (including 2 healthcare workers and several with
chronic disease) who had > 40ng/ml 25OHD and who had COVID
reported maximum stays in hospital under 4 days.
- In early June they started supplementing all COVID-19
inpatients with 7.5mg 300,000 IU intramuscularly plus
(presumably oral) D3 at 100 IU/day/kg == 0.0025mg/day/kg. For
a 70kg person this is 0.175mg 7000 IU/day. This is in addition
to hydroxychloroquine, Remdesivir and other treatments. This
resulted in:
. . . a dramatic and complete
resolution of ICU admissions was observed in the last 8
weeks.
We cannot over-emphasize the role of Vitamin D in
controlling all infectious diseases especially in COVID-19.
We had no patients with initial Vitamin D levels of
>40ng/ml that required more than 2 to 3 days of
hospitalization, hence no cytokine storm, hypercoagulation,
nor complement deregulation occurred.
Prior to this change, we had several deaths of COVID-19
patients on respirators.
They recommend 70 to 100 IU/day/kg ratio-based D3 supplemental
intake for all people, with a potential simplification for people
between 50kg and 100kg: to a 1.25mg 50,000 IU capsule per week,
which is 0.178mg 7143 IU / day. (143 to 71 IU/day/kg.)
For people with < 30ng/ml 25OHD, they recommend 7.5mg 300,000
IU D3 intramuscular injection, followed by bodyweight ratio-based
daily intakes. For people with 30 to 40ng/ml they recommend just
the ratio-based intakes. For people with >45ng/ml they suggest
retesting after a few days to check for a possibly erroneous
initial reading, and then testing every 4 months after that. Below, by "normal" they mean "healthy".
. . . we would like to propose changing
the VDL to 40 to 100-ng/ml as normal and consider below 40ng/ml as
deficient.
The Journal of Contemporary Medical Sciences (about) was
launched in 2015 and is a quarterly peer-reviewed open access
publication of Nab’a Al-Hayat Foundation for Medical Sciences and
Health Care, Iraq.
I am wary of journals I have never heard from non-Western
countries, but this is legitimate, being listed
in Index Copernicus and not mentioned in this list of predatory
journals: http://olddrji.lbp.world/administrator/RejectedJournals.aspx
. The not for profit hospital is the oldest in Dubai http://www.ihd.ae/about-us
and is primarily staffed by Iranians. https://en.wikipedia.org/wiki/Iranian_Hospital,_Dubai
.
This is the latest in a long line of excellent nutrition research
I have read from Iran and/or Iranians.
#2020-Rastogi
Vitamin D3 bolus AKA loading dosing: 1.5mg (60,000 IU) D3 a day for
7 or more days greatly helps people with asymptomatic or mild COVID-19
overcome the viral infection
Short term, high-dose vitamin D supplementation for COVID-19 disease: a randomised, placebo-controlled, study (SHADE study)
Ashu
Rastogi, Anil Bhansali, Niranjan Khare, Vikas Suri, Narayana
Yaddanapudi, Naresh Sachdeva, G D Puri, Pankaj Malhotra. BMJ
Postgraduate Medical Journal 2020-10-31
http://dx.doi.org/10.1136/postgradmedj-2020-139065
|
People admitted to a hospital in India
with asymptomatic or mild COVID-19, no comorbidities and 25OHD vitamin
D blood levels below
20ng/ml were randomly selected to be in the
control group (24) or the supplementation group (16).
The control group's average 25OHD level was
9.5ng/ml and the supplementation group's were
8.6ng/ml. The supplementation group recieved oral
1.5mg 60,000 IU vitamin D for 7 days (10.5mg 420,000 IU over 7 days) after which 12 of them had attained at least a healthy
50ng/ml 25OHD level and were then switched to 60,000 IU D3 a week. Another two did the same after 14 days.
25OHD rises over days or a week or so as the D3 is converted by enzymes
in the liver to circulating 25OHD. This bolus vitamin D dosing is
safe and better than regular dosing for people who are ill.
In the supplementation group, the inflammatory marker
fibrinogen [
WP]
decreased significantly
(p = 0.007). The liver raises fibrinogen levels to help with
clotting. This increase occurs due to tissue damage in general,
and especially due to
vascular damage
- damage to the blood vessels. It is well known that if the
infection takes hold in the lungs, that the endothelium (the layer of
endothelial cells which
form the inside lining of blood vessels) is severely damaged by some
combination of direct viral activity and the dysregulated,
hyper-inflammatory (cell destroying) immune responses which the viral
infection elicits, at least when there is insufficient 25OHD to
properly supply the autocrine signaling systems of many types of immune
cell. See
icu/#2020-McGregor for how Th1 lymphocytes remain pro-inflammatory rather than switching to an anti-inflammatory program,
due solely to the lack of 25OHD. More on endothelial cells in a moment.
The most important benefit conferred by this robust vitamin D
supplementation - called a loading or a bolus dose, if it is much
higher than usual for a day or for up to a week or so - is that
the vitamin D supplemented patients overcame their viral infection, on average, a lot sooner.
Only
20.8% of the control group had cleared the viral infection with 21 days
of being admitted to hospital. Clearing was determined by two
negative daily PCR tests. Of the supplementation group,
62.5% (10 of 16) cleared the virus by day 21 (p < 0.018).
This 1.5mg (60,000 IU) per day daily intake is
12 times the 0.125mg 5000 IU daily intake which will, after several months, raise the average 25OHD levels of 70kg adults to
50ng/ml. This daily intake is
150 times
the lousy 0.01mg 400 IU D3 intake recommended by the UK
government. It is 15 times the maximum daily intake for
adults recommended by the UK and many other governments, although it is
widely recognised that long term 0.25mg 10,000 IU D3 intake for average
weight adults is still well below the intakes which might lead to
toxicity.
Over a week, these patients received 10.5mg vitamin D3, which is as
much as someone using the scandalously low 0.01mg 400IU UK government recommended
intake would ingest over 2 years and 10 months. It did them a lot
of good and there was no sign of toxicity, which is to be expected,
since intakes like this would need to be continued for a few months
before such problems occurred, with 25OHD levels rising above 150ng/ml.
It is likely that the same or better results would have occurred with
even larger initial D3 doses, which would not have needed to be for so
many days. See
#2016-Han for a
bolus D3 dosing arrangement in which mechanically ventilated
intensive care patients (many with sepsis) received 2.5mg 100,000 IU a
day for 5 days. This is a little more D3, and faster, than the
first week's intake in this Rastogi trial. Those 500,000 IU bolus
treated patients left hospital on average after
18 days, while the control group left after an average of
36 days.
The two known mechanisms by which this bolus D3 dosing would prove effective for COVID-19 are:
- The best known reason is that the reasonably rapid (over a few
days to a week) rise in 25OHD levels - faster and higher than could be
achieved with regular intakes such as 0.125mg 5000 IU a day - result in
a faster and more complete restoration of 25OHD supply to the autocrine
signaling systems (tutorial) of immune cells, and of many other types of
cell.
This improves the ability of the immune cells to respond to their
circumstances, such as by increasing their direct attack on the
pathogens or infected cells, and by improving the ability of regulatory
immune cells, such as Th1 lymphocytes, to damp down destructive
inflammation (cell destruction.)
- A lesser known but surely significant benefit is that the D3
itself, without any conversion in the liver, directly protects the
endothelial cells. This does not rely on the vitamin D receptor
or any changes to the expression of genes. The exact mechanisms are a matter of
ongoing research. This benefit begins within hours as the
D3 goes into circulation. It is not dependent on the D3 being
converted in the liver to circulating 25OHD. This is reported in
the article cited in the next section. See #2015-Gibson below.
This
Rastogi et al. bolus D3 dosing protocol is very successful and should be widely applied
for many COVID-19 patients, including those with mild or no symptoms,
to help them clear the virus, to reduce the chance of serious symptoms
and to reduce their viral shedding and so the chance they will infect
others.
However, please also consider the great success of the Castillo
et al. Cordoba trial
in which hospitalised COVID-19 patients received extraordinary (much
the same as a magic bullet for COVID-19) benefit from an initial oral
dose of just 0.532 mg of 25OHD calcifediol. This is
reported in the previous section
#2020-Castillo.
25plusD3 - my suggestion for a D3 & 25OHD calcifediol
combination supplementation treatment for COVID-19, Kawasaki disease, Multisystem Inflammatory Syndrome, severe influenza
and sepsis
Below, in this section, is a
graph showing
how rapidly oral 25OHD calcifediol raises blood 25OHD levels. See
the following sections for where to get calcifediol - it is now
available in Australia, the USA and Canada, online, without prescription, as 10 microgram
tablets.
2021-05-02: DSM has released d.velop - non-prescription calcifediol,
with online ordering for customers and the USA (before about September
2021, they also allowed delivery to Canada), in packets of
60 tablets, each of 0.01 mg (not 20 micograms, as I previously wrote - this is the serving size of 2 tablets). Each packet, which costs USD$30
including shipping contains 0.6mg of calcifediol - just over the
0.532mg which saved lives and greatly reduced the need for intensive
care in the Cordoba trial (Castillo et al.).
This is excellent news, since
there are millions of people suffering from COVID-19, and at serious
risk of harm and death, whose illness could be reduced within hours and
days by just one milligram or so of this oral calcifediol. No other
compound can do what calcifediol does - raise 25OHD levels robustly in
a few hours. All the details are at: https://vitamindstopscovid.info/04-calcifediol/ .
Here, and in
https://vitamindstopscovid.info/01-supp/#25plusD3 I propose what I call the
25plusD3 protocol 25OHD (calcifediol) and D3 combination therapy
approach, to be implemented without delay for all patients with severe,
or potentially severe COVID-19 symptoms. I think it would also
work better than any treatments I know of for severe influenza and sepsis.
Please note that the following is
written by an electronic technician as a suggestion for what a good
treatment protocol would be.
However, the single dose of 0.014mg calcifediol per kilogram body
weight was developed in consultation with Sunil Wimalawansa MD (retired
professor of medicine, endocrinology and nutrition, at what is now
Rutger's University, New Jersey) who writes about this at
LinkedIn .
25plusD3 is simply the combination of the Han et al. D3 bolus protocol
#2016-Han
or continuing robust (e.g. 5000 IU/day for a 70kg adult) D3 intake, and
approximately double the Castillo et al. 0.566mg 25OHD (on
admission) Cordoba calcifediol protocol
#2020-Castillo.
However,
they
complement each other and I believe that this
25plusD3 double whammy
approach
would be better still than either of them. (The two plus
the rest of the MATH+ would be better still - and I suspect the MATH+
use of corticosteroids could be reduced considerably with these two
vitamin D dosage arrangements combined.)
From 2020-11-12, the highly regarded
MATH+ protocol https://covid19criticalcare.com-
the work of Dr Paul Marik and Colleagues also specifies the use of the
exact same 25OHD calcifediol dosing as used in the Cordoba trial.
This is the initial 0.532mg 25OHD calcifediol and then half this on
days 3, 7, 14, 21 etc.
This is the preferred option for ordinary ward COVID-19 patients
who
need less than 4 litres of oxygen an hour. If the 25OHD
calcifideol is not available, then either daily 0.25mg 10,000 IU D3 or
a small bolus D3 (1.5mg 60,000IU) arrangement is recommended.
However, only calcifediol can raise levels as required in a few
hours. The bolus D3 is too small to achieve this for most people,
and it takes days or a week or to to achieve its peak 25OHD
level. 5000IU/day will take months to raise most people's
25OHD to at least 50ng/ml.
For such patients who need more than this amount of oxygen, or who are
admitted to intensive care, the 2020-11-12 version of the MATH+
protocol recommends a substantial 12mg 480,000 IU D3 bolus. This
will still take a few days to raise circulating 25OHD levels
properly. 1mg calcifediol will do it within a few hours.
The
following graphic is adapted from this version of the
protocol.
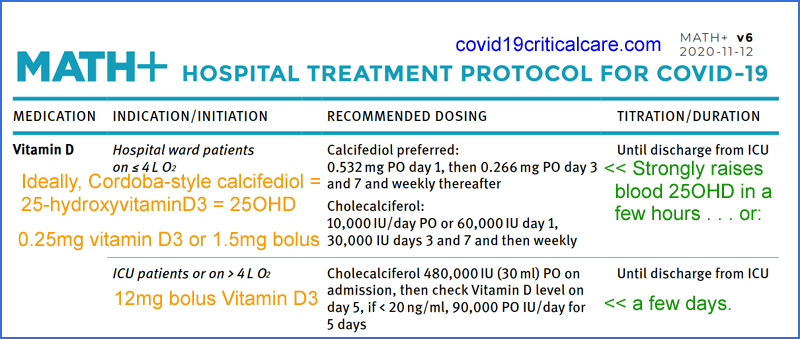
Be sure to check with the
https://covid19criticalcare.com site for the latest version, rather than relying on what I have written about it here at aminotheory.com .
After consulting with Dr Sunil Wimalawansa we agreed that a single
dose of 0.014mg oral calcifediol per kg bodyweight will be highly
effective in all circumstances and carry no risk of toxicity (unless
the person was already near toxic levels due to ingesting completely
excessive amounts of D3 for weeks or months). Please see Dr
Wimalawansa's LinkedIn
post about this and
https://vitamindstopscovid.info/04-calcifediol/#hm .
This is a single, urgent, attempt to replete someones circulating 25OHD
- so we should do a proper job of it.
Sidebar:
If I were a hospital director:
I would make a nuisance of myself
giving both oral 25OHD and bolus D3 (or a set of capsules to take, one
a week or so, for the month or two to follow) to every patient who
entered the
hospital who was had not already substantially supplementing with
D3. I would do the same for their relatives and friends, with the
intention that those relatives and friends wouldn't be turning up to my
hospital as patients for anything like severe COVID-19 or influenza or
sepsis (which is hard to recognise at first, always extremely serious
and likely to be deadly).
Calcifediol alone does not
provide the benefit (the magnitude of which I am not sure about) of D3 protecting endothelial cells [
Gibson et al. 2015]
which line our blood vessels.
The
double-whammy terminology is inspired by the
vitamin D hammer protocol of
Gerry Schwalfenberg MD of Canada. Gerry is an MD with decades of experience, is one of the world's foremost vitamin D researchers and s
ince 2009 has been an
Assistant Clinical
Professor at the Department of Family Medicine University of
Alberta. We are most fortunate that he has joined the NISH list. He teaches and continues his private practice in Alberta, Canada. His article describing this protocol is:
A colleague of mine and I have introduced
vitamin D at doses that have achieved greater than 100 nmol/L
[40ng/ml] in most of our patients for the past number of
years, and we now see very few patients in our clinics with
the flu or influenza like illness. In those patients who do
have influenza, we have treated them with the vitamin D
hammer, as coined by my colleague. This is a 1-time 50 000 IU
dose of vitamin D3 or 10 000 IU 3 times daily for 2 to 3 days.
The results are dramatic, with complete resolution of symptoms
in 48 to 72 hours.
|
For an overview of 155 (2020-11-17) vitamin D bolus dosing arrangements, please see this page
https://vitamindwiki.com/Overview+Loading+of+vitamin+D from Henry Lahore's nearly boundless
VitaminDWiki. (Synonyms for
bolus are
loading and
stoss.)
Here are the three vitamin D3 cholecalciferol bolus dosing arrangements
just mentioned, all known to be beneficial and, within the limits of
the experience and trials concerned, safe. I know of no reason to
believe that any these could lead to toxicity except if someone was
already at extremely high 25OHD levels - in which case they would
probably not be having much trouble with COVID-19, influenza or sepsis.
Name / author
|
Per day
|
Days
|
Total
|
Notes
|
Vitamin D hammer
Schwalfenberg 2015
|
1.25mg
50,000 IU
|
1
|
1.25mg
50,000 IU |
Influenza.
|
Rastogi et al. 2020
#2020-Rastogi
|
1.5mg
60,000 IU
|
7 or more if required to reach 50ng/ml 25OHD.
|
10.5mg
420,000 IU
|
Initially asymptomatic or mild COVID-19.
|
Han et al. 2016
#2016-Han
|
2.5mg
100,000 IU
|
5
|
12.5mg 500,000 IU
|
Sepsis etc. ICU patients on mechanical ventilation.
Half this amount resulted in a 25% reduction in hospital time. This dose resulted in a 50% reduction.
|
The second (the first is below), longer acting, and endothelium protecting part of the
25plusD3 protocol is the Han et al. approach, scaled appropriately by bodyweight for children and adolescents:
2.5mg 100,000 IU oral D3 cholecalciferol per day for 5 days = total 12.5mg 500,000 IU.
This provides immediate (hours) D3 benefits of stabilizing endothelial cells.
It also provides a steady and substantial increase in circulating 25OHD
over the next days and week or two, as the D3 is converted in the liver
to circulating 25OHD.
(Daily D3 supplementation can be continued, but the substantial bolus dose makes this unnecessary for a few weeks.)
Alternatively, for 55 to 85kg adults, a single bolus dose of 5mg 200,000IU D3
will sustain the immediately boosted levels from the 1mg calcifediol
for two weeks or so, after which the patient will ideally be largely
recovered and can return to daily or weekly D3 averaging 5000IU a day
or so.
The first part is immediately active - the same or similar to
the Castillo et al. approach in Cordoba, which was so successful:
A single oral dose of 0.014mg calcifediol per kg body weight at the very earliest opportunity after diagnosis. The the exact dose is not particularly critical. For 55 to 85kg adults, 1mg is fine.
This provides rapid and sustained (for days and weeks, even in
the absence of the D3 bolus) rises in circulating 25OHD, such as above
70ng/ml in a few hours.
The graph below depicts 25OHD levels in
healthy and presumably non-obese subjects, for two Faes
Farma (Spain) Hidroferol calcifediol oil-filled capsules, each of which
contains 0.266mg calcifediol. In Cordoba (Castillo et al.) they
used the same amount with patients, some of whom were suffering from
obesity. So the average dose in Cordoba was probably 0.006
to 0.007mg per kg body weight.
The original version of this graph is from the end of the PDF version of this patent by Faes Farma:
Calcifediol soft capsules
Josep María SUÑÉ NEGRE, Ignacio Ortega Azpitarte, Pepa Del Arenal Barrios, Gonzalo HERNÁNDEZ HERRERO
WIPO WO 2016/124724 Al 2016-08-11
https://patents.google.com/patent/WO2016124724A1/
These Hidroferol capsules are hard to find online, and are prescription medicines. They cost
€20 for 10 capsules.
The manufacturer lists only glass ampoules of this product but the capsules are mentioned
here:
They seem to be available from
pharmacies in Georgia (the country, not the US state). The 43.71 Gel price for ten capsules equates to about USD$14.
5 Hidroferol ampoules, each with oral solution containing 0.266mg
calcifediol are available, with prescription, from this Italian online
pharmacy:
https://www.farmaciatorrent.com/.../238993-vitamina-d-solucion-oral-10-ampollas.html
#neodidro
In May 2021, Dave
https://twitter.com/davinci_mora alerted me to a similar prescription-only product in Italy:
Neodidro 0.266mg
calcifediolo:
http://www.bruno.org/eng/area-osteoporosi.php with a list price of
€10 for 10 capsules. The technical details are:
https://www.torrinomedica.it/schede-farmaci/neodidro/ In English
translation the main ingredients are:
Each capsule contains 0.266 mg of calcifediol (equivalent to 15,960 IU of vitamin D ). Excipients
with known effects: Each capsule contains 4.98 mg of ethanol, 31.302 mg
of sorbitol (E-420) and 0.958 mg of sunset yellow (E-110).
These closely resemble or are the same as details in the Faes Farma patent. Using Google search for
Neodidro
I found several Italian online retailers, but none had any in
stock. These two Greek online sellers report having stock:
https://www.guttafarm.com/neodidro-cena and
https://aspirinca.com/pishchevarenie/neodidro .
The photos at these two sites show orange capsules in similar packaging
to that of Hidroferol, which makes me wonder if these capsules are
identical to Hidroferol capsules.
Bruno also make
Didrogyl prescription-only calcifediol oral solution, listed at the above page, with technical details:
https://www.my-personaltrainer.it/Foglietti-illustrativi/Didrogyl.html In English
translation this is bottle with 10ml solution containing a total of 1.5mg calcifediol.
Other notes about my
suggested 25plusD3 protocol:
As described, the supplementation is given orally, such as in capsules,
tablets or liquid. While 25OHD calcifediol is more easily
absorbed than D3 (due to its extra hydroxyl group making it more polar
and so more water soluble), relying on oral absorptoin in people with
serious illness is problematic. D3 is best absorbed
in the jejunum, when it is geared up for metabolising a fatty
meal. So it would be best to ingest these supplements
towards the end of a meal with at least some fat. It would
probably be a bad idea to take the supplements with a lot of liquids,
which would flush it through the jejunum quickly and limit
absorption.
Patients with Roux-en-Y gastric bypass surgeries have deliberately
reduced fat absorption and so are at risk of vitamin D deficiency and
will probably benefit from twice the quantities mentioned here.
Alternatively the 25OHD calcifediol and/or the D3 could be given
parenterally - by injection or IV drip. This would be necessary
if the patient was being mechanically ventilated, but the whole idea is
to supplement them well before ventilation would otherwise be necessary.
#calcifediol-availability
(Until April, 2021, limited) Availability of 25OHD calcifediol for
human use in the USA, and probably in many other countries as well -
but it is now available, online, without prescription, in Australia and the USA
Please see the above section on the
importance of raising 25OHD blood levels within hours, for all people
who are infected with COVID-19 and whose blood levels are below 50ng/ml
or so, or are reasonably suspected of being this low due to lack of
recent UV-B skin exposure and lack of robust vitamin D3 supplementation
in the last few months. There's no time to run tests and wait for
the results - these people need their 25OHD level raised
now, ideally in minutes, but a few hours will do.
This section concerns the situation before the March 2021 online
availability 25OHD calcifediol in Australia, without need for prescription,
and with the possibility of indirect or later direct shipping to other
countries. Please see the next section for details of this
important new development:
#calcifediol-avail-au .
2021-05-02: DSM has released d.velop - non-prescription calcifediol,
with online ordering for customers in the USA, in packets of
60 tablets, each of 10 micograms. Each packet, which costs USD$30
including shipping contains 0.6mg of calcifediol - just over the
0.532mg which saved lives and greatly reduced the need for intensive
care in the Cordoba trial (Castillo et al.).
This is excellent news, since
there are millions of people suffering from COVID-19, and at serious
risk of harm and death, whose illness could be reduced within hours and
days by just one milligram or so of this oral calcifediol. No other
compound can do what calcifediol does - raise 25OHD levels robustly in
a few hours. All the details are at: https://vitamindstopscovid.info/04-calcifediol/ .
See also a further section below
#calcifediol-lab-agri
on obtaining potentially (likely, in the case of severe COVID-19)
lifesaving calcifediol as lab-grade ~99.9% pure powder or in a diluted
powder form intended for supplementing agricultural animals.
25OHD calcifediol has been used for many years for people with kidney
disease, for regular administration in lower quantiles. So it
should be available in
hospital pharmacies - but read on about this perhaps not being the
case, with one exception: Rayaldee. I don't know
what guidelines or restrictions might govern its use, but you can see
from the Cordoba study that 0.532mg given
as soon as possible
has effects very close to those of a magic bullet for
COVID-19. So I suggest respecting that research and the
needs or the patients rather than whatever guidelines pertain to its
use in other circumstances. If I was treating COVID-19 patients
in the USA, and could not obtain the pharma 25OHD calcifediol needed, I would
be researching lab grade or agricultural feed alternatives.
There is a sustained release 25OHD calcifediol preparation known as
Rayaldee -
https://rayaldee.com.
As far as I know this is the only form of 25OHD calcifediol available
for human use in the USA. (Veterinarians use 25OHD calcifediol as
well, and it is sometimes used as a more easily absorbable alternative
to D3 cholecalciferol in animal feeds, such as for poultry, where it
may be sold as "Hy-D" - see the next section.)
Rayaldee is a patented slow (hours or a day, I guess) release capsule, of only 30ug
calcifediol. This is intended for people with end stage renal
disease, whose kidneys' ability to convert 25OHD into circulating
(hormonal) 1,25OHD for calcium-bone regulation is impaired. I
guess that raising 25OHD levels help by making the limited enzymatic
activity in the kidneys convert more of it to 1,25OHD.
Alternatively, perhaps it helps a little by higher 25OHD levels leading
to healthier supplies for autocrine / paracrine signaling (
https://vitamindstopscovid.info/02-autocrine/)
and that some of that 1,25OHD released for diffusion (paracrine
signaling to nearby cells) winds up in the circulation. The
circulating hormonal levels of 1,25OHD are much lower than those
produced in autocrine signaling - see the above page for links to
research on this.
Since 25OHD has quite a long half-life, typically a week or a few weeks
(though shorter if the levels are higher than ~50ng/ml - see the Ekwaru
et al. graph at:
https://vitamindstopscovid.info/01-supp/a-ratios/), it
is not clear to me why there is a need for extended release daily
capsules, since the extended release presumably goes for hours or a day
or so. Nor is it clear to me (I haven't read the research
on this, but this would be the place to start:
https://pubmed.ncbi.nlm.nih.gov/25446887/
) why these patients can't take substantial D3 supplements and have
their livers convert it to circulating 25OHD. (The quantities are
exceedingly small and are no burden to these large organs, the liver
and kidneys where the conversion enzymes are thinly distributed.)
Extended release is not what is needed in hospitalised COVID-19
hospital patients, since their health and life hangs in the balance and
we want their 25OHD levels boosted to 60ng/ml or more ASAP - ideally in
minutes, but 3 to 4 hours should be fine. I don't know how
slow the Rayaldee release is. Given the choice between extended
release Rayaldee and plain, non-extended release, 25OHD calcifediol
capsules - such the Hidroferol capsules mentioned in the patent above
and which proved so valuable in the Cordoba trial - I think the plain
ones would be better.
However, if extended release 25OHD calcifediol capsules were the only
form available, these would still probably work very well and be a lot
better than vitamin D3, including bolus D3 on its own, due to D3
requiring days to a week or so to be largely converted by the liver to
circulating 25OHD.
In the USA Rayaldee is apparently (I have been told by doctors) the
only form of prescribable calcifediol 25OHD. The capsules
are only 30ug each, and there are 30 in a packet.
20 of those capsules given immediately would be 0.6mg, which is
approximately the 0.532mg quantity in the two Hidroferol capsules given
ASAP in the Cordoba trial. I am just an electronic technician,
but if I was deciding what to take myself, or what loved ones would
take, in the event of suffering from COVID-19 with even a small risk of
it becoming a severe infection (which is always the case, unless one
has been infected for a week or two and seems to be getting entirely
over it), I would give the patient the entire packet of 30
capsules. (This is assuming that the patient probably has 25OHD
well below the desired 50ng/ml more more levels for good immune system
health, due to not taking robust vitamin D supplements in the previous
few months.) This would be 0.9mg 25OHD calcifediol, which is
(very roughly) equivalent (over a period of days or weeks) to three
times this amount of D3: 2.7mg = 108,000 IU = a modest bolus dose of
D3). This would do a proper job of raising the patient's 25OHD
levels within a few hours - and as far as I know, unless the patient
already had
much higher
levels of 25OHD and was at risk of vitamin D toxicity, there would be
zero risk of adverse effects. If the Cordoba results are anything
to go by, the benefits would likely be immense and decisive.
So, in the USA, as far as I know, it is administratively and
technically possible for a doctor to obtain a packet of Rayaldee and
have a COVID-19 patient take most or all of the capsules in a single
day. I assume they can make their own judgments about
dosage - this is all "off label", compassionate use, since Rayaldee is
only approved for use with end-stage kidney disease patients.
However, I know of doctors working in hospitals who, due to hospital
rules, cannot even order 25OHD blood tests for their pregnant
patients. So the idea of a doctor in the USA being a freewheeling
individual whose thoughts and actions are attuned only to preserving
health and preventing death is an ideal which may not be realistic.
There is one potential problem. Rayaldee is extremely
expensive - vastly more expensive than Faes Farma Hidroferol for which
a packet of ten capsules, containing a total of 2.66mg 25OHD
calcifediol, costs (at least in Georgia, the country), about
USD$14. This is about USD$5.23 per lifesaving milligram.
According to
https://www.drugs.com/price-guide/rayaldee a packet of Rayaldee costs
USD$1,206.88 . This is USD$1,340.98 per milligram,
256 times the cost of Hidroferol. I am not suggesting that this is not worth the expense for
COVID-19 patients, since it is likely to be a life-saver, and all it
has to do is get the patient out of ICU a few hours earlier - or not
need intensive care at all - for it to be well worth the expense.
#calcifediol-avail-au
DSM's ampli-D® - 25OHD calcifediol tablets for human use is now available as FORTARO, online, without prescription, in Australia!
Mid May 2021:
FORTARO can now be shipped to any country, with a limited quantity of
three bottles, totaling 3 x 60 tablets of 0.01mg = 1.8mg per overseas
shipment.
2021-05-02: DSM has released d.velop - non-prescription calcifediol,
with online ordering for customers in the USA, in packets of
60 tablets, each of 10 micograms. Each packet, which costs USD$30
including shipping contains 0.6mg of calcifediol - just over the
0.532mg which saved lives and greatly reduced the need for intensive
care in the Cordoba trial (Castillo et al.).
This is excellent news, since
there are millions of people suffering from COVID-19, and at serious
risk of harm and death, whose illness could be reduced within hours and
days by just one milligram or so of this oral calcifediol. No other
compound can do what calcifediol does - raise 25OHD levels robustly in
a few hours. All the details are at: https://vitamindstopscovid.info/04-calcifediol/ .
This update was added in the early
hours of 2021-03-05. To understand the significance of the
matters discussed in this section, you need to be up to speed:
- Broadly understand the importance of good, around 50ng/ml 125nmol/L
blood vitamin D (25OHD) levels to health in general, and the immune
system in general. This whole set of web-pages and my other site https://vitamindstopscovid.info is devoted to helping you acquire this knowledge.
See https://vitamindstopscovid.info/02-autocrine/#04-quraishi
for what I think is an especially precise way of measuring the 25OHD
levels needed for autocrine / paracrine signaling to enable immune
cells in general to work properly.
- Ideally, understand vitamin D autocrine / paracrine signaling, which the immune system depends on: https://vitamindstopscovid.info/02-autocrine/ . Most MDs do not know this, but they all need to. They
tend to think "vitamin D is a hormone", which is not the case regarding
the immune system. This includes, ideally, reading about the
McGregor et al. article which shows how Th1 regulatory lymphocytes fail
to quell the hyper-inflammatory (cell-destroying) immune responses
which cause some people to develop severe COVID-19, when these Th1
lymphocytes do not have sufficient supplies of 25OHD, the form of
vitamin D which is tested in blood tests, and which supplies their
autocrine (inside the cell) and paracrine (to nearby cells) signaling
system: icu/#2020-McGregor .
- Understand the need for
vitamin D supplementation for almost all people (not those who get
sufficient UV-B direct skin exposure all year round - but few do, and
this involves elevated risk of skin cancer). This includes
newborns who are not breast fed or who are breast-fed by mothers who
themselves are not replete. The D3 daily (or equivalent, once a
week or so) supplemental intake levels are ideally a ratio of
bodyweight, with a higher ratio for those who are suffering from
obesity: https://vitamindstopscovid.info/01-supp/ .
- Absolutely required reading:
Read and understand the sections above on the Cordoba 25OHD calcifediol
randomised clinical trial (RCT) involving hospitalised COVID-19
patients: #2020-Castillo , my suggestion
for 25OHD calcifediol 0.5 to 1.0mg dosing for immediately raising 25OHD
blood levels in those people who have low blood levels and are at risk
of developing severe COVID-19: #25plusD3 and the above section on calcifediol 25OHD availability prior to this March 2021 development in Australia: #calcifediol-availability .
Once you have done this you will know that supplementing with 25OHD
calcifediol is of no importance for people who already have good (such
as
50ng/ml 125nmol/L)
vitamin D (25OHD calcifediol) blood levels, which (except for people
with a lot of recent UV-B skin exposure, and ideally unpigmented skin)
means that they must have been robustly supplementing vitamin D3 for
several months.
See also a further section below
#calcifediol-lab-agri
on obtaining potentially (likely, in the case of severe COVID-19)
lifesaving calcifediol as lab-grade ~99.9% pure powder or in a diluted
powder form intended for supplementing agricultural animals.
Some people need higher 25OHD levels, such as to deal with multiple sclerosis and other autoimmune disorders:
https://www.grassrootshealth.net/blog/dr-coimbras-protocol-multiple-sclerosis/
. To quickly attain such higher levels (which should be monitored
in the long term by a Coimbra-protocol-aware MD to ensure there are no
problems) it is reasonable to consider calcifediol 25OHD, as discussed
here and above, as a faster way of attaining such higher 25OHD levels,
despite this involving more than the one tablet a day
recommendation.
Thanks to Robert Andrew Brown of the UK-based McCarrison Society
https://mccarrison.com for alerting me and other vitamin D researchers and advocates to this most welcome development.
Disclaimer:
Please remember that you are reading the best efforts of an electronic technician and computer programmer.
I probably know more about vitamin D than 99.9% of doctors and nurses,
but they know far, far, more about health and medicine than I ever
will. Medical advice is what you get from a qualified medical professional after they have examined you.
The following is for everyone's interest and edification. If you
make your own decisions about health and medical care, read on.
If you don't, read by all means - but please encourage your healthcare
professional to read and research very widely, including this material,
so they can be as up-to-date as possible with the latest research.
Dutch (human and animal) nutritional supplement company
DSM is
selling calcifediol tablets, without any need for a prescription,
via an online site, based at their Australian headquarters in Wagga
Wagga, a major regional city in southern inland New South Wales,
Australia. Deliveries were initially to Australia only, but to
all countries in early May 2021, with an overseas limit of 3 bottles
per order.
 FORTARO
FORTARO provides 0.6mg calcifediol per bottle for USD$20 =
USD$33.33 per milligram.
This is somewhat more expensive than
Hidroferol (mentioned above) which is 2.66mg a box of 10 capsules for about USD$14 =
USD$5.26 per milligram in theory - I do not know where to obtain Hidroferol, and is price was from pharmacies in Georgia, the country, not the US state.
FORTARO is a lot less expensive than
Rayaldee, at
USD$1,340.98 per milligram. FORTARO does not require a prescription in Australia.
2021-03-09: at the end of this section
#2021-03-09
are details of the small tablets themselves, and a link to an article
about neurological harm in children and adolescents suffering from
COVID-19.
There doesn't seem to be a limit on how many can be ordered for delivery to customers in Australia. In March
clicked the quantity up to 500 and the shopping cart software did not
complain.
It is probably possible to order more than three of these bottles for indirect delivery to countries outside Australia via a
mail/parcel/package forwarding company such as:
https://fromaustralia.parcl.com or
https://www.sosmail.com.au/pages/international-shopping/shop-in-australia . Please let me know of any success or otherwise with such companies.
Presumably the same 10ug calcifediol tablets are also sold as a
practitioner-only supplement (sold only to naturopaths and I guess
pharmacies, since medical doctors in Australia do not usually directly
provide supplements or drugs to patients) by Bioclinic Naturals /
Factors Group, as
Opti Active D in bottles of 60 or 120 tablets:
There's no pricing there and it is not available to the public, so the
rest of this section refers specifically to the FORTARO tablets direct
from DSM Australia.
My interest in the easy availability of calcifediol tablets is based on
using it in ways quite different to what they are intended for,
according to the FORTARO product brochure and the TGA approval
document(s) linked to at the end of this section.
The manufacturer (DSM) makes no mention of SARS-CoV-2 / COVID-19, sepsis, Kawasaki Disease (KD, see
#2015-Stagi) of the similarly extreme immune dysregulation disorder Multisystem Inflammatory Syndrome (MIS, see my comments on a
RebelEM article).
The brochure does however cite research on higher vitamin D blood
levels being protective against respiratory infections.
I am interested in how these tablets could be used to treat severe
COVID-19 (or the risk of it developing) and likewise sepsis, KD and
MIS. My interest is solely due to the way calcifediol 25OHD goes
straight into the circulation, without needing the days to week or so
of processing in the liver D3 needs to be transformed into circulating
25OHD. There is also a concern with D3 bolus doses, such as
100,000 IU to 400,000 IU, that this (apparently, I have not researched the details) upregulates 24-hydroxylase enzyme
activity to unusually high levels, which degrades D3, 25OHD
and 1,25OHD.
For longer term protection, as far as I know, D3 supplementation is
perfectly adequate. Calcifediol supplements would work too, but I
know of no long-term advantage, and D3 is less expensive and much more
readily available.
For this use - emergency 25OHD repletion, within hours - the 10
micrograms a day intended dosage of these products would be of almost
no use. I am interested in the use of oral calcifediol in
quantities such as 0.5 to 1mg (500 to 1000 micrograms) or more for obese adults, all at once, or
over a few hours, As Soon As Possible, with these sick people. (I don't
call them patients, since I am not a doctor, and nor would many readers
who want this to protect their loved ones and friends in a crisis,
especially when MDs can't or won't provide
calcifediol.)
These people are either in intensive care, or are at significant
risk of needing it. As I mention above in
#25plusD3,
I think the only need for calcifediol is for this ASAP initial dose,
and that D3 every day or few days thereafter should be fine to maintain
25OHD levels (though D3 on its own is known to protect epithelial
cells).
So my interest is the use of the whole bottle of 60 tablets, over a few
hours or whatever is required, to raise an adult's 25OHD levels as in
the Cordoba RCT. See
#25plusD3 for the graph depicting the rapid rise of 25OHD levels in young, healthy, presumably non-obese, subjects.
Before discussing how I think this product could be used in emergency
(hospital, or risk of hospitalisation) settings with COVID-19, sepsis
etc. I want to discuss how the claims made by DSM et al. for the speed
of action of these 10ug calcifediol tablets are:
- Unrelated to the benefit of D3 not needing to be converted in the liver to circulating 25OHD.
- Arguably inaccurate.
While I am very glad this product is available, and that DSM has
invested in its manufacture, marketing, retail sales business and in
particular getting TGA approval for it, I think their claims about it
being faster than D3 at raising 25OHD levels, on the timescale of
months, which is what they cite, are a poor account of what is
actually happening.
Only about 1/4 of ingested or cutaneously produced vitamin D3 cholecaldiferol is converted into circulating 25-hydroxyvitamin D
#vitD3conversion
It is widely recognised that over time periods of weeks to months,
25OHD calcifediol will contribute to circulating 25OHD levels about the
same amount as 2 to 3 times the same mass of vitamin D3
cholecalciferol. (The article cited below states this.
However, I think the factor is more likely to be 4 or perhaps higher.)
This
shows that only about 1/2 to 1/3 of the D3 molecules we ingest, or
produce in our skin when exposed to UV-B light, are actually converted
to circulating 25OHD. The other 2/3 - as D3 or recently produced
25OHD - must be broken down in some way, most likely by the
24-hydroxylase enzyme.
This well-known efficiency factor, which I assume here is around 3 - fully
explains the earlier attainment of specific 25OHD levels mentioned in
the DSM brochure (linked to at the end of this section), since the
graph in the brochure, here squished and rearranged a little, involves
timescales substantially longer than the 3, 4, 7 or whatever day delay
for converting most D3 into 25OHD.
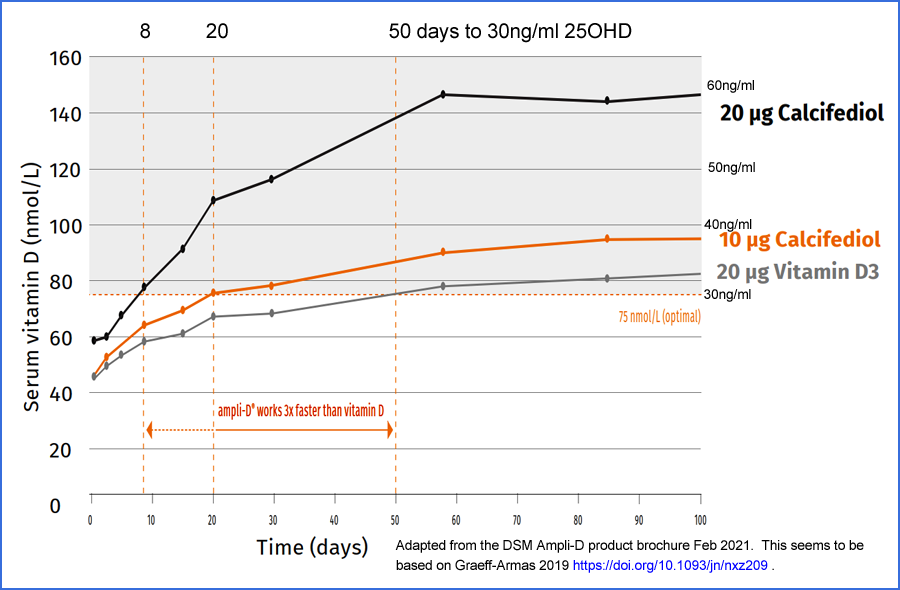
Contrary to the text next to the diagram in the brochure, which refers
to a "Graeff-Armas" article I can't find, this graph seems to be
adapted from this article, which is cited on the last page of the
brochure, with an incorrect 2018 date:
Supplemental
25-Hydroxycholecalciferol Is More Effective than Cholecalciferol in
Raising Serum 25-Hydroxyvitamin D Concentrations in Older Adults
Laura A Graeff-Armas, Igor Bendik, Iris Kunz, Rotraut Schoop, Sarah Hull, and Mareike Beck
Journal of Nutrition 2019-09-13
https://academic.oup.com/jn/article/150/1/73/5569650
|
This brochure graph concerns 20ug/day calcifediol raising levels to
30ng/ml supposedly in about 8 days (the intercept is actually 7 days)
while 20ug D3 supposedly takes about 50 days. This is
twice the amount of calcifediol as the recommended dose of these tablets. The speed ratio, when looking closely at the brochure graph, 6 or 7 to 1, not 3 to 1.
In the article's graph, the baselines are well aligned and the
intercepts to 30ng/ml are about 3 and 46 days, for a circa 15 to 1
speed ratio for 20ug/day calcifediol / D3. However, the text of
the article states that these times are 7 and 40 days respectively,
which I don't understand, and which leads to a 5.7 to 1 speed ratio.
Cholecalciferol certainly does work faster than D3, and in the original
article, the timescales are short enough that the lack of liver
processing is significant.
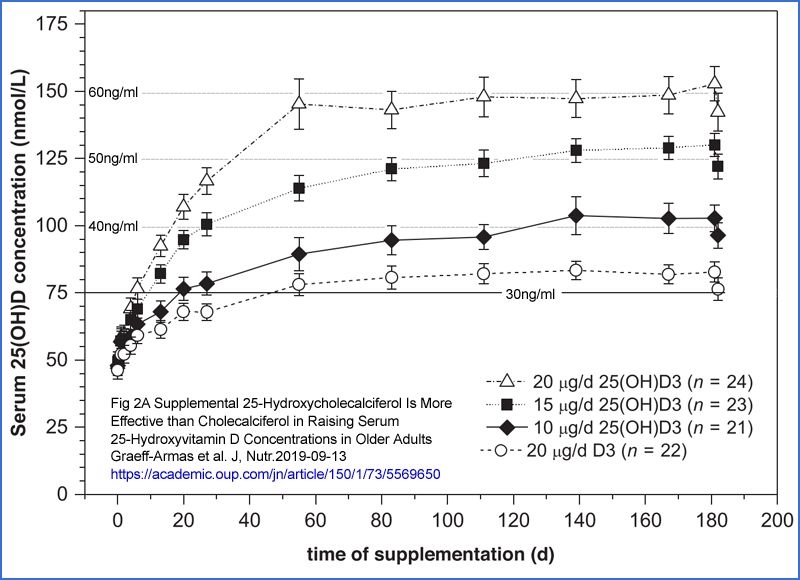
Regarding D3 being processed in the liver, the brochure states "This is
a slow process, thus it can take months to reach optimal vitamin D
levels.". It is more accurate to state that it is an inefficient
process, by a factor of about 3 (below I mention 4 or perhaps more), and that it entails some delay such as
up to a week or so to process most of the D3. As far as I know,
the levels take two months or so to stabilise since there is
considerable storage of 25OHD in adipose tissue - so I guess it would
take longer for obese people. (Also, I am not sure that the
adipose tissue gives all the 25OHD back to the circulation when blood levels drop.)
The article reports that steady state levels were achieved in the same
times for the three calcifediol dosages and for the D3. Both the
lack of liver delay and the greater efficiency explains a shorter time
for calcifediol to raise 25OHD levels above some low threshold, such as
30ng/ml.
#2021-03-07
NOTE 2021-03-07: The following attempt
to calculate the ratio by which calcifediol raises 25OHD levels with
respect to the same mass of D3 is flawed.
I hope to revise it soon.
The assumption below is that we can take, for instance in the graph
above, the 25OHD level rising 3 times as much with 20ug calcifediol per day as with
the same mass of D3 per day and call this a 3:1 ratio. This ignores the
fact that it gets progressively more difficult to raise 25OHD levels due to
the self-limiting activation of 24-hydroxylase enzyme, degrading the
25OHD, and how this is upregulated by at least the 25OHD level itself,
and perhaps the D3 level as well (I don't recall). See the
Ekwaru et al. 2014 graph at:
https://vitamindstopscovid.info/01-supp/a-ratios/
. However, I suspect the way those curves roll off so strongly
towards the horizontal is more extreme than the real situation.
The only way to determine this ratio is to choose a desired target level - such as
50ng/ml -
well above a known baseline, and find how much calcifediol and how much
D3 is required to attain this target level in two similar populations
of people, ideally with the same ingestion arrangements and with the
calcifediol and D3 similarly available as powders, tablets or ideally
with oil. None of these three articles provide such
data. My guess is the real ratio is around 4:1 - but that
is just a guess.
The full article graph supports the hypothesis that 20ug/day 25OHD
calcifediol raises 25OHD levels in the long term about 3 times as much
as 20ug/day vitamin D3 - and this
3:1 ratio is mentioned in the
article's conclusion.
But please remember that this 20ug D3 per day is only 800 IU a day, and
research such as Ekwaru et al. 2014, the graph from which is at:
https://vitamindstopscovid.info/01-supp/a-ratios/
indicates that average weight adults need (on average) 125ug 5000 IU /
day D3 to reach, in the long-term, a healthy 25OHD level of
50ng/ml.
This Graeff-Armas et al. graph shows just 20ug / day calcifediol
achieving this goal after 8 weeks, which is great. I am not
suggesting that calcifediol is any less effective than DMS claim it is,
just that their claims do not fit well with the observations, and that
they fail to distinguish between the 0.5 to 1 week delay inherent in
liver processing and the overall greater efficiency, in the long term
of calcifediol. Also, their description of the 25OHD needing to
be processed in the kidneys to produce 1,25OHD only applies to hormonal
1,25OHD. It is irrelevant to almost all the other functions of
vitamin D, which rely on autocrine and paracrine signaling.
As far as I know, there is no advantage to taking 10ug/day calcifediol
over 125ug 5000 IU / day D3 - both take two months or so to attain, on
average, a healthy
50ng/ml 25OHD level - or probably longer and a lower level in obese adults.
(Update 2021-03-06.)
The Graeff-Armas research reports that 20ug/day calcifediol
attaining long-term ~57ng/ml, from a baseline ~18ng/ml. If this
really does represent the general situation for average weight adults
(I assume ~70kg for Caucasians, with Asians being significantly lighter
[
WP]) then rather than the
3:1 ratio DSM claim in their FORTARO brochure, the real ratio would be in the order of
6:1 to
7:1
in favour of calcifediol. This is based on my analysis of
Ekwaru et al. 2014 where, approximately, and on average, for their
average weight, North American fitness-seeking survey adult subjects,
0.125mg 5000 IU D3 a day raised long-term 25OHD levels to around
50ng/ml.
https://vitamindstopscovid.info/01-supp/a-ratios/ .
Opinions vary on the relative abilities of calcifediol (25OHD) and D3
to raise circulating 25OHD. Here are two pertinent articles, kindly suggested by Owen
Parry. The exact ratio would depend on the formulation of the two
supplements (dry powder, tablet or oil capsule) and the way in which
they were ingested: empty stomach with water vs. start of meal (pushed
through fast) vs. near end of meal with fats (as I aim to do: good fat
absorption and a longer time to be absorbed).
Effects of Cholecalciferol vs Calcifediol on Total and Free 25-Hydroxyvitamin D and Parathyroid Hormone
Albert Shieh, Christina Ma, Rene F. Chun, Sten Witzel, Brandon Rafison,
Hannah T. M. Contreras, Jonas Wittwer-Schegg, Leon Swinkels [DSM],
Tonnie Huijs, Martin Hewison, John S. Adams
The Journal of Clinical Endocrinology & Metabolism, Volume 102, Issue 4, 2017-04-01
https://academic.oup.com/jcem/article/102/4/1133/2982842
20ug calcifediol per day was compared
with 60ug 2400 IU D3 for 16 weeks. Both were DSM powder in
capsules. Baseline average 25OHD levels were 16.2 and 17.0 ng/ml
in the calcifediol and D3 groups respectively. Total 25OHD rose
25.5 vs 13.8 ng/ml, which is a factor of 1.847. Free 25OHD rose
6.6 vs. 3.5 pg/ml, which is a factor of 1.886.
Since the comparison was with 3 times the mass of D3, I calculate an overall 25OHD raising factor of (3 * 1.847) = 5.54:1 in favour of calcifediol.
The graphs show no significant earlier response to calcifediol, which
is not surprising given the low quantities of both supplements and the
first measurement taking place at 28 days, which is much longer than
the 0.5 to 1.0 week time it apparently takes the liver to process most
of the newly circulating D3.
Superior
efficacy of calcifediol soft gelatin capsules vs cholecalciferol
independently of bmi, for the management of vitamin d deficiency in
postmenopausal women: a treatment to be considered in therapeutic
guidelines
Esteban Jódar, José Luis Pérez-Castrillón, Antonio Dueñas-Laita,
Gonzalo Hernández*, Nieves Fernández-Hernando* and Paula
Arranz-Gutiérrez*. * Faes Farma R&D Department.
Endocrine Abstracts, 22nd European Congress of Endocrinology 2020-09-05 (No PDF.)
https://www.endocrine-abstracts.org/ea/0070/ea0070oc2.6
RCT in which one Faes Farma (so, Hidroferol) 0.266mg oil-filled calcifediol capsule per month were compared with 0.625mg D3 per month
(form unknown, but I don't recall any oil filled capsules above 5000 or
perhaps 10,000 IU, so I guess it was powder in capsule. Per
day, this is 8.74ug calcifediol and 20.5ug D3, a 1:2.35 ratio.
I think that vitamin D supplements are best taken daily to weekly or
perhaps every 2 weeks. Every month (4.35 weeks) is surely better
than having none, but a supplemental intake every 7 days or less is surely a better match for the week or
so liver processing and few weeks half-life (less at higher levels,
more at lower) of circulating 25OHD.
41.3% of these postmenopausal women were obese, 32.6% overweight and
25.1% normal weight - with the remaining 1% underweight not included in
the analysis. I don't understand the 4 or 12 month "test regime"
time frames. I assume the results were for 12 months, which
represents steady state and which would also automatically null out
seasonal variations. Baseline 25OHD levels were all below
20ng/ml, so I guess the mean was 13 to 18ng/ml. Here are the
changes in ng/ml 25OHD, with the ratios I calculated to represent
effectiveness of equal masses of calcifediol / D3, considering the 1:2.35 dose ratio:
Morphology Calcifediol D3 Ratio
Normal
16.6
12.6 3.1
Overweight 15.6 9.8 3.7
Obese
13.4
8.9 3.5
I am inclined to think of calcifediol being
3 to 6 times more effective at raising 25OHD levels than D3,
but there will be considerable variation due to the form it is taken
in, whether it is taken with a meal or not, the nature of the meal and
any liquids, whether taken at the start, middle or end of the meal
etc.
(End of 2021-03-06 update.)
This article from 2012 to some extent avoids the abovementioned problem
of assuming that 25OHD levels rise linearly in proportion to supplied
25OHD or D3:
Relative
effectiveness of oral 25-hydroxyvitamin D3 and vitamin D3 in raising
wintertime serum 25-hydroxyvitamin D in older adults
Kevin D Cashman, Kelly M Seamans, Alice J Lucey, Elisabeth Stöcklin, Peter Weber, Mairead Kiely and Tom R Hill.
American Journal of Clinical Nutrition 2012-05-01
https://academic.oup.com/ajcn/article/95/6/1350/4568381
>= 50 year old apparently healthy
adults not in hospital or care homes were given 20ug (800IU) D3, 7ug
calcifediol and 20ug calcifediol. This was in late winter at 51°
N, over a treatment period of 10 weeks. This is not very long,
but is probably long enough to render the ~~1 week liver delay
unimportant.
Both capsules used spray dried
#spray-dry D3 or calcifediol, both manufactured by DSM.
The most interesting comparison is between the 7.7ng/ml increase in
25OHD for the 20ug D3 group (19.9 to 27.6) and the 11.3ng/ml increase
for the 7ug calcifediol group (17.0 to 28.3), though the latter was
from a somewhat lower baseline, and so easier to achieve. The
effectiveness ratio calculated from the masses of the supplements and
the increases is 4.2:1 calcifediol : D3. However, with the
lower baseline, I would adjust this down a little. So my guess is
that for these modest intakes, and modest 25OHD level rises
This makes me more confident of my
4:1 ratio guesstimate of the relative effectiveness of calcifediol and cholecalciferol D3.
Returning to my interest in
calcifediol in emergency settings, with
COVID-19, sepsis, KD and MIS etc. the advantage is that we know from
the Cordoba clinical results and the Faes Farma patent graph mentioned
above, that 0.532mg calcifediol in oil - specifically in the particular
oil and capsule formulation of Faes Farma's Hidroferol gel caps - works
wonders with the 25OHD level, taking it up to
60ng/ml or so in 4 hours or so, at least with the patent trial's healthy and presumably non-obese subjects.
The three calcifediol preparations discussed here are all quite different:
- The Faes Farma Hidroferol capsules have the calcifediol dissolved
in 80% or more by mass oil and 0.3 to 6% by mass solvents. According to
the patent:
- an oily component selected from the group consisting of a medium chain triglyceride, isopropyl myristate, C14-C18 alkyl alcohol, a C14-C18 alkenyl alcohol, lanolin alcohol and mixtures thereof, and
- a
pharmaceutically acceptable organic solvent selected from the group
consisting of ethanol, isopropanol, propylene glycol, polyethylene
glycol, benzyl alcohol and mixtures thereof;
- The capsules used in the Graeff-Armas et al. trial used a "spray
dried" form of calcifediol, dry in a capsule, made by DSM. More
spray drying below.
- FORTARO is a solid tablet. I assume it uses the spray dried powder, pressed together with the various excipients.
We known nothing about how the Hidroferol capsules were ingested in the
patent trial or in the Cordoba trial. In the latter hospital
setting I guess it would have been with water, not with a meal - since
they were keen to treat the patients ASAP. The oil in the capsule
and perhaps the solvents would have helped with absorption of the
calcifediol.
Calcifediol with two hydroxyl groups is apparently more easily absorbed
into the bloodstream than D3, with one, but my experience reading the
absorption literature is confusing.
#spray-dry
As far as I know, from reading about industrial production of both
pharma and feed grade vitamin D, the waxy solid semi-crystalline (at
least for pharma grade, the feed grade is not so well refined) D3 is
dissolved in hot cottonseed oil. I guess it is actually
hydrolyzed cottonseed oil so that its melting point is well above room
temperature. This is sprayed under pressure into cool air
together with a dusting of powders which coat the small solid
particles, which form in mid-air, so they do not stick together.
This is only a few percent, or a fraction of a percent, D3, but the
powder is relatively stable and easy to handle and mix with other
substances. I assume the same process is used for calcifediol.
I would expect the Faes Farma calcifediol to be more readily absorbed
than the dry powder capsule and compacted tablet forms from DSM.
My interest is in how these DSM FORTARO capsules might be used in
emergency (in or pre-hospital, immediate danger for the sick person)
situations. Here are some thoughts about practical matters.
- The Faes Farma 0.266mg capsules are obviously the superior
product. They use oil and are known to work well in the Cordoba
trial and in raising 25OHD levels. Two capsules does the
trick. I am just an electronic technician, but I would
probably use 3 capsules for Justin - Justin Case - unless the person
was 60kg or less. Obese adults need all the help they can
get. I would give 4 capsules for morbidly obese people. (See the #2021-03-09 update for more thoughts on calcifediol dosage by bodyweight.)
Unless they already had very high 25OHD levels, this couldn't do any
harm - and if they had such levels they probably would not be in danger
with COVID-19 and would not have sepsis, KD or MIS.
- However, hardly anyone can obtain these Hidroferol capsules. They
are prescription only, not sold in the USA and are not available in any
reputable site I am aware of. (Please let me know any such sites.)
- FORTARO is easy to get in Australia. See the #2021-03-09 update for details of the tablets themselves. I ordered some in
Case I know anyone who needs urgent 25OHD boosts this Australian
winter, when the new variants of SARS-CoV-2 will surely be causing harm
and death, probably worse than last winter.
Probably most people in most countries could order it if they go
through a package forwarding company in Australia. These
companies may be good at flying things under the Customs radar, so
in practical terms, the US ban on importing prescription items (which
they would be under US law, I assume) may not matter.
Since everyone already has D3, the only reason for wanting calcifediol
is for these COVID-19 emergencies. Even in Australia it can
take a week or more for mail deliveries, so it is no good waiting for
the emergency and ordering some. The sick person needs their
25OHD boosted now - this hour or the next - since their health and life
hangs in the balance.
So any form of calcifediol needs to be pre-ordered so it is ready for
these emergencies. Doctors and nurses can and should do this,
since it can be a lifesaver. No matter where I lived, I
would order some to be ready for emergencies with friends and family,
or neighbours, who haven't been robustly supplementing with D3 for
months.
- To be useful in such emergencies, these FORTARO tablets need to
be taken in large quantities, such as the whole 60 capsules in a
bottle, ASAP (hours or a day) to be useful. If the 60 x 0.01 =
0.600mg intake needed is stretched out over a week, then this is likely
to be little or no better than giving the person two or three 50,000 IU
D3 capsules.
So I would assume at least one 60 tablet bottle per emergency for adults
At a 3:1 effectiveness ratio, the 0.6mg total calcifediol in the bottle
would be roughly equivalent to 1.8mg = 72,000 IU D3. At a
6:1 effectiveness ratio, it would be equivalent to 3.6mg 144,000 IU
D3. Neither of these D3 quantities are particularly big for a
bolus dose, for a 70kg adult. So except for very light adults or
adolescents and children, I would be inclined to think the person would
generally do better with all 60 tablets, or more, as soon as they could safely
be ingested, than with fewer.
Morbidly obese adults' lives are in peril anyway with their extreme
adiposity - and surely low vitamin D levels, unless they have been
supplementing very robustly for a few months at least. They face grave
risks with COVID-19. So I would think two bottles per emergency. (Please
remember you are reading the ramblings of an electronic technician, for
the interest of MDs, nurses and autodidacts such as myself. If
you want medical advice, you need a qualified health professional to
examine you - and hopefully all the material at this site will be of
interest to them, as part of them keeping up with the latest research.)
UK doctors (many of whom seem to think D3 is akin to LSD, strychnine,
ultra-prednisolone or whatever) should probably take some alprazolam
before even thinking about this step beyond the UK government's 4000
IU/day upper limit - but I am an electronic technician and I know of no
reason to fear any adverse outcomes of this 25OHD boost for such
people. See also #2016-Han for 500,000
IU D3 over 5 days halving ICU patients' time in hospital while half
this reduced hospitalisation times by a quarter.
- The tablets are small and should be easy to ingest - see below for details.
- I am not sure to what degree it might be practical to add some
oil, or take them with a meal, to (ideally) enhance absorption. I
assume that the excipients would pose no danger in these quantities,
but that is just an assumption. Can anyone advise? From the
TGA approvals:
calcium hydrogen phosphate \
dihydratecroscarmellose
sodium crospovidone
dl-alpha-tocopherol
magnesium stearate
medium chain triglycerides
microcrystalline cellulose
silicon dioxide
sodium ascorbate
starch
sodium octenyl succinate
sucrose
The world is currently going to hell in a handbasket due to the direct
effects of COVID-19 and the lockdowns, travel, social and business
restrictions - and the likely ongoing nature of these as countries
enforce "vaccine passports" or "immunity passports" and other such
privacy horrors to facilitate limited travel.
COVID-19 would be far less of a problem - probably not requiring most
of these terrible measures - if everyone was vitamin D replete.
They won't be for years, because there is entrenched opposition from
many MDs and administrators, who should know better than to fear this
nutrient. The drug companies would loose countless billions of
dollars if everyone was vitamin D replete. Likewise hospitals.
Calcifediol is not important for long-term repletion, but nothing
else compares with its ability to protect health and lives through
raising 25OHD levels robustly in a few hours.
I was not expecting calcifediol to be available without a prescription
anywhere - but now it is! These tablets are not as convenient,
and may not be as effective, as the excellent Faes Farma capsules, but they are available and affordable.
Some background to DSM's recent human calcifediol initiatives:
DSM's 2021-03-03
ampli-D® press release has a
very long URL
. The statement about 25OHD needing to be processed in the
kidneys to form the 1,25OHD calcitriol, which activates vitamin D
receptors, is only true regarding the circulating (hormonal) 1,25OHD
which regulates calcium-bone metabolism. This very low level of
hormonal 1,25OHD does not affect immune cells, which convert 25OHD to
1,25OHD inside themselves, with vitamin D based autocrine
signaling: https://vitamindstopscovid.info/02-autocrine/#02-nothorm . (What
is the
Get to market faster graphic meant to represent? A salt or sand timer?) A write-up of the press release is at another long URL:
https://www.pharmiweb.com/press-release/2021-03-03/...
DSM's
ampli-D® product page is:
This links (or did in early March - in late March I can't find a link or the brochure itself) to an attractive
ampli-D®
product brochure:
Where others see VITAMIN D we see the opportunity to deliver it FASTER
(PDF creation date 2021-02-12) with images of two cheerful-looking
women and a thoughtful-looking outdoorsy fellow who looks like he would
really appreciate some cheering up. The brochure cites articles
including two written by long time vitamin D researcher and
advocate Bill Grant
http://www.sunarc.org/biography.html and colleagues.
Documents from the Australian Government Health Department's Therapeutic Goods Administration:
https://www.tga.gov.au/book-page/14-calcifediol-monohydrate
2020-05-07 or 2020-06-01 decision to
allow 10ug/day calcifediol. I haven't read it all, but it
contains potentially interesting historical material from various
countries concerning vitamin D regulations.
Three PDFs with very long URLs which are the public summary for ARTG entries for these three products:
All three have the same product description (0.01mg calcifediol
monohydrate plus the same hopefully benign excipients in an uncoated
tablet) and warnings:
Calcifediol
may have similar effects to Vitamin D. Consult your health care
professional before taking in combination with other medicines.
The medicine should not be taken in combination with supplements
containing Vitamin D without medical advice (or words to that effect).
Use in children under 9 years is not recommended.
The Indication Requirements of the DMS products are, with * indicating those which also apply to Opti-Active-D:
Product presentation must not imply or refer to mental illnesses, disorders or conditions.
* If product is indicated for supplementation, Label statement:
[Vitamins/minerals/nutrients/dietary supplements] can only be of
assistance if dietary intake is
inadequate OR [Vitamins/minerals/nutrients/dietary supplements] should not replace a balanced diet (or words to that effect).
Product presentation must not imply or refer to serious immunological diseases.
* Product presentation must not imply or refer to bone disease or
disorders e.g. rheumatoid arthritis, juvenile arthritis, debilitating
osteoarthritis, osteoporosis. Note: this requirement is not
intended to apply where the indications referring to osteoporosis
specified in column 2 of Table 2 of this instrument are also used.
* Label statement: [Vitamins/minerals/nutrients/dietary supplements]
can only be of assistance if dietary intake is inadequate OR
[Vitamins/minerals/nutrients/dietary supplements] should not replace a
balanced diet (or words to that effect).
Product presentation must not imply or refer to serious cardiovascular conditions.
One additional Indication Requirement applies to Opti-Active-D:
Label statement: Advise your doctor of any medicine you take during pregnancy, particularly in your first trimester.
The Permitted Indications for the DSM products are, with bold indicating those which also apply to Opti-Active-D:
Maintain/support general health and wellbeing
Maintain/support healthy teeth
Maintain/support bone health
Aids/assists healthy bone development/growth/building
Help maintain/support bone mineralisation
Maintain/support heart health
Maintain/support immune system health
Maintain/support healthy immune system function
Maintain/support muscle health
Maintain/support muscle function
Maintain/support absorption of dietary (state vitamin/mineral/nutrient)
Maintain/support (state vitamin/mineral/nutrient) levels in the body
Helps prevent dietary (state vitamin/mineral/nutrient) deficiency
Maintain/support neuromuscular function
Maintain/support nervous system health
The additional Permitted Indications for Opti-Active-D are:
Maintain/support bone health in post-menopausal women
Maintain/support bone mass/density/integrity in post-menopausal women
Maintain/support bone mass/density/integrity
Maintain/support bone strength in post-menopausal women
Maintain/support bone strength
Vitamin D helps
calcium absorption (or words of like intent) and a diet deficient in
calcium can lead to osteoporosis in later life
Enhance/improve/promote immune defence/immunity
Maintain/support immune system to fight illness
Enhance/improve/promote/increase (state vitamin/mineral/nutrient) levels in the body
Helps prevent dietary (state vitamin/mineral/nutrient) deficiency
Maintains/support healthy foetal development
Maintain/support healthy pregnancy
2021-03-09 update:
The tablets arrived 5 days after the day of my 2AM order.
They are 0.15 grams, 6.5mm in diameter and 4.5mm top to
bottom. With 10ug calcifediol, these tablets are 0.0000667 =
0.0067% calcifediol. To get 1 milligram of calcifediol, we need
100 tablets, which weigh
15 grams.
Here are 60 of them on 2mm graph paper.
A tablet disintegrated in my mouth after about 15 seconds and had no
taste or smell. In a glass of warm water, each tablet
disintegrates in a few seconds.
I can't imagine anyone having difficulty ingesting 2 a minute, or even
10 a minute. So I expect it would be safe to take a bunch of them
- such as all 60 for a calcifediol quantity of 0.6mg, very similar to
the Cordoba RCT's 0.532mg - in half an hour or less.
However, I think it would be best not to use too much water for this,
so the tablets don't get washed though the intestines too
quickly. The upper part of the small intestine is best for
absorbing oils, and calcifediol is more oily than watery. (People
who have had Roux en Y gastric bypass weight loss surgery have had this
part removed, specifically to reduce fat absorption, so they may need
higher than usual D3 supplements - and so perhaps calcifediol
supplements - to counter this impaired absorption.)
Perhaps the oil-filled Hidroferol capsules used in Cordoba might be
more bioavailable than these tablets. Calcifediol 25OHD is more
readily absorbed into circulation than D3, because it has two hydroxyl
groups rather than D3's one - making D3 less soluble in water and more
in oil.
Maybe taking
these tablets towards the end of a fatty meal would aid
absorption. However, this suggested use is for emergency
treatment of people who are, or may soon become, very ill - so there's
no time for fussing around with theoretically (perhaps) ideal meals.
Everything you read here, apart from direct quotes from other sources, is the ramblings of an electronic technician.
It is intended for MDs, nurses, other health practitioners,
nutritionists and autodidacts such as myself - primarily as a guide to
the latest research. My opinions should carry no weight
whatsoever, but I hope my discussion is of interest and helps with
understanding the research If you make your own decisions about
health - go right ahead, they are your
decisions. If you don't, you should seek medical advice and,
ideally, encourage your healthcare provider to read this material and
other sources as part of keeping up with the latest research.
Please remember that my interest in these tablets is for a totally
different use from what the manufacturer intends: 60 or more - or over
hundred at a time - for morbidly obese people, as a one-off emergency
25OHD vitamin D repletion measure for people at risk of, or already
suffering from, severe COVID-19 & influenza, sepsis, Kawasaki
disease, Multisystem Inflammatory Syndrome or any other acute illness
which is driven primarily by dysregulated, overly-inflammatory immune
responses.
This differs from the use the manufacturers intend the product for, and
what they are allowed to claim it might be useful for. Firstly,
my suggested use is one off, for emergencies - rather than long term
supplementation. Secondly I am contemplating large numbers of
tablets in an hour or so, or less, while this product is intended to be
used one a day for adults.
Assuming the person needing vitamin D repletion has not been
supplementing substantially with D3 for the last month or two, and has
not been getting a lot of unprotected UV exposure (or they have been,
but their skin is brown or black), then it is reasonable to assume
their 25OHD level is between 3 and 20 or maybe 25ng/ml (7 and 50 or
maybe 62nmol/L). We need to get it up to at least 50ng/ml
ASAP. There's no time for tests, and no way of knowing how
responsive they will be. I would aim higher, since there is
no downside in attaining 100ng/ml, and there is a serious downside in
attaining only a level which is not as high as the person really needs.
Children as well as adults can suffer serious harm from COVID-19 and the other conditions just mentioned:
 Kids
Hospitalized With COVID-19 Frequently Have Neuro Symptoms - Most are
transient, but some develop into life-threatening disorders
Kids
Hospitalized With COVID-19 Frequently Have Neuro Symptoms - Most are
transient, but some develop into life-threatening disorders, by Judy George
I would err on the high side to do everything possible with vitamin D
to reduce this dysregulation ASAP. Vitamin C, perhaps IV, and
other measures according to the FLCCC's MATH+ protocol should also be
considered:
https://covid19criticalcare.com/math-hospital-treatment/ .
I guess that 14 micrograms calcifediol per kilogram bodyweight would do
the trick, even for children and adults suffering from obesity.
So that is 1.4 tablets per kilogram, or 0.7 tablets per pound
bodyweight. Probably half this would be fine for most
people, but there's no way of knowing who needs more.
The Cordoba trial was very successful with 532 micrograms. If we
guess the patients body weights were about 70kg (they could easily have
been more) than this was 7.6 micrograms per kg bodyweight. Maybe
their obese adult patients would have done even better with twice or
three times this amount: 110kg is far from the extremes of
obesity (photo #54
here). The Cordoba dose would have been 5 micrograms per kg bodyweight for a 110kg person.
#calcifediol-lab-agri
Alternative sources of calcifediol, including lab grade pure powder
and DSM Hy-D diluted powder intended for agricultural animal feed
Before proceeding here, please read the previous section
#calcifediol-au and all the items of required reading specified there.
This was a long subsection, so I moved it to its own web-page:
#2015-Gibson
Vitamin D3 itself, without conversion to 25OHD, protects endothelial cells, which form the inner lining of blood vessels
This research shows that
vitamin D3 cholecalciferol on its own - previously thought to be
important only as the precursor for 25OHD calcifediol, which itself is
only important because it is the precursor for the 1,25OHD calcitriol
which activates vitamin D receptors - acts on its own, without
involving vitamin D receptors and without altering the transcription of
genes, to protect endothelial cells.
Please see the previous section for how this is clinically important
regarding D3 bolus dosing, and how it is a function presumably not
performed by 25OHD.
I also propose in
https://vitamindstopscovid.info/01-supp/
that this is an argument for not spacing out regular D3 intakes
more than a week, or perhaps two at the most. D3 has a
relatively short half life compared to 25OHD, in part because it is
progressively converted in the liver, over periods of days or a week or
so, into 25OHD.
In order to maintain reasonably high levels of circulating D3, it
follows that D3 intake (or its creation from UVB skin exposure) should
be no less frequent than once a week or so,
#2020-Mardani
Vitamin D 25OHD levels of Iranian patients without COVID-19, with COVID-19 who survived and of those who died due to COVID-19
In March 2020 123 outpatients aged 18
to 78 (median age 42) were referred to hospital with respiratory
symptoms and/or a CT scan showing ground glass opacity in the lungs
(X-ray absorption broadly consistent with pneumonia). 63 patients
these were confirmed by PCR test as suffering from COVID-19 and 4 of
these subsequently died.
Here are the averages of the initial 25OHD levels of these three groups
of patients, bearing in mind that the COVID-19 positive group is all
the 63, including the 4 who died:
|
Not COVID-19
|
COVID-19 positive total
|
COVID-19 positive who died
|
Patients
|
60
|
63
|
4
|
25OHD
ng/ml
|
30.2
|
18.5
|
8.2 |
Fig 1 shows a three bar graph with a different figure for "positive",
being 19.25ng/ml. I think this refers to the average 25OHD levels
of the 59 COVID-19 positive people who survived.
#2020-Jain
Indian hospital observational study of initially asymptomatic patients and those who were admitted, at first, to intensive care
This study is unusual in that the two
groups of patients were chosen to be those at the extreme
ends of the spectrum of severity at admission. Extensive analysis
was performed regarding initial 25OHD levels and the levels of three
substances which indicate the severity of inflammation.
Analysis
of vitamin D level among asymptomatic and critically ill COVID-19
patients and its correlation with inflammatory markers
Anshul Jain, Rachna Chaurasia, Narendra Singh Sengar, Mayank Singh, Sachin Mahor & Sumit Narain
Nature Scientific Reports v10, 20191 2020-11-19
https://doi.org/10.1038/s41598-020-77093-z
|
The 91 patients in Group A were
initially asymptomatic. The 63 patients in Group B were admitted
initially to intensive care - and were more likely to be males and
older than those in Group A.
|
Group A
Asymptomatic
|
Group B
ICU
|
Notes |
Patients
|
91
|
63
|
|
Mean 25OHD ng/ml
|
27.8
|
14.4
|
P = 0.0001.
|
25OHD > 20ng/ml
|
62 (68%)
|
2 (3%)
|
|
25OHD < 20ng/ml
|
29 (32%)
|
62 (97%)
|
|
Highest tertile 25OHD:
27.8 to 49.1ng/ml
|
52 (57%)
|
1 (1.6%)
|
|
Middle tertile 25OHD:
9.2 to 27.7ng/ml |
27 (30%)
|
23 (37%)
|
|
Lowest tertile 25OHD:
3.2 to 9.1ng/ml |
12 (13%)
|
39 (62%)
|
|
In the two groups combined, markers for inflammation were inversely
proportional to vitamin D 25OHD levels. Since 25OHD levels are
relatively stable and little affected by disease progression, it is
reasonable to assume that most of this anti-correlation can be
explained by low 25OHD levels causing the inflammation.
|
Ferritin
ng/ml
|
IL-6
pg/ml
|
Tumor necrosis
factor alpha
pg/ml
|
Highest tertile 25OHD:
27.8 to 49.1ng/ml
|
170
|
10.4
|
10.4
|
Middle tertile 25OHD:
9.2 to 27.7ng/ml |
231
|
17.4
|
12.6
|
Lowest tertile 25OHD:
3.2 to 9.1ng/ml |
384
|
21.2
|
14.3
|
There was a sharp distinction in death rates below and above 20ng/ml
and again, another view of the anticorrelation between levels of
inflammatory markers and 25OHD level.
|
Vitamin D
25OHD levels
below 20ng/ml
(50nmol/L)
|
Vitamin D
25OHD levels
20ng/ml
(50nmol/L)
and above
|
Patients
|
90
|
64
|
Died
|
19 = 21%
|
2 = 3%
|
| Ferritin ng/ml |
19.3
|
12.2
|
| IL-6 pg/ml |
13.6
|
11.9
|
| Tumor necrosis factor alpha pg/ml |
319
|
186
|
#2020-Gennari
Milan study: Vitamin D levels correlate inversely with COVID-19 severity
This
report in
Healio
of a conference paper by Luigi Gennari MD, PhD, associate professor in
the department of medicine, surgery and neurosciences at the University
of Siena, Italy:
Low vitamin D levels independently associated with severe COVID-19 cases, death (
2020-09-11) reports on analysis of 25OHD levels in 155 people:
The
hospitalized COVID-19 group had lower 25OHD levels (mean, 18.2 ng/mL)
than the group with mild symptoms (30.3 ng/mL) or the control group
(25.4 ng/mL; P < .0001 for both).
Compared with COVID-19 cases who survived, those who died had lower 25OHD levels (mean, 13.2 ng/mL vs. 19.3 ng/mL; P = .03).
|
#2020-Panagiotou
Newcastle upon Tyne (UK) COVID-19 patients are vitamin D deficient - and the ICU patients are more deficient
Here is the first substantial report I
know of regarding low vitamin D levels correlating with COVID-19
severity. However, I have
not yet had time to look carefully at this 2020-06-10 Singaporean
article:
https://www.medrxiv.org/content/10.1101/2020.06.01.20112334v2 .
See also the next item
#2020-Merzon for an
Israeli study reporting a similar relationship between low vitamin D
levels and symptom severity, but with greater statistical significance.
Low
serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalised
with COVID-19 are associated with greater disease severity: results of
a local audit of practice.
Grigorios
Panagiotou, Su Ann Tee, Yasir Ihsan, Waseem Athar, Gabriella
Marchitelli, Donna Kelly, Christopher S. Boot, Nadia Stock, Jim
Macfarlane, Adrian R. Martineau, Graham Paul Burns, Richard
Quinton 2020-06-25 (Not peer-reviewed.)
https://www.medrxiv.org/content/10.1101/2020.06.21.20136903v2
|
164 primarily Caucasian hospital inpatients with COVID-19 had their
25OHD levels tested on admission, prior to a selective vitamin D
supplementation trial - more on this below.
92 were in the general wards and 42 in the ICU. (I am not sure
how this assessment was made, since patients can be transferred between
these.) The most directly interesting findings were that the
general ward patients averaged
30.6ng/ml 25OHD while those in the
ICU averaged
24.4ng/ml
. This looks like a significant difference to me, but, probably
due to the wide range of values in each group, analysis revealed that
the p value was only 0.3, meaning that that with the observed scatter
of values, even if there was no actual link between the ward/ICU
observation and the measured levels, that on average, once in every
3.333 trials we would see a deviation like this.
However, some of the other observations point more strongly to a strong
correlation between low vitamin D levels and COVID-19
severity. No-one is seriously suggesting that the low 25OHD
levels result entirely or largely from the severity of COVID-19, so
most of this relationship presumably reflects low vitamin D levels
causing the increased severity. For this not to be the case, some
more complicated hypothesis would need to be accepted, such as an
unmeasured condition causing both the low 25OHD levels and the
severity. This is not out of the question to some degree, but
when we consider how far these 25OHD levels are below the 40 to 60ng/ml
levels recommended as optimal, it is hard to avoid the conclusion that
low vitamin D levels are a major causative factor of COVID-19 severity.
The first observation is that the general ward group was, on average,
older (76.4 years) than the ICU group (61.1). This is highly
statistically significant: p less than or equal to 0.001.
This means that if there really was no relationship, then such a
deviation would be observed on average only once in 1000 or more trails.
Since greater age is generally associated with worse disease outcomes
(the association is causative from age to outcomes, since the outcomes
can't affect age!) the fact that the ICU patients were younger makes us
think that some common factor, such as low vitamin D, might be having a
stronger ill effect with these people, than if the average ages of both
groups were the same.
Moreover, many comorbid conditions (pre-existing conditions generally associated with worse COVID-19 outcomes) were marginally
less
prevalent in the ICU group. The two exceptions were obesity (how
defined?) with ward/ICU percentages 6.3% / 25.7% and hypertension (how
defined) 40.5% / 686.6%, both of which were p <= 0.01, and so highly
significant. However, I am puzzled by the hypertension finding,
since the ICU average blood pressures were lower than the ward average.
C-reactive protein levels were much higher in ICU patients than in the
ward patients. This is expected since this is marker of increased
inflammation.
The researchers defined "normal" 25OHD levels as 20ng/ml or
above. This may be normal in the far north of England, but it is
half the bottom of the 40 to 60ng/ml range recommended by the D*action
MDs and researchers. The ward/ICU percentages of patients with
less than 20ng/ml 25OHD were 61% / 81% (p = 0.02.) This is a very
coarse level of analysis.
Overall, the patients (here the ward and ICU patients are considered all together) had low vitamin D levels:
- 66.4% had less than 20ng/ml.
- 37.3% had less than 10ng/ml.
- 21.6% had less than 6ng/ml. This is described correctly as "very severe deficiency".
Even more horrifying, the researchers mentioned that an unspecified number of patients' 25OHD levels were
below the 3.2ng/ml detection limit! This threshold is 7% of the 46ng/ml average of East African herders and hunter gatherers.
This is a highly preliminary report, as part of a program in which
COVID-19 patients with sufficiently low 25OHD levels recieved
supplemental vitamin D3.
Sidebar: I am just a . . . . If I was a . . . .
I am just an electronic technician, and
I think of low 25OHD levels like a sagging power supply voltage or a
flat battery. I would see patients suffering and dying for lack
of this vital nutrient and I would move fast to fix it. So I
would be supplementing these patients to get their 25OHD levels well
into the 40ng and higher range. I would use oral or perhaps IV
25OHD (calcifideol) itself, since this goes straight into the
bloodstream, while D3 takes days to a week or so to be converted into
25OHD - and that assumes normal liver function, which is unlikely to be
the case.
I would also recommend that everyone on Earth supplement to get their
25OHD levels up to 40ng/ml at least. To me, this is just
like telling my musical instrument customers to use fresh alkaline
batteries, not old ones, or ordinary carbon-zinc batteries. The
cost of these batteries and of vitamin D supplements is vastly lower
than the cost of batteries being flat, or 25OHD being low.
These researchers considered patients with
30ng/ml or more as not needing any vitamin D
supplementation.
- Patients with levels between 16 and 30ng/ml were
given 0.02mg (800IU) D3 orally a day. This is a fraction of the dose most
adults need to attain 40ng/ml or the like, but at least it is something
- and twice the scandalously low 400IU a day the UK government
recommends.
-
Patients with 25OHD levels between 10 and 16ng/ml were given 2.5mg (100,000IU) D3 as a single bolus dose, followed by 0.02mg (800IU) a day.
-
Patients with 25OHD levels between 5.2 and 10ng/ml were given 5mg (200,000IU) D3 as a single bolus dose, followed by 0.02mg (800IU) a day.
-
Patients with 25OHD levels below 5.2ng/ml were given 7.5mg (300,000IU) D3 as a single bolus dose, followed by 0.04mg (1600IU) a day.
No hypercalcemia resulted from any of these bolus doses, which is not surprising.
The authors write that vitamin D levels are so low in the UK in part
due to poor promotion of vitamin D supplements to the public.
They don't mention that this 400IU dose is 10% or less of what most
people need to get to
40ng/ml or so. The note that in
Scandinavia, vitamin D prescription is promoted to the public in
winter, and result in better outcomes.
My overall view of the UK, being hit by COVID-19 as the country came
out of winter, is that almost everyone has dangerously low 25OHD
levels, and that this is in part due to the high latitude and to the
scandalously low standards of dosage and adequate 250HD level
recommended by the UK government. I regard these low levels
as being the biggest single easily avoidable cause of COVID-19
suffering, harm and death in the UK. A similar pattern plays out
in all countries - but the
UK government recommendations are, in my view, just to be very clear,
dangerously and irresponsibly low.
#2020-Merzon
Israeli COVID-19 positive patients who require hospital treatment have lower vitamin D levels than those who don't
Here is a report which passed peer review in late July 2020:
From an initial population of 14,000
people, 7,807 had had their vitamin D (25OHD) levels tested in
February, March or April 2020 - due to some health concern. Of
these, 782 (10.1%) tested COVID-19 positive with a PCR (viral DNA, not
antibody) test. There was a marginal difference in 25OHD levels
between those who tested negative (20.55mg/ml) and those who tested
positive (19.00ng/ml). With the large numbers of subjects, this
was highly significant - P < 0.001, meaning that if there was no
actual relationship, such a difference would only occur once in more
than 1,000 trials.
While it is not particularly surprising that higher vitamin D levels
might reduce rates of infection with SARS-CoV-2, no-one is seriously
suggesting that any level of vitamin D in the blood will provide
reliable protection against infection.
Of much greater interest is the average 25OHD levels of those COVID-19 positive people who were not hospitalised (20.45ng/ml) vs. the levels of those who were (18.38ng/ml).
This is not a particularly dramatic relationship, and it shows that
there is no particular level, at least in these ranges, of vitamin D
which will completely protect against symptoms severe enough to warrant
hospitalisation.
The value of this research is that it involves many more subjects than
the Newcastle upon Tyne research. While the two studies
both relate different levels of symptom severity - the Newcastle one in
hospitalised patients between needing general ward or ICU treatment,
and the Israeli one between not needing hospital treatment and needing
it - we see the same association with low vitamin D and greater symptom
severity.
In the Newcastle research, it could be argued that the COVID-19
symptoms, severe enough to warrant hospitalisation, may have reduced
the vitamin D blood levels (directly, or by causing people to spend
less time in the sun, ingest less food or supplements etc.) by the time
they were tested, upon admission to hospital. The Israeli
research is less subject to such concerns about reverse causality,
because the 25OHD levels were generally, as far as I can tell, taken
before the onset of any symptoms or the COVID-19 PCR tests.
While, due to low numbers of subjects and the (I assume) wide scatter
of the 25OHD levels in both groups, the Newcastle trend was only
significant to p = 0.3, the Israeli research reports a similar trend
with very high significance p < 0.001.
#2020-Maghbooli
Iranian COVID-19 patients' symptom severity, inflammatory biomarkers and death rate correlate with low vitamin D levels
Here a preprint, from ten authors in
Iran with co-author Michael Holick of Boston University - arguably the
best known and most prolific vitamin D researcher.
Vitamin D Sufficiency Reduced Risk for Morbidity and Mortality in COVID-19 Patients
Zhila Maghbooli PhD, Mehdi Ebrahimi MD, Arash Shirvani MD PhD, Mehrad Nasiri, Marzieh Pazoki MD, Samira Kafan MD, Hedieh Moradi Tabriz MD, Azar Hadadi MD, Mahnaz Montazeri MD, Mohammad Ali Sahraian MD, Michael F. Holick PhD MD. Lancet preprint 2020-07-14
https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3616008
|
The PDF date of of this preprint (v1) is 2020-05-28. It reports on clinical observations up to 2020-05-01 (
red, below), from
Sina Hospital, Tehran, towards the end of the first wave of infections in Iran (from
Worldometer) which began at the end of winter. Tehran is at 35.4 degrees north, closer to the equator then most of Europe.
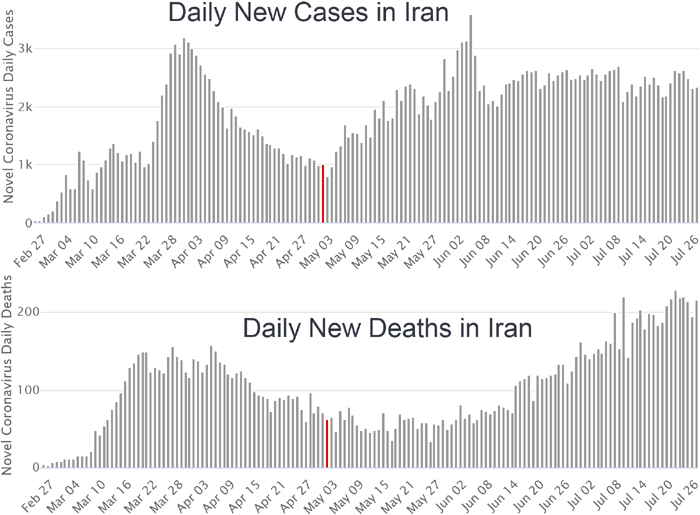
Of the 611 COVID-19 patients at Sina
Hospital, this study concerns 235 who had 25OHD levels tested upon
hospitalisation. There is no mention of vitamin D or any other
nutritional
supplementation in hospital. All patients were 18 years or older
with
mean age 58.7. 37.4 were over were 65+. No patients
40 years or
younger died.
30ng/ml was defined as vitamin D sufficient, according to Endocrine
Society and other standards - not the UK standard which is 10ng/ml
(which vitamin D researchers and clinicians have been protesting for
years).
However, the observations show that for COVID-19 sufferers, 30ng is not
sufficient, replete or whatever - since, as best I understand the
analysis, bad outcomes were inversely proportional to vitamin D levels
for most or all of the cohort of patients, not just those with 25OHD
levels below 30ng/ml.
Sidebar on Iranian research:
I read a lot of research from all over the world, and I frequently encounter excellent research from Iran, Turkey, Iraq and (in at least one case) Kurdistan regarding nutrition, especially regarding vitamin D and boron.
I wonder why, in the midst of a
disastrous wave of COVID-19, and operating under numerous other
difficulties, these Iranian clinicians were able to measure the 25OHD
levels of 38% of their COVID-19 hospital patients AND conduct a
detailed study, in April, when months later, in the whole rest of the
world - with Western hospitals operating under far fewer difficulties -
is very rare to find any research study of all those concerning with
COVID-19 that even mentions vitamin D.
In the West, most doctors would
look at you blankly at the mention of boron as a nutrient. Even
the vitamin D researchers rarely mention it.
My working hypothesis is that
whatever the cause of the unknowing, unreasonable, lack of interest
regarding nutrition which seems to be a hallmark of much of Western
medicine, many clinicians and researchers in these countries have done
well to avoid this stifling trend.
Some key points, with my paraphrasing:
- Low vitamin D correlated significantly (p = 0.04 to 0.004) with
mortality, symptom severity, unconsciousness, hypoxia, C-reactive
protein [W] (a marker of inflammation) and low levels of lymphocytes.
- 77.2% of patients with less than 30ng/ml 25OHD had severe
symptoms, and for the others, with 30ng/ml or greater the figure was
63.6%.
This shows there is a
downwards slope in symptom severity with increasing 25OHD levels, but
no magic safety zone above any particular value which protects people from severe symptoms,
as is depicted in the widely circulated, and still cited, Raharusun
article (withdrawn in late June 2020, which I now believe is fictional:
#2020-Raharusun) and from which the
steep slope graph you can see here:
https://borsche.de/res/Patterns_of_COVID_19_Mortality_and_Vitamin_D_An_Indonesian_Study.pdf
was supposedly derived from. This steep slope graph, which I used
to have on this page, is also widely cited, at least on Twitter, blog
posts and the like.
Ideally we would have age and 25OHD data for the population from which
the patients came, with such data for those who were known to be infected. Then we
would be able to estimate, for different age groups, to what extent
high vitamin D levels were protective against being hospitalised,
having severe symptoms or dying, rather than having few enough symptoms
not to need to go to hospital. However, we don't have this data.
From the article, here are some of the most significant differences in
outcome between the 158 patients with less than 30ng/ml 25OHD and the
77 patients with 30ng/ml or more.
Clinical outcomes
|
< 30ng/ml
N = 158
|
>= 30ng/ml
N = 77
|
P value
|
Deaths
|
20.0% (26)
|
9.0% (7)
|
0.04
|
Unconsciousness
|
8.3% (13)
|
1.3% (1)
|
0.03
|
Hypoxia
|
39.2% (62)
|
19.4% (15)
|
0.004
|
CFP > 40ng/L
|
77·2% (122)
|
61.0% (47)
|
0.01
|
Lymphocytes < 20%
|
60·1% (95)
|
45·5% (35) |
0.03
|
Severe - critical
|
77·2% (122)
|
63·6% (49)
|
0.02
|
In late July 2020, as I write this, we might have reasonably expected
clinicians and researchers, starting in China, to have been measuring
vitamin D levels and their correlation with symptoms since January of
February, with a rich set of studies being published by March or
April. Yet, here we are, with only a handful of studies - and all
of them which we can easily imagine being more detailed.
In this context, I take some interest in the following diagram.
It depicts all patients in this Iranian study, denoting those who
died. (I compacted the legends a little and moved the
horizontal line at the bottom to the 0ng/nl position.)
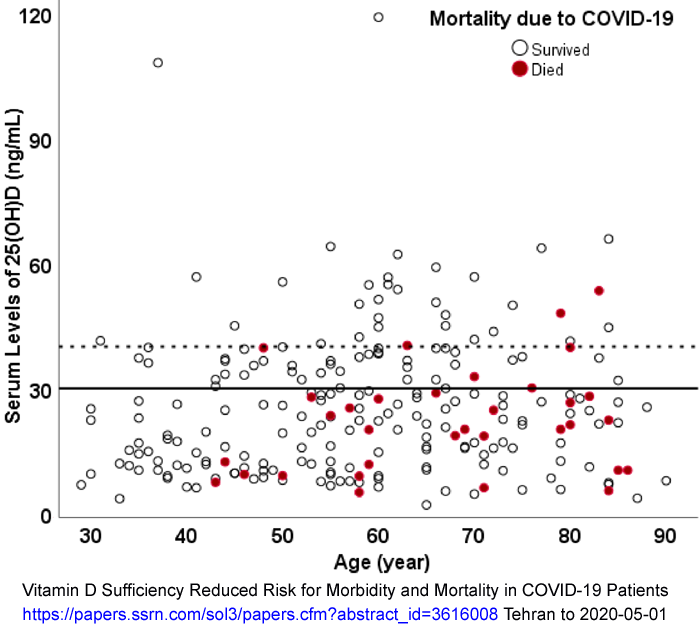
It is notable that quite a few people
with 40ng/ml or more 25OHD needed to go to hospital. The five
people who died with the highest vitamin D levels included one with
about 54ng/ml, one with about 48ng/ml and three with about 40ng/ml.
Ignoring the two outliers with over 100ng/ml, there is a general trend
towards people being hospitalised and dying with higher vitamin D
levels according to their greater age.
Assuming that people under 50 also have a wide range of 25OHD levels,
and that these people suffered similar rates of COVID-19 infection, we
can see that:
- Younger people (anyone under 50 or 60 is young with COVID-19) were less likely to need hospital treatment.
- The subset of the younger people who did need hospital treatment
had lower 25OHD levels than those who were older. So it can
be inferred that higher vitamin D levels were protective for people in
their 30s to 50s too.
- These Tehran hospital patients seem to have a higher range of
25OHD levels than can be seen in charts on this page for other
populations, such as non-supplementing white women in the USA (below),
or all people in the UK (above).
In these patients, there is no hard level above which 25OHD levels
offer complete or very high levels of protection against needing
hospital care, or of dying, from COVID-19, at least for people aged 40
years or more.
Assuming that the vitamin D level - severity/death correlations for
these Iranians can be extrapolated to other populations, including
those where vitamin D levels are generally (without supplementation)
generally lower but where quite a few people have levels above 40 or 50
due to robust supplementation (I assume most people stay out of the
sun) then I propose that in this data we see evidence of a relationship
with both COVID severity and mortality which slopes downward over a
range of vitamin D levels, from 0 to 60ng/ml at least.
Contemplating a COVID-19 suffering, harm and death hazard curve according to vitamin D levels
Assuming for the moment that this is
the case, I would depict this curve, or line, representing severity
(and so the level of suffering and lasting harm) and of the risk of
death, vs 25OHD levels, as sloping downwards from top left to bottom
right, in the range of interest, at least to 60ng/ml, and probably
somewhat beyond.
Here is an all-cause mortality graph from a recent UK BIOBANK research article. It has nothing to do with COVID-19.
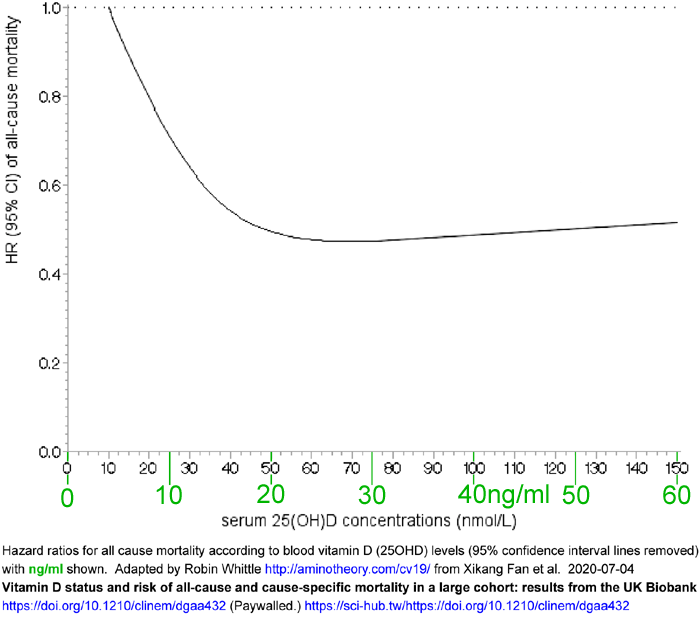
This results from an average 8.9 year follow-up time for 365,530 UK
adults who reported no cardiovascular disease (CVD), cancer or diabetes
at baseline, 2006 - 2010.
The 1.0 starting point is the all cause mortality risk for the 10% of
the cohort with the lowest 25OHD levels ("lowest decile 10.0 to
22.7nmol/L) - a range of 4 to 9ng/ml. 46ng/ml (115nmol/L)
is the average level for traditionally living Maasai herders and
Hadzabe hunter gatherers.
See the chart above
#2020-UK-vit-D-BAME
(also derived from BIOBANK data) showing that, depending on season, sex
and white / BAME, people in the UK mainly had 25OHD levels in the ~7 to
~27ng/ml range.
The rise in the risk of death shown above about 30ng/ml is primarily
due to the risk of cancer and could be due to people who were ill at
baseline taking vitamin D supplements, and later dying due to their
pre-existing illness. (The survey asked about vitamin D
supplementation, but not the dose, and did not include anyone with a
cancer diagnosis at baseline.) See pages 16 and 17 of the article
for their discussion of this small rise in risk beyond 30ng/ml not
being reported in all other comparable studies, and not necessarily
reflecting actual risks.
As noted above, vitamin D specialists recommend 25OHD levels of 40 to 60ng/ml for proper health.
There's a difference between what we all aim for - robust good health
in numerous respects, as close as possible to what our bodies are
capable of with good nutrition and care - and death, which is the
failure to have any health at all.
Consider neurodegeneration - Alzheimers disease, Parkinson's disease,
dementia with Lewy bodies etc. They are all much the same, with
minor differences in detail. Excessive inflammation (which would be reduced by adequate vitamin
D, omega 3 fatty acids
* and I think
boron) drives protein agglomeration and further immune
responses which damage and kill neurons, subtly at first, and then
vastly, degrading quality of life - and
eventually extinguishing it.
* VitaminDWiki has thousands of
pages on this topic.
This and many other degradations of quality of life don't show up as
death until we have been suffering them for decades. So all-cause
mortality is some kind of guide as to what we want to avoid, but our
goals are to thrive, not just survive.
Consider this curve, and for now assume it is flat beyond 30ng/ml.
If you know for a fact that your 25OHD level is consistently 30ng/ml,
it would be tempting to keep it there, since it looks like it would
need to go as low as 15ng/ml before there was a noticeable increase in
risk of death. Some people who recovered from cancer or MS with
much higher levels of vitamin D would tell you their experience is
different - but lets assume you will never be in their position (though
you may be). In terms of
CVD, cancer and all other causes experienced by these BIOBANK people, it looks like there's no health advantage to raising your 25OHD levels beyond 30ng/ml.
But this is mid-to-late 2020 and it is reasonable to assume that most
of us are going to get COVID-19 in the months or year or so to
come. There are several conditions other than COVID-19
which test of our immune system's initial strength and its proper
regulation - which fails spectacularly in sepsis, ARDS, influenza-driven
pneumonia etc.
Most people think - not always correctly - that these things won't happen to them.
COVID-19 is a much more rigorous test of our immune systems than
influenza - and it is spreading rapidly, with most of us having
no immunity, and no chance of protection via vaccines, antivirals
(except perhaps if we can get into hospital, which is not assured) etc.
Now, back to the Iranian data. The following are my thoughts, and
I have no medical training - so consider everything carefully and don't
take my word for anything.
It seems that the Iranian cohort had a
much wider range of vitamin D levels than the UK BIOBANK data.
Most of the UK people, as far as I know, have vitamin D levels
below 30ng/ml. They are living 50 to 58 degrees north, which is
totally different from the Iranian experience at 36 degrees.
Yet there are quite a few Iranians - at least those older than 40 - in
hospital due to COVID-19. (Iran health is probably suffering
since the country is subject to trade sanctions and faces other
difficulties.)
IF we assume that the Iranian data is broadly applicable to all people
- at least those older than 40 (and still with some relevance to
a smaller proportion of younger people and children, according to
genetic and other factors), AND since we know that in the Iranian
cohort, the inverse relationship between vitamin D level and
severity/death is strong well into the range above 30ng/ml, then, at
least for people over 40, we can draw another line very approximately,
on a chart such as the above, depicting the continuing benefits of
improving one's vitamin D levels even if they are 30ng/ml, assuming
that one is going to get COVID-19 sooner or later. Perhaps
the benefits of increasing vitamin D levels, in terms of coping well
with COVID-10, continue well into the 40, 50 and 60ng mil range,
at least for a subset of the population with one or more risk factors for COVID-19 severe symptoms, such as advanced age,
obesity, lung injuries, diabetes, particular
haplotypes etc.
On the above
speculative basis here is the same chart, but with a line
I drew in, based on a WAG (a SWAG [
W]
not necessarily expert or rigorously scientific) of what the risk of
suffering, lasting harm and death would look like, for people
aged 40 and above, according to vitamin D levels AND COVID-19
infection, considering all the comorbid conditions which tend to
accumulate with age (though most would accumulate much more slowly if
everyone had > 40ng/ml 25OHD):
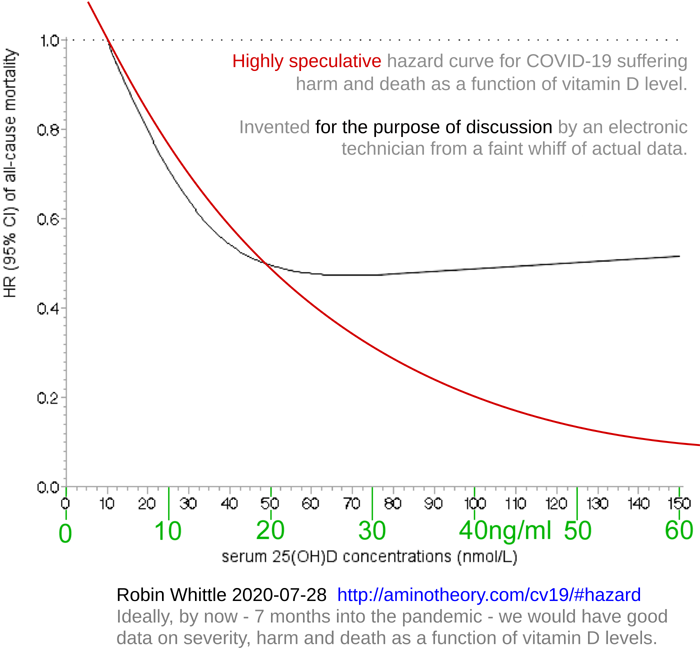
While this is highly speculative, the Iranian data indicates clearly
that COVID-19 patients in hospital who have less then 30ng/ml vitamin D
do significantly worse than those with more than this.
So even if the pre-COVID-19 hazard rate for death curve really did
flatten out above 30ng, and the hazard curve for suffering and harm
(which as far as I know is not calculated, since it is very hard to
define and measure) did the same, then the the fact that the COVID-19
curve continues to provide better health above 30ng/ml means we should
raise our levels more.
Its not radical to aspire to 60 or even 100ng/ml (the high end of
normal, according to the Endocrine Society). But such a statement will make many doctors twitch,
especially those in the UK.
Even if the pre-COVID-19 hazard curves, for suffering, harm and death
really do go slightly upwards beyond 30ng/ml, if the curves for COVID-19 go
down more over that range of 25OHD levels, which would not be
surprising, then we would again do well to raise our vitamin D levels.
Of course, if we have already had COVID-19, did OK with it, believe
correctly that we are never going to get it again, or if we get a
vaccine soon and are very sure it is going to protect us, then the
COVID-19 hazard curve is irrelevant and we can,
according to theory, rest on our laurels at 30ng/ml.
#2020-Baktash
Baktash et al. in Southern England: Elderly COVID-19 patients have low vitamin D levels
Researchers in Slough, west of London,
report on a cohort of 105 elderly (65 years and greater, av. age 81)
hospital patients with symptoms matching those of a viral infection in
March and April 2020.
The 35 patients not diagnosed with COVID-19 had median 25OHD vitamin D levels of
20.8ng/ml and the 70 who were diagnosed with COVID-19 had mean 25OHD levels of
10.8ng/ml. There is no data on the levels of aged matched healthy controls.
In these observations, interquartile range (IQR) is a measure of the
distribution of values such that 25% of subjects have levels below the
first value and 25% have levels above the second value. So this
range encompasses the values of half the patients.
The interquartile ranges of the non-COVID-19 patients was 12.6 to
28.6ng/ml. The COVID-19 patients range was 8.0 to
18.8ng/ml. The significance of these mean and IQR
differences was p = 0.0008, which means that if there really was no
mechanism for such a relationship, observations with this divergence
would only be made about once in 1250 trials.
The patients were 76% Caucasian, with 21 South Asian, 2 East Asian and
4 Afro-Caribbean. The COVID-19 group were 60% men and on average
3.2 years younger then the non-COVID-19 group, who were 57%
women. Eyeballing the chart above
#2020-UK-vit-D-BAME
I estimate that at this time of year, in the whole of the UK, much of
which is more northerly, the average 25OHD levels for an ethnicity and
sex mix matching the COVID-19 group would be about 15ng/ml.
However, this is for all adults and people in their 80s typically have
lower levels unless they supplement with D3 at higher levels than the
very small 0.01mg (400IU) day recommended by the UK government.
Like many MDs in the UK, these researchers considered the threshold of
vitamin D repletion to be only 12ng/ml, and gave patients with levels
below this a 0.01mg (400IU) supplemental dose of vitamin D3.
(This article cites the
fake Alipio article.) Some quotes:
Vitamin
D has been shown to condition the innate immune reaction against both
bacterial and viral infections. Calcitriol 1,25OH, the active form of
vitamin D, modulates macrophage activity by inhibiting the release of
pro-inflammatory cytokines such as IL-1, IL-6, IL-8, IL-12 and tumour
necrosis factor-alpha. Vitamin D shifts the adaptive immune
reaction from a Th1 to a Th2 phenotype, downregulating differentiation
of naïve T cells into pro-inflammatory Th17 cells, and promotes T
regulatory cell induction. Dysregulation of both innate and
adaptive immunity, as a result of vitamin D deficiency, may therefore
be central to precipitating the "cytokine storm" seen in COVID-19
infection.
In addition to anti-inflammatory properties, vitamin D also exerts a
protective effect on human alveolar epithelial cells by promoting wound
repair. Vitamin D has also been shown to preserve endothelial
integrity and deficiencies result in increased vascular permeability
and leak.
Vitamin D also increases the expression of ACE2. While increased
ACE2 expression in the early pandemic was predicted to increase the
risk of infection, paradoxically, ACE2 has also been shown to protect
against acute lung injury.
|
#2020-Shakoor
Shakoor et al. Be well: A potential role for vitamin B in COVID-19
The B vitamins are rarely mentioned in
articles concerning immunity and COVID-19, but vitamin B1, Thiamine, is
a key feature of Paul Marik's ICU protocol, which predates COVID-19 by
several years, and is the basis for the MATH+ protocol:
icu/#Marik-protocol ,
https://covid19criticalcare.com as explained in an
article MATH+ Protocol for the Treatment of SARS-CoV-2 Infection: The Scientific Rationale Paul E. Marik, Pierre Kory, Joseph Varon, Jose Iglesias & G. Umberto Meduri.
Here is an article focusing on the B vitamins:
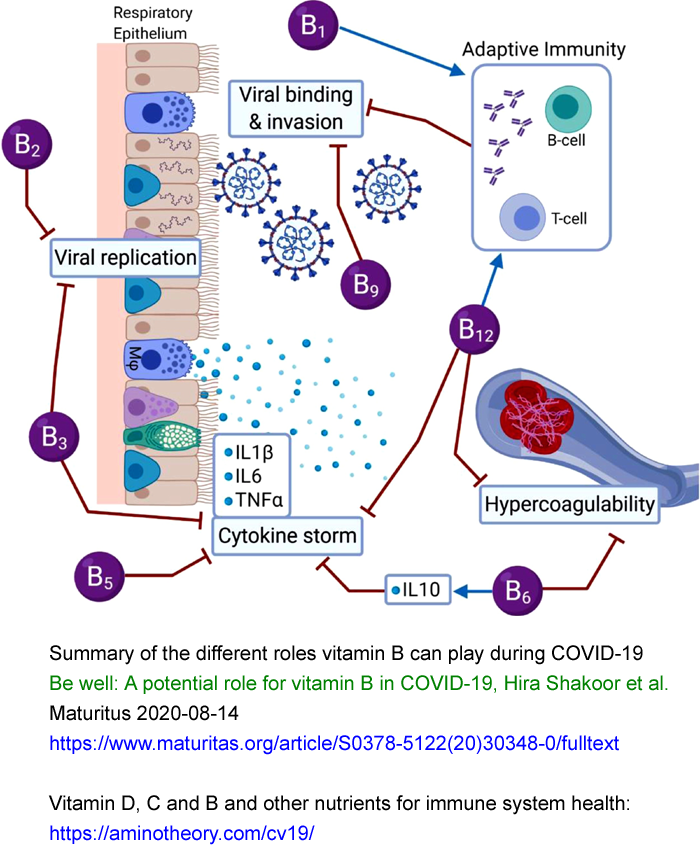
Low
levels of vitamins D and C result in coagulopathy and suppress the
immune system, causing lymphocytopenia. Evidence has shown that the
mortality rate is higher in COVID-19 patients with low vitamin D
concentrations. Further, vitamin C supplementation increases the
oxygenation index in COVID-19 infected patients. Similarly,
vitamin B deficiency can significantly impair cell and immune system
function, and lead to inflammation due to hyperhomocysteinemia.
There is a need to highlight the importance of vitamin B because it
plays a pivotal role in cell functioning, energy metabolism, and proper
immune function. Vitamin B assists in proper activation of both
the innate and adaptive immune responses, reduces pro-inflammatory
cytokine levels, improves respiratory function, maintains endothelial
integrity, prevents hypercoagulability and can reduce the length of
stay in hospital.
|
Regarding B vitamins used with vitamin D research projects dealing with specific conditions, with 25OHD targets above the
40 to 60ng/ml
range unrecommended by recent research articles mentioned above (and so
even further above many MD's 12 to 30ng/ml standard of repletion)
please see this
Vitamin D Wiki page, which results from 2019 interviews with researchers:
They all use magnesium, vitamin K2, omega 3 fatty acids and one or more
of the B vitamins. Two also use boron, zinc and C0-Q 10.
The majority of Italian COVID-19 patients are vitamin D deficient
It might seem obvious, but unfortunately, nutrition is still widely overlooked in the hospital setting.
Our preliminary analysis clearly shows that the majority of patients admitted with COVID-19 have a vitamin D deficiency.
I hope that COVID-19 and that research, such as my own and the other
studies, are seen and taken as our chance to develop a well-designed
preventive campaign that puts nutrition and tailored vitamin
supplementation at the core of preventative medicine.
|
Latitude and COVID-19 severity - solar UV exposure and vitamin D
I have not yet had time to read this article, but it looks interesting:
Death rates correlate with high northern latitude. There is too little data at southern high latitudes to be significant.
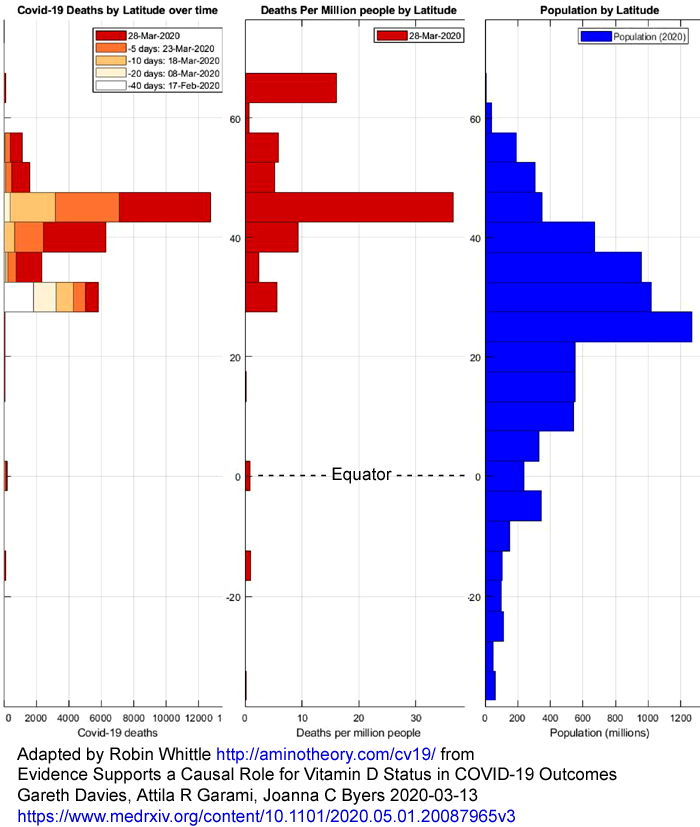
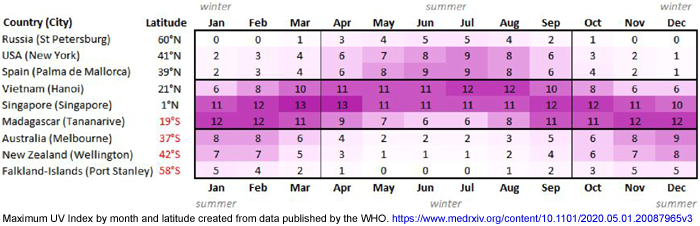
There is also a critique of RCTs (Randomized Clinical Trials), citing
the work of several other researchers on this topic - regarding some
RCTs not meeting proper requirements and their results incorrectly
being being ascribed greater validity than observational studies.
#az-trial
Arizona State University trial of vitamin D to reduce COVID-19 severity
This trial is due for completion on
2020-08-18. It involves robust vitamin D3 supplementation with
the aim of determining whether this reduces the severity of COVID-19
symptoms:
The supplementation levels are high enough to effect significant change
in 25OHD levels, though this will depend on absorption and on how fast
the liver converts the D3 to 25OHD:
Take a vitamin D supplement daily for two weeks, at a dosage of 10,000 IU/day (0.25mg) b.i.d. (age 18-69 years) or 15,000 IU/day (0.375mg) t.i.d. (age 70+)
After
two weeks of taking vitamin D, return to SCNM for a blood draw to
remeasure levels of vitamin D, comprehensive metabolic panel, and
complete blood count with differential. If vitamin D levels are still
below 30 ng/ml, continue the dosage for 3 more weeks. If vitamin D
levels are 30-49 ng/ml, continue at a dosage of 5000 IU/day. If vitamin D levels are 50+ ng/ml, stop supplementation.
|
This medical abbreviation (acronyms?) decoder
http://www.cwladis.com/math104/lecture5.php
tells us that "b.i.d" means twice a day and "t.i.d" means three times a
day, so this would refer to frequency of taking 0.15mg (5000IU)
capsules.
#veracity #2020-Raharusun #2020-Alipio
Reports of research from Indonesia and the Philippines which I
previously accepted and quoted are, in my opinion now, completely
fictitious
Please see my new site:
for all the reasons I now believe these two articles
(and one other not cited here) concerning vitamin D and COVID-19 are
fabricated. Please read the material there and make up your
own mind, rather than taking my word for it. I am not an
authority..
Important update 2020-07-27:
See the following article in which three Indonesian MDs find no trace
of the purported authors of the above article. This includes
searching the Indonesian Medical Council database and contacting the
hospital mentioned in the article :
COVID-19 and Misinformation: How an Infodemic Fueled the prominence of Vitamin D
Joshua Henrina, Michael Anthonius Lim and Raymond Pranata
British Journal of Nutrition 2020-07-27
https://doi.org/10.1017/S0007114520002950
|
I apologise for not scrutinising these articles more carefully at
first. I had no idea that anyone would write completely fictional
documents posing as academic articles.
23% of the Indonesian population is
vitamin D "deficient" (25OHD < 20ng/ml). "The examination of Vitamin
D status is not a routine in Indonesian clinical setting." Of 10
COVID-19 patients average age 49.6 in Bethesda Hospital Yogyakarta, 9
were deficient and 1 was "insufficient" (20 to 29ng/ml).
Their levels were (patients sorted by age):
Pt. 25OHD Comorbidities (HT = hypertension.)
Age ng/ml Symptoms (Fever, Fatigue.)
7 14F 8.3 -
3 17M 20.5 -
4 40M 11.9 Fa, Fe, dry cough
1 49F <8.1 Fa
2 51M 10.6 Diabetes Fe, diarrhea
8 54F 10.1 Fa, headache
10 64F <8.1 HT, post stroke Fe, dry cough
5 65F 11.6 HT Fa, Fe, headache
9 69M <8.1 HT Fa, dry cough
6 73M 12.4 HT COPD Fa, Fe, dry cough
All patients received 2000IU oral D3 a day.
Singapore trial of 1000IU vitamin D3, B12 and magnesium
On 2020-06-10 the results of a small trial in Singapore were published:
The patients were all over 50 years
old, not requiring oxygen therapy. The control group of 26 were
admitted before the trial began. The intervention group of 17
patients received, daily, on average for 5 days:
- 1000IU vitamin D3.
- 150mg magnesium (compound not specified).
- 500ug vitamin B12.
The intervention group was younger than the control group (average 58.4
to 64.1) and had a greater number of comorbidities (14 over 17
patients, compared to 49 over 26 control patients). The
intervention group required less oxygen therapy (3 = 17.6% to 16 =
61.5%) and only one of them required ICU treatment, compared to 8 of
the control group. Of the 3 intervention group patients who
required oxygen therapy, 2 had only been treated for one day.
This is a small, non-randomized, non-blinded trial, conducted under
"difficult dynamic circumstances" with modest vitamin D3 and magnesium
doses and with no record of 25OHD levels. The authors claim that
after correcting for age and comorbidities, that the DMB intervention
was associated with significantly better outcomes - and this includes
with the two patients who were only treated for one day.
Research from Belgium, Louisiana, a homeless shelter in Boston . . .
In this Belgian retrospective study, male but not female
COVID-19 hospital patients had lower 25OHD levels than controls whose
levels were sampled at the same time of year. However, the
controls were all "diseased" in that they were attending or admitted to
hospital too.
In males, but
not females, there is a clear correlation between low vitamin D and
COVID-19 disease severity:
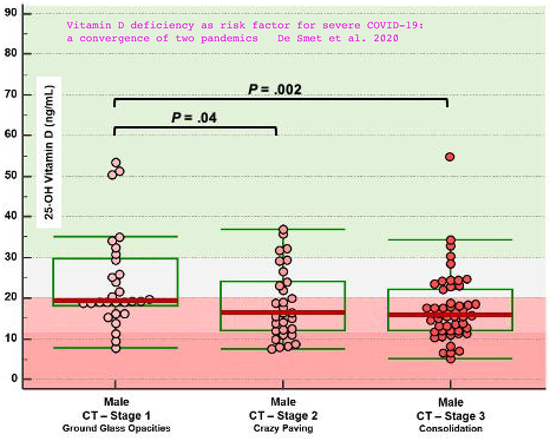
There's no record of to what extent any of these patients
or controls were supplementing with vitamin D3. Nor are there
data on 25OHD levels for age matched non-hospitalised controls.
There are
numerous items of interest here, including:
In
Louisiana, African Americans account for 70% of COVID-19 deaths despite
representing only 32% of the population. In a Boston homeless shelter,
100% of 147 COVID-19 positive subjects were asymptomatic.
|
COVID-19
hospital patients in ICU, on average, have lower vitamin D
levels than those not in ICU. Of these 19 ICU patients, 17 are
African American. 17 of these patients have 26ng/ml 25OHD or less.
408 people in a homeless shelter in Boston were PCR tested and 36% were
positive for COVID-19. Their average age was 53.1. They had no
serious symptoms, and a remarkably low incidence of minor symptoms:
7.5% cough, 1.4% shortness of breath and 0.7% fever - and these rates
hardly differed from those who tested negative, average age 50.8.
Homeless
people are more exposed than average to sun, and therefore
might be expected to have higher than average vitamin D levels, even
without supplements. They also get more exercise - and I suspect few of
them are as old as those in their 70s and 80s who suffer the worst harm
from COVID-19. They are probably less likely to use drugs to
lower fever, though I guess they would often find it harder to keep
warm and so sustain any fever which was helping them fight the
coronavirus.
Also, perhaps they smoke more - and there is some evidence of smoking being protective:
. . . . France (nicotine?), Ireland . . .
File this under "COVID-19 curve-ball": 25.4% of
the French population smoke. 4.4% of a COVID-19 inpatient group
smoke and 5.3% of an outpatient group.
A large survey of Irish males 40 to 60 yo revealed they had a median
25OHD level of 18.8ng/ml. 25% of
them had 16.4ng/ml or less!
25% of them had 26ng/ml or more. So, assuming for the moment that
the Indonesian and Philippino reports above are relevant to Irish men
(and ignoring any nicotine use) most of these Irish men are at much
higher risk of serious harm and death from COVID-19 than if they
supplemented with vitamin D3 to bring their 25OHD levels well above
30ng/ml - say to the 40 to 50 range.
The report concerns 33 males 40yo and above with COVID-19 pneumonia and
respiratory failure. None of them suffered from cancer, diabetes,
CVD or had received chronic immunosuppressive therapy. 12 were
placed on mechanical ventilators and four of these men died. The
21 who did not need mechanical ventilation had mean 25OHD 16.4ng/ml, while the 12 who needed
this had mean 25OHD 10.8ng/ml.
All these levels are very low. indeed.
2015: Severe vitamin D deficiency in Italian children with Kawasaki disease
By mid-May 2020 it has become clear that some
children are suffering
severe symptoms from COVID-19 - and some of them are suffering serious
harm or are dying. The
inflammatory symptoms are similar to Kawasaki disease and it is
reasonable to regard such cases as instances of
Kawasaki disease [
W].
However, due to some specific disease features - presumably due to
particular characteristics of the SARS-CoV-2 infection - and its sudden
wide prevalence, a new diagnostic category has been created for this
condition when triggered by COVID-19:
Paediatric multisystem inflammatory syndrome [
W]. Here I will use "KD" and "Kawasaki disease" to include both diagnostic categories.
Here is a
2015 article of crucial importance from Italy:
Severe vitamin D deficiency in
patients with Kawasaki disease: a potential role in the risk to develop
heart vascular abnormalities?
Stefano Stagi et al. Clinical Rheumatology volume 35, pages 1865–1872
(2015)
https://link.springer.com/article/10.1007/s10067-015-2970-6 (Paywalled.)
https://sci-hub.se/10.1007/s10067-015-2970-6
Google Scholar 13 citations (2020-05-29)
On 2020-05-30, as best I could tell, none of the numerous academic
journal articles concerning Kawasaki disease and COVID-19 cite this
one. See below #kdarticles
below for a link to the list of such articles. I wrote to the corresponding authors
of all these articles pointing them to this Stefano Stagi et al. 2015
article.
Every such article should cite this one, because there is no other way
of understanding the etiology of Kawasaki disease, how to prevent it,
or how to cure it, if the central and surely causative role of vitamin
D deficiency is not fully recognised. This is true whether it is
triggered by COVID-19 or any other condition.
|
|
The patients were 21 girls and 58 boys, average age 5.8 years.
Their average 25OHD levels were
9.2ng/ml, while age-matched controls averaged 23.3ng/ml. In the patients
who developed coronary artery abnormalities, the average 25OHD
level was
4.9ng/ml (sd 1.36).
These children, due to the decisions made by adults, were
struggling to live with vitamin D 25OHD in their bloodstream 20%
to 11% of what is normal for hunter gatherers in Africa.
https://www.ncbi.nlm.nih.gov/pubmed/22264449
These children are severely
vitamin D deficient. What is hard about this? For heaven's
sake give children vitamin D supplements so they never have to suffer
and die
like this! All children before they get ill, and especially these
KD children who have such low levels. Why are so many doctors resistant
to vitamin D
supplementation when most people, without supplements are deficient?
More on Kawasaki disease in sections following the next one.
Ending the global vitamin D deficiency pandemic
Inadequate vitamin D levels - such as
25OHD levels below 40ng/ml (100nmol/L) - are a slippery slope leading
to multiple forms of ill-health, disease and sometimes
death. This is a global pandemic. See the Google
search results for
vitamin D deficiency pandemic .
We are now living in what I hope will be the last months or year or so of the
Vitamin D Dark Ages.
Future generations will look back in bewilderment that we had such
sophisticated technology, hospital care and social and scientific
achievements - yet still expected most people to live with inadequate
nutrition, including especially vitamin D. This will be clumped
together with other
health-horrors-now-thankfully-and-firmly-in-the-past: The days
before sewerage systems; hand-washing and basic sanitation;
antibiotics; vaccines; anesthetics; chemical analysis of blood
and tissue samples; X-ray and MRI machines; Internet access to health
information and lively discussions like this one . . . .
The days when many people, including many doctors,
smoked. (They still do in China.)
It is not practical to repeatedly test the 25OHD levels of every person
on Earth. This would be far more trouble and expense than the
vitamin D supplements themselves. There are some concerns about
vitamin D toxicity (
link)
among a small fraction of the population, which I want to analyse and
write more about later - but in general everyone needs to get their
25OHD to 40ng/ml or more in order that their immune system works
correctly. This goal is at odds with the advice given by
some, such as
#21authors, that we should aim for 25OHD levels merely above 10ng/ml (25nmol/L).
Here are some arguments for robust vitamin D supplementation to ensure
25OHD levels above 40ng/ml which will ensure, in most people, strong
initial immune responses to infections and well-regulated later
responses with good resolution mechanisms - not the overly-aggressive,
pro-inflammatory, self-destructive responses which cause the harm in
Kawasaki disease, COVID-19 and many other conditions.
I am using Kawasaki disease (see the article linked to in the previous
section) in children as an example, but the principles apply to people
of all ages, and for all sorts of conditions - of which COVID-19 is the
one which most urgently demands our attention.
The estimated vitamin D intakes of the KD children did not differ
significantly from those of the control group. The numbers
in brackets are the standard deviation [
W].
Significance [
W]
values show the probability that this difference would
occur by chance due to random differences even if there was no actual
relationship between the two variables. NS means the difference
is not statistically significant - in this article, below 0.05.
NS means that there is a greater than 1 in 20 chance the difference in
these observations could occur due to random variation
rather than due to a real cause.
|
Control |
KD |
Significance |
Vitamin D from diet IU/day
micrograms
|
209(43)
5.2
|
220(49)
5.5
|
NS |
Vit D supplementation in prior 6 months
|
10.7% |
11.4% |
NS |
25OHD vit D ng/ml
KD children with heart damage
|
23.3(10.6) |
9.17(4.9)
4.92(1.4)
|
< 0.0001 |
Only
about 11% of the children had received vitamin D supplements in the
past 6 months. We don't know how much they were given, or how
these children's 25OHD levels differed from those who were not
supplemented. The control group's 23OHD level of 23.3ng/ml is (I
guess) about the same as for many adolescents and adults.
However, older people, and those with darker skins would have generally
lower levels.
A simplistic analysis of this might be that the KD children had the
same (or slightly more) vitamin D intake as the controls (their
sunlight exposure and sunscreen use was about the same too) and that
a viral or bacterial infection trigger caused their 25OHD levels to plummet in the course of
their illness. In this basis, there might be no argument for
greater vitamin D supplementation to prevent illness.
There are, of course, strong arguments for supplementing these children
with vitamin D once they are ill. However I have not found any
reports of doctors doing this. It seems that most doctors are
unaware of these low vitamin D levels, or consider them insignificant
or at least not amenable to change once in hospital. I am not a
doctor, but it seems obvious to me that these children should get oral,
intravenous or intramuscular 25OHD (25 dihyhdroxy vitamin D =
calcifediol = Rayaldee) supplements as a matter of urgency, since this
will directly raise the blood 25OHD their immune system relies upon.
Failing this, they should at least get oral vitamin D3, which will take
some days to be converted by their livers into the circulating 25OHD.
It is possible that the viral infection (and the direct, helpful - even
if weakened - immune response to it) and/or the KD disease process
itself (which is a self-destructive dysregulated immune response)
depletes 25OHD
levels. I am still researching this, but I think there is limited
evidence for substantial declines like this in any illness.
The
half-life of 25OHD in adults is weeks, but I guess it might be shorter
in
children. Being ill, they may have been out of the sun for a
month
or so by the time they were admitted to hospital, and they may have not
been eating well, absorbing vitamin D3 or converting it in their livers
to 25OHD in the bloodstream. So even without direct effects
of the viral or KD illnesses, we might expect these children's 25OHD
levels to drop a few percent to 30% (my guess) over this month or so of
ill-health.
(Whatever small amount of boron they might have had from their normal
food - fruits, vegetables and nuts mainly - would be rapidly depleted
if they stopped eating this due to illness. The half life in
adults is less than a day. Hospital food probably has little or
no boron, since it is not recognised as a nutrient.)
Accepting that some non-trivial fraction of the difference between 25OHD levels of the control and KD children is
caused by the viral illness and the immune system's subsequent attack
(all the KD literature indicates that KD occurs weeks after the peak of
viral replication),
here is my attempt
to explain the causative role of vitamin D deficiency in Kawasaki
disease in general, KD or anything like it in children due to COVID-19 and
more generally severe symptoms from COVID-19 in adults.
For
completeness, this explanation also attempts to cover severe outcomes for adolescents whose disease progression
differs significantly from that of KD and of adult COVID-19. Adult
COVID-19 severe symptoms result from viral replication in the lungs
driving endothelial damage and a resulting hypercoagulative
state.
icu/ KD does not seem to involve the lungs so much, and most of
the harm is observed in mid-sized arteries - especially those supplying
the heart muscles - though I think stroke is also a cause of harm and
death.
We start with a population of children of suitable age for KD, before
any disease trigger. We assume that the dietary vitamin D
estimates and those for sunlight are valid and that the 23.3ng/ml
average 25OHD levels of the control group apply to this whole group.
The first thing to note is that although the Endocrine Society
regards levels of 30ng/ml or as being replete, 23.3ng/ml is too low by
a factor of
about 2. It is half the average level of 25OHD in African herders
and hunter gatherers. See
#2020-Baker-a and
#2016-Caprio below for why we should aim for 40 to 60ng/ml.
Assuming (for simplicity in this example) a Gaussian distribution [
K]
the 10.6 standard deviation indicates that 16% of these children have
25OHD levels below 12.7ng/ml, which is
very low. Let's take these
children and call them subset
AA. The reasons for these low levels include some mixture of:
- These children, on average, had lower than average (for the
entire initial set of children) vitamin D3 intake from food and
supplements.
- Darker skin pigments. (Dark skinned people also have more
melanin and another uncoloured protein in their skin which absorbs the
UVB light before it can reach the lower parts of the skin where vitamin
D3 can be made.)
- Less skin exposure to sunlight with UVB, due to latitude,
clothing, sunscreen, air pollution, lifestyle, living in dense urban
environments etc.
- Poor absorption of D3 in food and supplements due to genetic
differences, nutritional differences (not yet known, but they likely
exist), whether or not the D3 was taken with a fatty meal - which is
best for absorbing this fat-soluble vitamin - and potentially other
unknown reasons.
- Genetic or other reasons why the D3 is not converted to circulating 25OHD so well in the liver.
- Body size variations and fat storage diluting the D3 in the whole body so there is a lower concentration in the blood.
- Genetic, nutritional and other currently unknown variations
affecting the quantity of vitamin D transporter protein in the
blood. This affects the availability of 25OHD to the immune
system cells.
- Likewise other variations in the genes which determine the
structure of this transporter protein, and in the proclivity of 25OHD
to bind to any other proteins there (I recall albumin is one of them).
Now, by some magical means, we sort these children AA according to
their genetic proclivity to mount an overly-aggressive pro-inflammatory
immune response to infection
even
if
they were replete in all nutrients including vitamin D and any we
currently know little about (such as boron) which affect immune
functioning.
This proclivity is due to numerous types of genetic variation
concerning their immune system cells, on top of the general human
tendency for our inflammatory immune response to be overly-aggressive
due to the fact that we have no intestinal worms. (See
#helminthsgone
below.) Let's pick the 20% of these AA children with the most
destructively dysregulated immune responses, and call them group
BB.
BB are 3.2% of the initial group of children whose age made them possibly at risk of KD.
Now I will assume that 5% of these BB children - group
CC - are infected with SARS-CoV-2. This is 0.16% of the initial set of children.
Ignoring, for simplicity, genetic variations in the virus, some
children will get a mild initial dose and others will get a large
initial viral load, which is inherently more difficult to fight.
There could be 100 to 1 variations in the viral load these children get.
Some of these SARS-CoV-2 infected children will develop a fever.
Of these, a fraction will be given drugs to lower that fever. As
far as I know, from all the research
fever/ I
found regarding viral infection fevers in general - not specific
to COVID-19 - this is a bad idea, and is likely to cause a weakened
innate and adaptive antiviral response, and so a greater chance that
the infection will worsen and so increase the likelihood of triggering
KD.
Assuming the lack of helminths and genetic variations in
overly-aggressive pro-inflammatory responses are not important in the
initial stages of the infection (in the throat, or perhaps the eyes),
there will be some inherent genetic variation in how strongly the
children can fight the virus, even if they were replete in all
nutrients.
However, all of group AA, BB and CC are
very
low in vitamin D (less than or equal to 12.7ng/ml in this example), and
this greatly reduces the ability of their innate (at first [
K]) and later adaptive [
K]
immune systems to fight the virus directly. So we expect some
fraction of the CC children not to stop the viral infection in the
first few days.
I will assume this is 20%. For these children, group
DD,
the virus replicates in large numbers in their lungs, blood vessels or
wherever else it is active in a way which tends to stimulate a
self-destructive immune response we later diagnose as Kawasaki
disease. This is group DD - now 0.16 * 0.5 * 0.05 * 0.20 = 0.08%
of the whole initial group of children - one in 1,250.
These children are in trouble - and these are the ones who, in general,
get Kawasaki disease or whatever else their condition might be called -
severe symptoms with possible lasting damage the heart and other
organs, triggered by COVID-19.
The short version of this story is that a SARS-CoV-2 viral infection
has triggered KD in a relatively small subset of all children,
according to the combined effects of various circumstances as just
described. I have assumed a sharp cutoff of 25OHD 12.7ng/ml to
denote the children at risk of KD. In fact, there is no sharp
cutoff. Some children with higher levels will get KD - presumably
due to some bad combination of all the variables just mentioned.
Still, for discussion, this 12.7ng/ml sharp threshold is good enough.
Now lets re-run the situation with one major change. This change
is easier to make than changing lifestyle, urban shadowing, culturally
driven patterns of clothing and sunscreen use, or food choices.
This change is also a hell of a lot easier than coping with the
situation described above, in which some children - thousands to
hundreds of thousands in any one country as COVID-19 affects almost the
entire population - suffer illness, lasting harm and perhaps death,
with all the efforts at treatment etc.
The change is that with the support of most doctors and the government,
the great majority of parents recognise the need to get their
children's 25OHD levels safely at or above 40ng/ml. This means
lifelong robust vitamin D supplementation
(except perhaps if, as adults, they spend a lot of time all-year round
in UVB rich sunlight without clothing or sunscreen protection).
It also requires robust vitamin D supplementation for women in
general and especially women of childbearing age, since their baby's
25OHD levels depend entirely on their own before birth, and frequently
after when they rely on breast feeding.
(This will also significantly reduce the incidence of autism and
probably numerous other health conditions. Low vitamin D in-utero
and/or early life seems to be a significant cause of autism:
https://www.scientificamerican.com/article/vitamin-d-and-autism/ .)
The whole set of children now average 46ng/ml 25OHD. The proportion of them with dangerously low 25OHD levels is now
reduced.
So the incidence of KD in general, and in response to COVID-19, will be
correspondingly lower. Likewise adolescents and adults regarding
severe symptoms from COVID-19 and numerous other chronic conditions and
acute diseases.
If doubling the average level also doubled the standard deviation, then:
Ave. SD Proportion below
25OHD 12.7ng/ml
23.3 10.6 15.9% calc
46.6 21.2 5.5% calc
in theory, 65% (
1 - (5.5 / 15.9))of
the children at risk of KD in the first scenario due to low vitamin D
levels would no longer be at risk. Likewise any other diseases
which strongly depend on low
25OHD levels.
If everyone supplemented about the same amount, to double the average
levels, the standard deviation would probably increase by less than a
factor of 2, as I have assumed here. The bell curve would be
narrower and the proportion of children with less than 12.7ng/ml 25OHD
would be even less than this. If the SD was 16, only
1.7% of the children would have 25OHD levels below 12.7ng/ml - a reduction of 89% from
15.9%.
In this future era of ubiquitous vitamin D awareness, any children
diagnosed with KD or similar conditions would be quickly treated with
extra vitamin D, ideally 25OHD, and any other nutrients which would
improve their immune system dysregulation. At present, this does
not occur, and hospital treatment relies on transfusions of donated
plasma with antibodies, anti-inflammatory drugs, aspirin and (as far as
I know - and though the doctors may not recognise this) probably a low
level of vitamin D3 which may be in the food or IV drips the children
receive once in hospital.
The same reductions in severe disease should apply for adolescents and
adults with COVID-19, sepsis, severe symptoms from influenza etc.
Come the revolution we will all have generally good levels of
vitamin D supplementation, generally good (40ng/ml) 25OHD levels and so
a great reduction in the incidence of severe disease states, with
prompt repletion as soon as such states are diagnosed.
COVID-19 induced Kawasaki disease in children and babies
Further to the two sections above:
It is reasonable to assume that when children infected with COVID-19
have severe symptoms and sometimes die from a condition closely
resembling Kawasaki disease, that in most cases they too were already struggling with
extremely low 25OHD levels.
According to these newspaper reports, on 2020-04-16, Alexander
Parsons became the youngest person in the UK to die due to
COVID-19. He was 8 months old:
(In mid May 2020, Google reports 6,050
pages on this child's tragic death.)
In the Daily Mail comments, VV, Cheshire wrote:
My daughter's immunologist told me they had 200 cases in 6 weeks in the
U.K. because of the instance in initially Asymptomatic COVID-19 in
children. There's usually only 300 cases of Kawasaki in an entire
year.
|
"Only 300 cases" a year? There are numerous bacterial and viral
triggers for Kawasaki disease, with SARS-CoV-2 being a novel, widespread
and potent one. But these extremely low 25OHD levels can at
best be only partly explained as a result of the disease (there are
some suggestions in research that the levels drop due to
inflammation).
It is obvious that most of these 300 children a year would not be suffering
Kawasaki disease if their 25OHD levels were not so extremely low.
While individual levels do vary, for any given body weight and intake,
surely if these children were properly supplemented, most of them would not
have this disease, no matter what triggering condition they have which
might have set it off in children with very low 25OHD levels.
NHS advice
https://www.nhs.uk/conditions/vitamins-and-minerals/vitamin-d/ is that babies to 1 year should take 240 to 400IU vitamin D3 a
day. This seems like a reasonable amount considering their small bodies.
mickyfin of Leeds wrote:
I
also read recently that around 40% of covid patients recovering from
treatment were also diagnosed with dangerous blood clots.
|
The comments are full of sorrow, grief and people apparently resigned
to all that is happening - both COVID-19 and the decades old pattern of
Kawasaki disease. I saw no mention of vitamin D or any
other preventative measures.
I am an electronic technician and computer programmer. I want
things to work properly - including especially people's bodies! I
wrote this comment to both newspapers, but in neither case did the
moderators approve it:
It
is reasonable to assume that children suffering severe symptoms from
COVID-19 - especially those with a condition resembling Kawasaki
disease - are struggling with extremely low vitamin D levels:
Severe vitamin D
deficiency in patients with Kawasaki disease: a potential role in the
risk to develop heart vascular abnormalities? Stefano Stagi et al.
Clinical Rheumatology volume 35 (2015)
https://sci-hub.se/10.1007/s10067-015-2970-6
The patients were 21
girls and 58 boys, average age 5.8 years. Their average 25OHD
(vitamin D) levels were 9.2ng/ml, while age-matched controls averaged
23.3ng/ml. In the children who developed severe coronary artery
abnormalities, the average 25OHD level was 4.9ng/ml. These
children, due to the decisions made by adults, were struggling to live
with vitamin D in their bloodstream about 10% to 20% of what is normal
for hunter gatherers in Africa: 46ng/ml (115nmol/L):
https://www.ncbi.nlm.nih.gov/pubmed/22264449
|
On 2020-05-30 I searched Google Scholar
for articles concerning this disease and COVID-19. I found none
which mentioned the Stefano Stagi et al. 2015 article
#2025-Stagi . I think this article is
the key to understanding, preventing and treating Kawasaki disease, no
matter what triggers it.
This outrigger page:
lists those 15 articles, with a few notes about the contents of
some of
these articles. See also below another 3 articles and the email I sent to the corresponding authors:
#more-KD-articles-1 .
I may have missed one or two, but I think this is
the great majority of the articles written about COVID-19 and Kawasaki
disease. None of them mention:
- The Stefano Stagi et al. 2015 article.
- Vitamin D.
- The word "vitamin".
- Nutrition.
The general picture presented by all of them is that the etiology is
Kawasaki disease is unknown, except that there is usually a viral
or bacterial infection trigger and that the fact that only some children get it is explained
by currently unknown genetic factors.
This is despite some of the articles observing a disproportionate
number of sufferers being dark skinned (living in Paris, for instance)
and that in Japan, the peak incidence coincides with
winter.
The average person would quickly link these observations to the
possibility that vitamin D deficiency was a significant contributing
cause to the disease.
However, these doctors do not think of this. Some studies
included lab tests on numerous compounds associated with general health and inflammation, but 25OHD was never mentioned.
I know there is a problem with the volume of research, but
any academic article concerning Kawasaki disease is affecting matters
of life and death, and so should be based on the best available
knowledge of the cause of the condition, and of measures to prevent and
cure it.
The Stefano Stagi et al. 2015 article is good research of
immense importance.
Perhaps some contributing reasons to it being only occasionally cited
are that it is behind a paywall and that it is in a rheumatology
journal - and so may not be seen by the heart and vascular
specialists who tend to work on Kawasaki disease.
#2019-Meyer
A 2019 article on Kawasaki disease does mention vitamin D and cites Stagi et al. 2016:
This is a retrospective study of
Kawasaki disease in German children, with a control group made up
largely of children who were in similar families - often friends of the
families of the KD children.
The researchers had no information on vitamin D levels in any of the
children. They drew on medical records of the KD cases, which
included various details of their condition and treatment. This
indicates that in general, the doctors treating these Kawasaki disease children had no interest in their vitamin D status.
The researchers attempted to find a correlation between the incidence
of KD and the length of vitamin D supplementation from birth and of
breastfeeding. Some correlation was found, but I think it is of
little interest, since the median age of KD onset was 30 months and
vitamin D supplementation ended on average after 5 months. Of the
79% of KD patients who were supplemented, 27% were "irregularly"
supplemented, and there is no information on the dosages.
Breastfeeding data was even less precise, with 21% of KD patients being
breastfed for less than 2 weeks and no data on how long the remainder
were breastfed. Nor was there any information on the mothers' 25OHD levels, or those of the milk itself.
By 2.5 years, there would be no effect of that breastfeeding or vitamin
D supplementation on actual 25OHD levels. There might however be
some correlation with the children's general nutrition and/or some
lasting effects of the original breastfeeding and vitamin D
supplementation on the children's immune systems.
In Germany, vitamin D supplementation generally is recommended for the first year of life. |
As you will read in these pages, to safely reach or exceed 40ng/ml 25OHD -
which seems to be the minimum required for proper immune system
functioning - all people, from birth, need supplements, with the
possible exception of those who spend so much time in the sun all year
round that they produce enough D3 themselves.
The 1 year recommendation is obviously too short, but it did did result
in more than half of the children being supplemented for 5 or so months
to start with.
#more-KD-articles-1On
2020-06-11 I found two more articles concerning Kawasaki disease and
COVID-19, both with clinical details, plus another two discussing
these. I could probably have found more if I searched assiduously.
The first three are written by 28 medical doctors and one PhD. There is
NO mention of vitamin D!!
It should be obvious to anyone with an understanding of immune
dysregulation and vitamin D, and who is aware of the low 25OHD levels
in child (KD) and adult COVID-19 patients with severe symptoms, that
these symptoms are both, in large part, caused by
inadequate vitamin D.
Of all the things I have ever researched, this is the greatest mystery:
Why are so many doctors so ignorant of, so blind to, or whatever, the
importance (generally causative) of inadequate vitamin D and a these
two acute conditions which are affecting hundreds of thousands and soon
millions of adults and children all around the world?
On 2020-06-11 I wrote to the corresponding authors of these articles,
and of the 15 mentioned above, a message you can read here:
kd/#msg
. I won't mention details of any correspondence, but will add a
note here if and when I receive any replies. (5 days later . . .
. nothing.)
UK discussion about BAME community susceptibility to severe COVID-19 symptoms generally ignores vitamin D
In mid-June 2020, the tide is turning
and more people are seriously considering the low vitamin D levels of
Black, Asian, Minority Ethnic (black and brown skinned) people in the
UK regarding their much greater share of COVID-19 harm and death.
So hopefully the above heading will soon be be a footnote in history,
rather than referring to tragic reality.
Please
see the graph I added on 2020-06-20
above #2020-UK-vit-D-BAME which shows seriously low vitamin D level for UK White people and disastrously low levels for BAME people.
Here is an article, one of many
concerning the much greater death toll among Black, Asian and Minority
Ethnic people in the UK - especially among doctors and other healthcare
workers.
I wrote a response to this.
I wanted to write a similar response to an article in Unherd,
concerning a hypothesis, which I disagree with, that the majority of
people are already immune to the virus without being infected.
However, Unherd's discussion system, like that of the above BMJ page,
is controlled by Disqus, and I am concerned that by writing something
similar, the Disqus system will regard me as a spammer.
My response is on a separate page here:
bmj-gopal-response/
On 2020-06-15 I was happy my comment, the first, was accepted for this
Conversation.com article on the BAME COVID-19 tragedy, which
does mention nutrition for immune system:
#SAAD
This 2020-05-26 article
http://www.pulsetoday.co.uk/.../20040871.article * reports on a team of doctors north of Manchester (Dr Mohammed Jiva and colleagues, Rochdale and Bury LMC
staff.php) who developed a Safety Assessment and Decision scorecard (SAAD), which commemorates their colleague,
Dr Saad Al-Dubbaisi, who died of COVID-19. (
Article on hundreds lining the streets for his funeral procession.)
* I was able to access this
article at first, but not a second time. Clearing my browser's
cookies for www.pulsetoday.co.uk enabled me to see it again.
Side note on geography and music:
Bury is 53.6° north of the equator. So is Wigan, where my father Jeff was born - and Wigan gets a mention in the KLF's Its Grim Up North .
This is like living 900km south of the southern tip of the South
Island of New Zealand, with its glaciers and all. Heaven help the
Scots!
Here's a live performance of Justified & Ancient,
with Tammy Wynette, Maxine Harvey and Ricardo da Force all warming this
world immeasurably - the last two BAME, though I think the term didn't
exist in 1991: https://www.youtube.com/watch?v=f1PNnDagj6s .
This is my absolute favourite.
Here is my adaptation of the SAAD scorecard, with 25OHD levels in both ng/ml and (x 2.5) nmol/L:
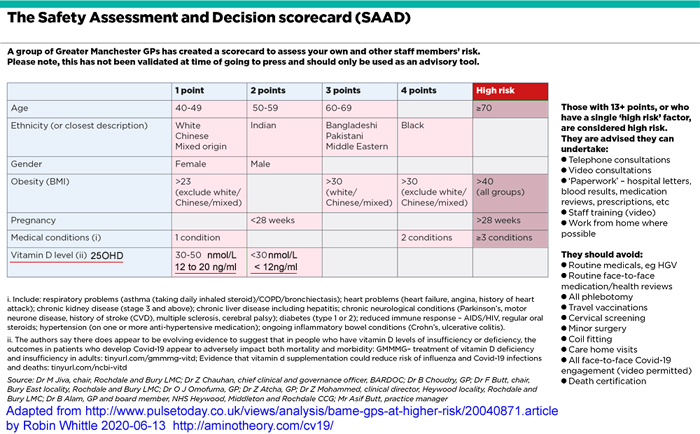
Here is a bigger version:
SAAD_table--ng-per-ml--1000x620.png .
They only consider low vitamin D levels a risk factor for COVID-19
severe symptoms and death if 25OHD is below 20ng/ml. See
#2016-Caprio below for arguments for raising 25OHD levels to at least 40ng/ml.
Low vitamin D levels may be
thought of as a risk factor along with other conditions like age, but
unlike all the other factors listed in the above table, it
can be changed within a week or so with substantial vitamin D3 supplementation - far more than the paltry
400IU/day recommended by the UK government. If anyone has 25OHD
below 40ng/ml, according to all the research I can find, there is are
very good arguments why they should raise that by robust vitamin D
supplementation as a matter of great urgency - to at least 40ng/ml, to
approximate, to the best of our knowledge, the levels our African
ancestors had when our immune systems evolved.
This would apply to virtually all people in the UK who were not already
taking substantial (4000IU or more) vitamin D3 supplements.
Low vitamin D levels in the UK population in general, and in BAME
communities in particular, have been recognised for years:
This recent article assumes a 20ng/ml threshold for vitamin D deficiency and cites 2013 research:
which found that, of 45 years and older people recruited at medical clinics, with
South
Asian (India, Pakistan and Bangladesh) and
Black
African-
Caribbean, background,
Male and
Female, the following percentages of people had 25OHD levels:
25OHD
ng/ml = nmol/L SA-M SA-F BAC-M BAC-F
>
20 > 50 7% 11% 13% 30%
12-20 30-50 17% 13% 34% 33%
6-12 15-30 36% 31% 41% 38%
< 6 < 15 40% 44% 14% 11%
These are "age adjusted" figures which I rounded to the nearest
integer. The article explains that for some conditions, SA and
BAC people seem to be able to cope with lower 25OHD levels than people
of European ancestry. Still, these levels are frighteningly low
for general immune health, and are clearly a significant factor in the
higher rates of harm and death among these people due to COVID-19.
These extremely low vitamin D levels, and their generally causative
association with a plethora of illnesses, have been known for
decades. I don't understand why governments, at the urging of
most doctors have not not implement programs to get everyone's 25OHD levels at least to above 30ng/ml. To this day (
#21authors, below), some in the UK use 10ng/ml (25nmol/L) as the threshold above which they consider 25OHD levels to be sufficient.
The past record of ill-health hasn't prompted this push for adequate
supplementation. Even now (mid-June 2020) with the deaths of so
many UK doctors, nurses and other health workers from their weak and
dysregulated immune system responses to SARS-CoV-2, there are just
murmurings about vitamin D, and lots more fuss about more
difficult-to-correct factors such as crowded homes and
workplaces. These affect the likelihood of contracting the virus,
while vitamin D levels have a profound effect on the incidence of
severe symptoms. Density of housing, use of PPE etc. are not decisive, because within months
most people will be infected anyway. The lockdowns necessary to really
slow transmission are not sustainable for more than a few months.
There are many reasons to believe that a truly safe, effective, vaccine
for SARS-CoV-2 in all its variations will never be possible. Even
if it was, it would take years to develop, test, refine and put into
billion-dose scale production. Individuals and governments
waiting for a vaccine to save the day any month now are completely
mistaken.
Robust population-scale vitamin D supplementation will be safer,
cheaper and vastly more effective than all the current investment in
drugs or vaccines.
The British Medical Association has a page devoted to the threat posed by COVID-19 to BAME medical workers:
https://www.bma.org.uk/advice-and-support/covid-19/your-health/covid-19-the-risk-to-bame-doctors
It doesn't mention vitamin D.
Dr David Grimes, from Blackburn, north of Bury, wrote on 2020-05-07
that all the doctors in Blackburn had recently begun prescribing
vitamin D and taking it themselves - perhaps in part due to an
impromptu video lecture he did while buying fuel for his chainsaw being
widely circulated on Facebook.
http://www.drdavidgrimes.com/2020/06/covid-19-vitamin-d-progress.html
He also writes that the deaths of (mainly BAME) doctors in the UK is
slowing and that this was due in large part to vitamin D awareness
being spread by social media and local newspapers.
A 2020-04-19 article in the BMJ
Is ethnicity linked to incidence or outcomes of covid-19?
https://www.bmj.com/content/369/bmj.m1548 briefly mentioned vitamin D. Most of the 24 (2020-06-15)
responses concerned vitamin D.
The response from veteran vitamin D researcher William B. Grant
mentions, among many other things, that winter 25OHD levels were
15.2ng/ml for vegans and 25.2 for meat eaters, which he attributed to
meat containing both vitamin D3 and 25OHD. Leslie Lewis
mentions 1999
research
into South Asian ethnicity and polymorphisms in the ACE (not ACE2)
enzyme. Robert A. Brown and numerous colleagues from the
McCarrison Society wrote at length about vitamin D.
Pep-talk for doctors regarding the need for robust vitamin D supplementation to protect against severe COVID-19 symptoms
DOCTORS!!!! What is it about vitamin D deficiency that you just don't see, or accept in some fatalistic manner?
The page you are reading and the
icu/ page link to
plenty of research showing the need for proper - 40 to 60ng/ml (100 to
150nmol/L) 25OHD levels to prevent the weakened and dysregulated immune
response which is harming and killing millions of people due to
COVID-19 - and has been doing so for decades at a slower rate with
numerous other acute diseases and chronic conditions.
What is it about vitamin D toxicity (link) which makes you so wary of recommending robust supplementation of 4000IU and more for adults to achieve these levels?
If this catastrophic level of harm and death to your
patients doesn't prompt you do do this, and the harm and death to your
colleagues
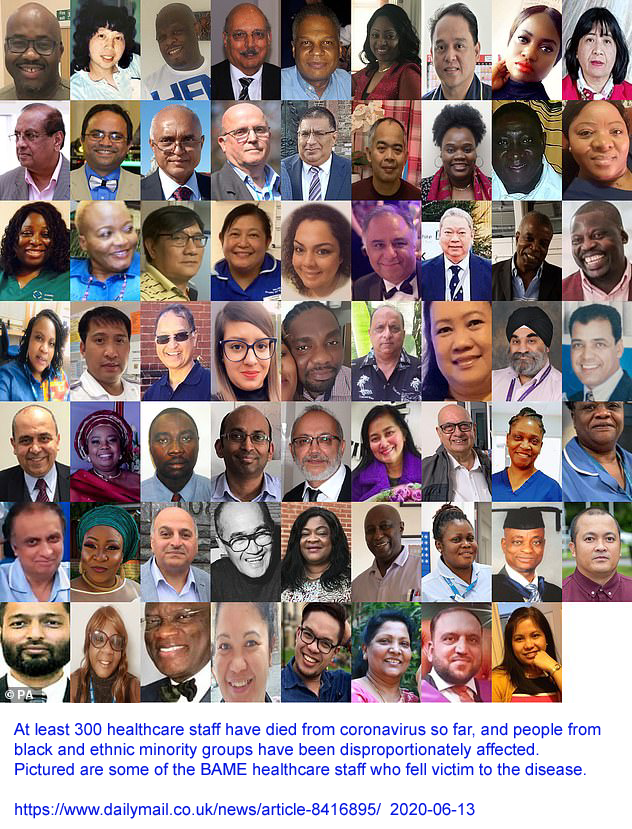
doesn't prompt you to do this, what will?
Doctors are subject to enormous pressures to
conform, not to make wild claims, not to do anything which might cause
harm. Your ability to practice your profession requires you not
to do anything which might make people think of you in terms of the
sound made by ducks.
Non-doctors all around the world are figuring out the need for robust
vitamin D supplementation - sometimes with the help of doctors who
recognise the need for this. I am an electronic technician in
Australia. As far as I know, I have never seen a person infected
with SARS-CoV-2.
Since March
it
was obvious to me that vitamin D deficiency was driving much of the
harm and death from COVID-19. Before I established
these web pages on 2020-03-22 I wrote to numerous doctors and other
responsible people about this. The first version of the email
went to the WHO
Strategic and Technical Advisory Group for Infectious Hazards (STAG-IH) :
Since I figured out the urgent need for a global program of vitamin D
supplementation program in March this year, when the Wordometer looked
like this (2020-03-17):
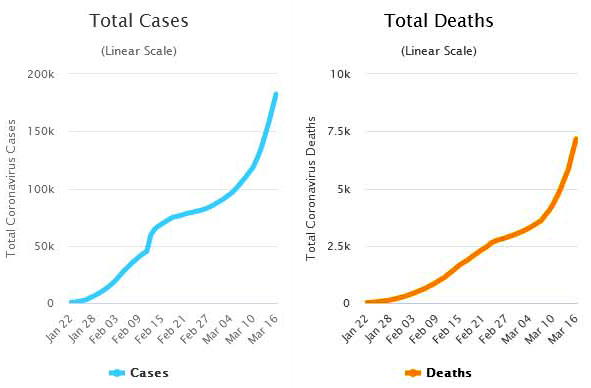
I expect everyone else to have figured it out by now (13.5 weeks later 2020-06-13):
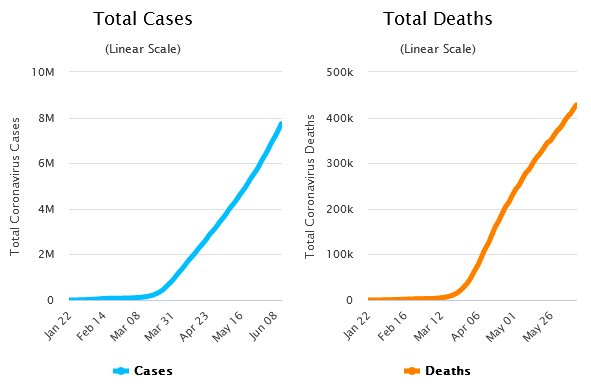
with 120,000 new confirmed cases and 4000 deaths a day.
Remember, the ex-factory cost of pharmaceutical grade vitamin D3, in
1kg lots, is USD$2.50 a gram. At this rate, 4000IU a day costs
USD$0.09 a year. If all adults in the world took this, there would
be little serious harm or death from COVID-19, or influenza and a great
reduction in numerous chronic diseases. Some people, especially
those overweight, need twice this (see the next section).
We don't need blood tests, doctors consultations, double-blind placebo
controlled randomized clinical trials etc. etc. We need a program
to get everyone's vitamin D levels safely above 40ng/ml, ideally within
weeks - but it will take months with all the best efforts and full
support of most doctors and governments. It won't work for
everyone, since it will be voluntary, but it will help most people
escape harm from the COVID-19 infections they are bound to get in the
months to come. Fortunately, for the northern hemisphere, it will
be summer.
Dr David Grimes, from Blackburn, north of Bury, reports (2020-06-07)
http://www.drdavidgrimes.com/2020/06/covid-19-vitamin-d-progress.html
that many BAME doctors are prescribing and taking vitamin D, and that
the death rate among BAME healthcare workers is declining, at least in
his area.
#2020-Baker-a
Articles concerning vitamin D supplementation to protect against harm and death from COVID-19
You can see the vitamin D supplementation naysayers (who want RCT
trials of COVID-19 patients before they would recommend supplements,
though a few say it would do little harm) debating with doctors and
nurses who recognise how important it is to supplement vitamin D, in
the comments to this article:
Dr
Manson, who has lead vitamin D supplementation research, proposes
further work on the value of vitamin D supplementation in anticipation
of COVID-19 infection.
I found two interesting comments: Dr Robert Baker of New Jersey
https://robertbakermdhealthnewsletter.blogspot.com
wrote (my boldface), on 2020-05-14:
I have
tested
over 12,000 patients for a vitamin D level since 2004. A number
of
patients told me when tested that they take 1000 or 2000IU a day of
vitamin D. In spite of that almost all of those people come back
with
a result in the 20's. Seldom over 30ng/ml.
Most adults need
5000 units a day to reach a level of 40 to 50 ng. Some actually
need
double that. The only way to tell for sure is to test at 6
months and
yearly. It would be a waste to do a study that is only going to
raise
the level to high 20's or 30's.
How does
one get
someone to fund an RCT to document what so many clinicians have
observed in the field for decades? The correlation of dramatically
reduced incidence and severity of respiratory infections in
hundreds of
thousands of patients who replete
serum vitamin D levels to 50ng/ml or more is
not ‘anecdotal.’ It’s reams of unpublished potential case studies that
could save lives.
Studies on the effects of vitamin D on various forms
of immunity are probably being designed right now with the same
pathetically insufficient doses to support healthy immune system
function. Such a waste. Mostly over misplaced
fear of Hypercalcemia.
Most average weight patients would need to take 10,000 IU daily for a
year to begin to see a rise in serum calcium levels.
Benefit - Risk Assessment of Vitamin D Supplementation
Heike A. Bischoff-Ferrari1 et al. Osteoporosis Int. 2010 July ; 21(7):
1121–1132
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3062161/
|
Mike Vidler wrote:
80 yr old British born; user for 25 years, southern USA. No degenerative illnesses. NO infections in 20 yr.
Prepared to accept the consequences of my decision whatever they may be!)..
Typical dose 10,000 IU. (10 years)Typical 25(OH)d 70 mg/dL (175 nMol/L)
|
2400IU (0.06mg) a day D3 raises the 25OHD levels of most, but not
all, white women in the USA above 30ng/ml - but few have their levels
raised to the 40 to 60ng/ml range required for optimum health
Here
is my adaptation of one of the charts. Each circle represents the
vitamin D level of one woman in one of the five study groups after 12
months. The first study group received no vitamin D supplements,
so their vitamin D levels result only from sun exposure and the small
amounts of vitamin D in food, with some foods containing small
supplemental levels.
This chart shows the levels of the white women studied. African
American women, without supplementation, had still lower levels: on
average 11.6ng/ml.
Doctors advising vitamin D supplementation in sufficient quantities
to raise 25OHD to 40 to 60ng/ml, which they regard as being vitamin D
replete
Since 2008, with the Scientists' Call to D*Action
link, doctors and researchers have been advocating 40 to 60ng/ml as the healthy standard for vitamin D 25OHD levels.
While they may be in the minority, there are doctors all over
the world, who - like Robert Baker
#2020-Baker-a - recommend high enough D3 intakes
that their patients will be vitamin D replete:
Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza
and COVID-19 Infections and Deaths
William B. Grant
et al. Nutrients 2020, 12(4), 988
https://www.mdpi.com/2072-6643/12/4/988
|
It is
recommended that people at risk of influenza and/or COVID-19 consider
taking 10,000 IU/d [0.25mg a day] of vitamin D3 for a few weeks to
rapidly raise 25(OH)D concentrations, followed by 5000 IU/d [0.125mg per day]. The goal should be to
raise 25(OH)D concentrations above 40 to 60 ng/mL (100–150 nmol/L).
|
I had back surgery in October 2019 and my Dr. recommended to start taking D3 4000IU
[0.1mg] every day + vit. E 1000 to help absorbed D3, I had the surgery and I
was walking the same day. I also had COVID-19 in February and I didn’t
know I had it until I recovered and no fever ever I was just very tired for 1 1/2 week. I‘m 76 yrs. Old and doing great!
|
This article has a good review of "high
dose" (compared to recommendations such as 2000IU a day) vitamin D
supplementation, including with oral and intramuscular 25OHD
(calcifideol). A 6 month trial with relapsing-remitting multiple
sclerosis patients, of 800IU and 10,400IU D3 (cholecalciferol) per day:
. . . achieved 25OHD levels between 40 and 60ng/ml, which was considered the optimal target for patients with MS.
In addition, only in the high-dose group, there was a reduction in the
proportion of IL17+ CD4+ T cells, considered a major contributor to the
immunopathogenesis of MS, with a concomitant increase in the proportion
of central memory CD4+ T cells and naıve CD4+ T cells, concluding that
high-dose cholecalciferol therapy exhibits in vivo pleiotropic
immunomodulatory effects in MS. Adverse events were minor and did not
differ between the two groups, indicating that 10,400 IU
cholecalciferol daily is a safe and well-tolerated therapy in patients
with MS. [0.2mg].
A Brazilian pilot study by Finamor et al. on the efficacy and safety of prolonged high-dose vitamin D3 therapy in patients with psoriasis and vitiligo suggested that an oral daily dose of 35,000 IU
[0.875mg] D3 for 6 months, associated with preventive measures (low-calcium diet
and a daily hydration of at least 2.5 L daily), is a safe and effective
therapeutic strategy for reducing disease activity. All nine patients
with psoriasis and 14 out of 16 with vitiligo recruited in the study
received benefit from the treatment, showing a decreased disease
activity with no side effects. Altogether these studies indicate that
25OHD blood levels below 100ng/mL are safe.
Nevertheless, there are groups of individuals in which high doses of
vitamin D over a long period could be detrimental in terms of
developing hypercalcemia and rapid deterioration of kidney function,
such as patients with primitive hyperparathyroidism or those with
chronic granulomatous diseases, which are prone to elevated extrarenal
synthesis of 1,25OHD. Moreover, even healthy subjects with
mutations in CYP24A1 - the mitochondrial enzyme responsible for the
deactivation of 1,25OHD - are susceptible to developing hypercalcemia,
hypercalciuria, and kidney stones when exposed to high vitamin D
doses.
Therefore, to avoid toxicity, all patients eligible for a high-dose
treatment should be previously screened for hypercalcemia and
hypercalciuria, while serum and urinary calcium levels should be
monitored during the vitamin D treatment itself.
To date, it can be established that vitamin D dose up to 2000 IU/day, or more recently, 4000 IU/day [0.1mg] should be considered safe above the age of 9. This dose should be corrected according to non-pharmacological intake of the vitamin D.
|
The question of potential vitamin
toxicity for particular groups of people is a frequent argument for
limiting supplement does for all people. I plan to research this
assiduously when writing the forthcoming website, using the best
available research on vitamin D toxicity such as
this
. I have an article here somewhere arguing that patients with
granulomatous diseases do better with higher doses of vitamin D.
(These are immune system disorders in which the troops fuss and fight,
mistake each other for the enemy, and bind to each other in numerous
small clumps throughout the body. Some immune cells in these
clumps have been observed to convert 25OHD into 1,25OHD in such
quantities perhaps due to intracellular bacterial infection - that it diffuses into the bloodstream,
potentially disturbing calcium metabolism.)
Massimiliano Caprio and colleagues cite several lines of research
indicating the need for 40ng/ml or more 25OHD to avoid various
illnesses:
Editorial – Vitamin D status: a key modulator of innate immunity and natural defense from acute viral respiratory infections
A. Fabbri, M. Infante, C. Ricordi Eur Rev Med Pharmacol Sci 2020; 24 (7): 4048-4052 2020-04-05
https://www.europeanreview.org/article/20876
|
They mention that 40 to 60ng/ml circulating 25OHD is required for the autocrine signaling system of immune cells to function properly.
25OHD in the bloodstream (from food, supplements or UVB-irradiated
skin), for instance at a concentration by mass of 1 part in 25 million
(40ng/ml) diffuses into the cytoplasm of the cell where it is the input
(substrate) molecule for the CYP27B1 enzyme which converts it to
1,25OHD, which immediately complexes with vitamin D receptor
molecules. The complexes then migrate to the nucleus find a
promoter molecule bonded to DNA near the start of a gene, and there
activate the process of transcribing that gene into an RNA molecule
containing the gene's instructions.
That messenger RNA molecule - or rather multiple such molecules
produced by this transcription mechanism - goes into the cytoplasm were
ribosomes work along it, using its instructions to build a molecule of
protein from the specified amino acids.
The enzyme and receptor genes are both upregulated by a process driven
by external conditions according to the cell type. Likewise, the
one or more genes upregulated (and some can be downregulated) by the
1,25)HD-vitamin-D-receptor complex vary according to cell type.
With blood concentrations of 40 to 60ng/ml
or above, the rate of 1,25OHD synthesis becomes "substrate independent"
- that is, the enzyme does not spend long waiting for another 25OHD
molecule to fall into its active site for conversion. Below this
concentration, it takes longer, on average, for a new 25OHD molecule to
engage, so this lowers the enzyme molecule's output of 1,25OHD and so
limits this entire autocrine signaling pathway, reducing the cell's
ability to respond as it should to all its conditions. In the
case of various types of immune system cell, this leads to both
weakness in direct responses to the infection, and also to weak
regulatory actions, which are intended to release anti-inflammatory
cytokines and so reduce overly aggressive, self-destructive,
hyper=inflammatory actions (AKA cytokine storm) by other immune cells.
So it is not surprising that low 25OHD levels make it more likely that
SARS-CoV-2 will progress to the lungs, and once there, trigger an
overly-aggressive, destructive, hyper-inflammatory cytokine
storm. This leads to destruction of endothelial cells lining the
blood vessels and so to hyper-coagulatory blood which causes micro
embolisms all over the body.
We also believe that maintenance of circulating 25-hydroxyvitamin D levels of 40 - 60ng/ml would be optimal, since it has been suggested that concentrations amounting to 40ng/ml represent the beginning point of the plateau where the synthesis of the active form calcitriol becomes substrate-independent [2011-Hollis err] [2018-Wagner].
Additionally, serum 25-hydroxyvitamin D levels of approximately greater than or equal to 40ng/ml
could provide protection against acute viral respiratory infections, as
demonstrated in a prospective cohort study published in PLoS One and
conducted on 198 healthy adults [2020-Sabetta]. To reach these concentrations in adults, a dietary and/or supplemental intake of vitamin D up to 6000 IU/day
– deemed to be safe – is required. However, elderly subjects,
overweight/obese and diabetic patients, patients with malabsorption
syndromes, and patients on medications affecting vitamin D metabolism may require even higher doses under medical supervision.
|
Dr David Ajibade of the Nigerian based Brain and Body Foundation (
bio) stated, on 2020-07-25 in an
interview :
In
my opinion, the best way for black people to get adequate levels of
vitamin D is by supplementation. And the research shows that adults
should be getting no less than 10,000 IUs a day. (0.25mg a day.)
In my opinion, the best
way for black people to get adequate levels of vitamin D is by
supplementation. And the research shows that adults should be getting no
less than 10,000 IUs a day.
Read more at:
https://www.vanguardngr.com/2020/07/vitamin-d-crucial-in-management-of-covid-19-sickle-cell-disorders-dr-david-ajibade/
In my opinion, the best
way for black people to get adequate levels of vitamin D is by
supplementation. And the research shows that adults should be getting no
less than 10,000 IUs a day. Read more at:
https://www.vanguardngr.com/2020/07/vitamin-d-crucial-in-management-of-covid-19-sickle-cell-disorders-dr-david-ajibade/
In my opinion, the best
way for black people to get adequate levels of vitamin D is by
supplementation. And the research shows that adults should be getting no
less than 10,000 IUs a day.
Read more at:
https://www.vanguardngr.com/2020/07/vitamin-d-crucial-in-management-of-covid-19-sickle-cell-disorders-dr-david-ajibade/
|
#Maharashtra-police
Indian Police receive substantial vitamin D supplementation
Here is an example of the action
governments and particular organisations and companies can take in this
time of crisis to make a real difference to people's health through
nutrition:
 https://www.expresspharma.in/....vitamin-d3-dv-60k-for-250000-maharashtra-police-personnel/
https://www.expresspharma.in/....vitamin-d3-dv-60k-for-250000-maharashtra-police-personnel/
Fermenta Biotech is one of the biggest producers of vitamin D3
cholecalciferol for both pharmaceutical use and for agricultural
feed. They have cholecalciferol factories in Kullu and Dahej:

Fermenta Biotech and Indchemie Health Specialities have jointly
committed to supplying Maharashtra Police personnel 250,000 strips of DV
60K, each strip containing sufficient dosage for an individual’s
recommended regime of 60,000 IU of Vitamin D3 per week for two months.
|
The state of Maharashtra includes Mumbai and has a population of 112
million people. Its 250,000 personnel will use these oil-filled
minicaps once a week to provide 8571IU (214ug) vitamin D3 per day.
Other articles not yet mentioned
I don't have time to report in detail
on a number of vitamin D COVID-19 articles. Here are the
URLs. I hope to return to these at a later date, probably on the
new website, since this page is getting very long:
#low-verylow
Irish doctors debate whether to use low or ridiculously low doses of vitamin D3
You may be interested to read Irish doctors debating how much supplemental vitamin D3
should be given, with one group (and these are the good guys) arguing
for
2500IU (62.5ug) a day - which, above, Robert Baker wrote was nowhere near
enough - and the other group arguing for
800IU (20ug) or so a day, which
is 10% to 20% of what people actually need. These are two of
several articles in a Vitamin D Debate section of the May 2020 edition (
index):
They are concerned about supplements of 2000IU (50ug) being "high".
They were responding to an article by McCartney et al,
here,
citing the Filipino work (
#2020-Alipio) I now regard as fake, with suggestions of up
to 2500IU/day.
Likewise a doctor who cites the Philippino and Indonesian research
mentioned above, and who for some reason thinks that 600IU/day D3 is
sufficient: (
link)
until RCTs demonstrate that more is needed for COVID-19 patients.
The central mystery for me, in all this, is not what is happening in
COVID-19 patients, or in people who are suffering from a wide range of
diseases, nor in how these tragic, disastrous, patterns of ill-health
can be largely resolved by supplementation. The
central mystery, which I am slowly coming to elucidate, is why many
doctors (at least in the West - and I haven't seen such a trend in
nurses) are so ignorant and/or unreasonably wary of nutritional
supplements in general and of vitamin D in particular.
I will write up my thoughts some other time, but for now, I regard many doctors'
extreme reluctance to advise robust, safe, doses of vitamin D3 is
contributing to the immense toll of harm and death due to immune system dysfunction.
21 authors advise very low levels of D3 supplementation, aiming for a minimum 25OHD level of only 10ng/ml
Meanwhile 21 authors, in an article
finalised on 2020-04-29, support the official UK guidance on vitamin D
intakes, cautioning strongly against exceeding 4000IU/day on account of
unspecified dangers (though kidney disease was mentioned in passing):
They advocate daily, midday sunshine as an important part of
maintaining vitamin D levels - despite the sun not always shining and
not being at a high enough angle in the sky to be useful, even if
direct sunlight can be found in dense urban environments in which many
people are confined due to shelter at home laws. There's no
mention of skin area to be exposed, but their "season appropriate
clothing" description implies scarves and gloves, with little skin to
be exposed, in winter.
They explicitly support the official recommendations for 400IU/day D3
(UK) and 600IU/day (USA and for >70 yo Europeans). They note
that the UK standards are intended to ensure the majority of the
population have 25OHD levels above
10ng/ml (UK) or
12 to
20ng/ml
(USA). There is no reference to hunter-gatherer levels of
46ng/ml (
https://www.ncbi.nlm.nih.gov/pubmed/22264449), or to the severe vitamin D deficiency observed in, and
obviously causing (in combination with some infectious insult) Kawasaki
Disease (
#2015-Stagi above) were sufferers averaged 9.2ng/ml.
Historical note:
I initially complained here "Nor is there any mention of the work of #2020-Alipio (3 weeks before their final version) and #2020-Raharusun (a day after) showing much greater risk of serious COVID-19 symptoms and death with 25OHD levels below 30ng/ml." but in late June I recognised these to be fake, so these Susan Lanham-New et al, were right not to cite these.
21 highly qualified people went to some trouble to write an article
which gave people completely false assurances about the desirability of
such low levels of vitamin D supplementation and 25OHD levels, whilst
warning strongly against dosages which are actually, as mentioned
above, at the low end of what is necessary to achieve vitamin D
repleteness regarding immune system functioning.
I regard
work such as this as a fundamental part of the problem we are trying to
solve - and that it directly contributes to the suffering, harm and
death caused by dysregulated immune system responses to SARS-CoV-2.
I wrote a comment to this article on 2020-05-20.
Despite assurances via email that the were attending to this, no
comments have been published. Meanwhile, the article has been
widely reported in the press along the lines of experts advising that
there is no reason to believe that vitamin D supplementation will help
with COVID-19 symptoms - while suggesting that their low doses should
be taken anyway, with an absolute upper limit of 4000IU/day.
COVID-19 pathology - weak and dysregulated immune systems
On the ICU page
icu/ please see these items:
Firstly,
Farid Jalali's beautiful detective work icu/#2020-Jalali-b
- an etiological hypothesis of COVID-19 lung injury, which explains may
observations which are unique to this disease. One of is diagrams:
Secondly a link icu/#2020-Kim
to a recent article Vitamin D and Endothelial Function which shows how
important vitamin D is for enabling endothelial cells to vasodilate
(and COVID-19 makes them vasoconstrict) and to resist inflammation.
If you are are a researcher or doctor - or if you still doubt how
essential it is to make everyone vitamin D replete - please see the icu/ page for more detailed descriptions of COVID-19 lung and pathology and the role vitamin D deficiency plays in this.
Please see the ICU page
icu/#2020-Tay
for a link to an article which makes it clear how much severe COVID-19
symptoms are a result of weakened and dysregulated, overly-aggressive,
proinflammatory immune responses. A diagram from the article:
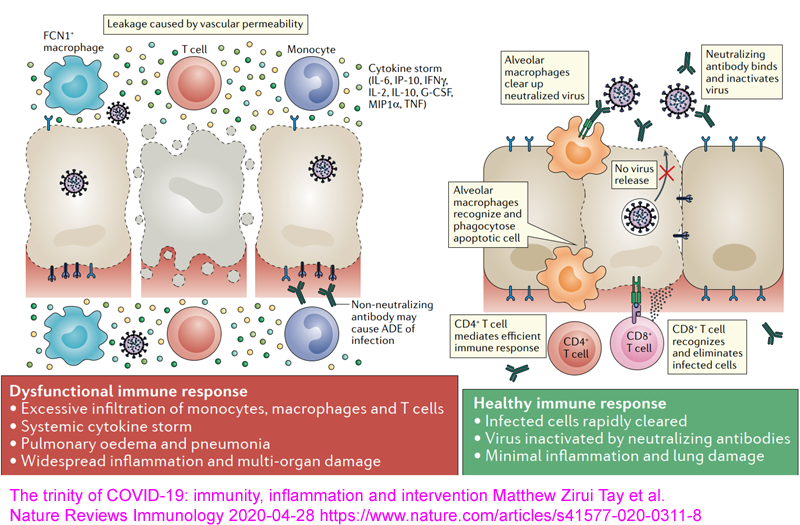
#helminthsgone
Weak and dysregulated, over-inflammatory, immune responses are
caused by lack of helminths, individual genetic variation, dietary
excesses and several common nutritional deficiencies
This
is my account of this important question. I haven't read it like
this in any one academic article, but I cite such articles which
support the various parts of my explanation.
The material below was written in 2020. Please see this section
of a page on my newerr websties for more information on helminths and
the immune system, including an article which reports that Ethiopians
with active helmith infections had a 77% lower chance of severe
symptoms, and a very much reduced risk (to zero, in the infected
people) of death:
The primary reason
for the immune dysregulation which makes COVID-19 potentially harmful
and deadly is that our immune systems evolved to be overly-aggressive
due to the presence of intestinal worm (helminth) infestations which
downregulated many aspects of our immune response. Now - in
developed countries - without such helminths, our immune system is
overly-aggressive in several important ways, which contributes
enormously to a plethora of acute and chronic inflammatory and
autoimmune diseases, including asthma, MS (multiple sclerosis),
inflammatory bowel disease, osteoporosis etc. etc.
Low vitamin D makes this much worse, due to it reducing the ability of regulatory immune cells to limit inflammation /icu/#2020-McGregor
- likewise inadequate omega-3 fatty acids, magnesium and probably
boron. However, even with perfect nutrition, we would still
generally have a problem with some of our inflammatory responses, such
as those from eosinophils [WP], being overly aggressive and so self destructive.
The degree to which this is a problem in any one person depends on
their genetics, with a wide variation in the strength of these
responses apparently being partly hereditary. Developmental
differences would also be important, and of course some or many
autoimmune disorders occur after some triggering event, such as a viral
or bacterial infection, or pollen, particular foods etc.
Eosinophils are the suicide bombers of the immune system. When
they are activated and so disintegrate, they release chemicals which
destroy all cells - ideally those of multicellular parasites such as
helminths, but also our own cells.
Helminths evolved ways of downmodulating some of our immune responses,
such as eosinophilic inflammation (cell destruction). Our
ancestors evolved stronger responses. Now the helminths are gone
we are left with the generally, or at least frequently, overly strong
inflammatory responses.
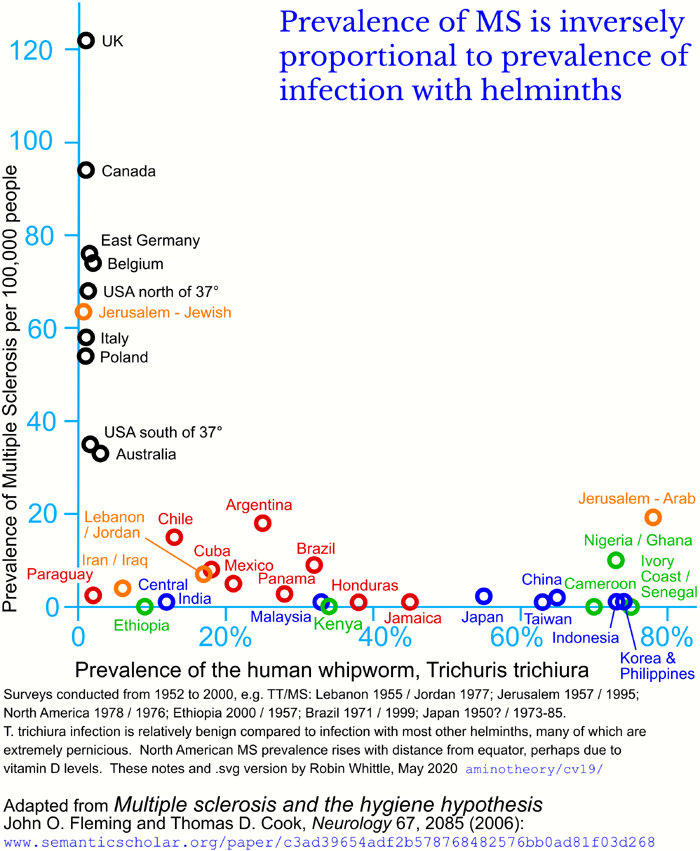
(The Inkscape .svg file of the above chart his
here.)
Low vitamin D levels also drive the incidence of MS. For
instance, hardly anyone in Australia has helminths, but MS is much more
common in Tasmania, far from the equator, than in sub-tropical and
tropical Queensland.
Some information on helminth infection prevalence by country and within countries is available at
http://www.thiswormyworld.org/maps/find-a-map and
PMC6114701 .
It would not be surprising if people with such infections
had less trouble with COVID-19 than those in developed nations where we
got rid of helminths decades ago. However, many of these people
suffer numerous health problems and have little access to hospital
care. They may also be deficient in vitamin D, boron and other
nutrients, so this is not a cause for complacency or even much
hope.
#Ethiopia
That said, please consider these two items concerning Ethiopia:
51% prevalence of helminths. I haven't scrutinised the article,
but it is clear from many other articles that helminths are more
prevalent in Ethiopia than in most other countries. Also, this advice for travelers (
iamat.org) states
Risk is present in urban and rural areas of Ethiopia. Fleming
et al. state that since school age children are the most likely hosts,
and that
infection in childhood may provide protection from MS for
life, so that relatively low (such as for most children being infected at
some stage, rather than the whole population all the time) levels of helminth
infection may provide good protection for most of the population.
Numerous factors are discussed which
might explain the low rate of spread and severity in Ethiopia.
Vitamin D is mentioned briefly, but not helminths.
We cannot easily fix the overly-aggressive immune systems we inherited. Helminthic therapy
https://helminthictherapywiki.org
is sometimes used for severe asthma, Crohn's disease etc. There
is a lot of research into compounds which replicate of mimic the
downregulating chemicals helminths exude. More on this below.
One dramatic demonstration of the importance of this evolutionary
overshoot to inflammatory diseases is that Crohn's disease patients
went into remission when infected with the relatively benign pig
whipworm:
There is, of course, considerable
genetic variation
between individuals. For instance, sensitivity to Crohn's disease
has a strong genetic component. Yet pig whipworm infection causes
many Crohn's sufferers to go into remission.
The
second set of reasons
for
this immune system dysregulation is
nutritional deficiencies - and
dietary excesses, such of salt and some fats. These weaken
many initial immune responses and are an additional cause of
dysregulation which drives overly-aggressive inflammatory responses,
which harm the self while failing to destroy the virus, bacteria or
whatever it is which is causing the infection.
These nutritional deficiencies can be fixed - and fixing them for most humans is the only way we
can coexist with COVID-19 without further disastrous harm and death
and without the need for the disastrously harmful and deadly lockdowns.
In 2018 and 2019
helminth researchers made
important progress. They identified one particular compound which
helminths produce which down-modulates our inflammatory immune
responses. The compound can be manufactured in the lab and is
being used in a number of non-human animal studies.
The compound is
Tuftsin-PhosphorylCholine (TPC) and the lead researcher in this field is Prof Miri Blank, currently working in Israel:
https://autoimmunity2018.kenes.com/2018/scientific-information/aesku-award.html .
Here are three pertinent articles:
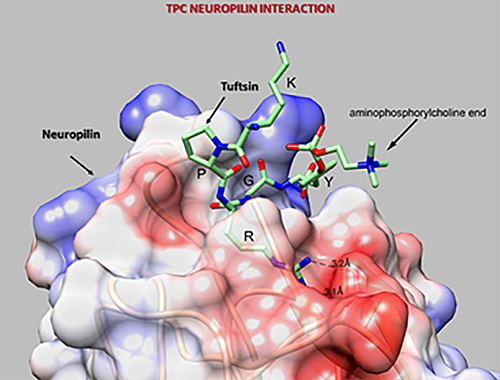
This is from:
Helminths-based bi-functional molecule, tuftsin-phosphorylcholine (TPC), ameliorates an established murine arthritis
Miri Blank, Tomer Bashi, Jordan Lachnish, Dana Ben-Ami-Shor, Ora
Shovman, Mati Fridkin, Miriam Eisenstein, Alexander Volkov, Iris
Barshack and Yehuda Shoenfeld.
PLoS One 2018-08-08
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0200615
|
Helminth-Based Product and the Microbiome of Mice with Lupus
Hadar Neuman, Hadar Mor, Tomer Bashi, Or Givol, Abdulla Watad, Asaf
Shemer, Alexander Volkov, Iris Barshack, Mati Fridkin, Miri Blank,
Yehuda Shoenfeld and Omry Koren
American Society for Microbiology mSystems 2019-02-19
https://msystems.asm.org/content/4/1/e00160-18
|
These autoimmune researchers are making
bold progress on the most profound problems - but I get the impression
they are not paying much attention to vitamin D deficiency.
Some or many vitamin D researchers and clinicians are very interested
in autoimmune conditions, but I think they should do more to keep up
with this fundamental research into helminths and their inflammation
downmodulating mechanisms. Now that one of the presumably
multiple signaling molecules are identified, there would be arguments
for using them in humans to at least partially replicate the helminths'
anti-inflammatory effects.
Two articles concerning higher levels than normal of D3 supplementation
and circulating 25OHD, and how these are able to suppress autoimmune
conditions such as psoriasis, are from Patrick McCullough and
colleagues in Cincinnati Ohio.
The vast majority of 4700 adult patients admitted over 7 years to
a modern 291 bed Cincinnati psychiatric
hospital
specializing in addiction and behavioural problems agreed to
vitamin D supplementation and monitoring. D3 supplemental intake
was typically 0.125mg 5000 IU to 0.250mg 10,000 IU per day, with
some patients reducing their psoriasis with daily intakes of
20,000 and 50,000 IU a day.
We found intakes of 20,000 IU/d to 60,000
IU/d, associated with 25OHD blood levels ranging as high as
384 mg/dl, safe when taken on an extended daily basis. Many of
the 25OHD blood levels we have observed are much higher than
the currently defined upper limit of normal of 100 ng/ml, yet we found no evidence of toxicity in any
individual who achieved these blood levels after taking these
doses for extended periods of time.
Two of the authors had safe,
beneficial, experiences with intakes which would generally be
considered dangerous:
The decision to
treat our psoriasis patients with vitamin D was made due to
the multiple reports cited earlier showing its clinical
efficacy and safety [14,54–59]. This includes the previous
success of one of the authors (PM) in treating psoriasis using
oral vitamin D3 in doses ranging up to 40,000 IU/d [57]. We
were also confident that the doses we used would be safe and
effective due to the recent experience of two of the authors
(JA, PM) in safely using comparable doses of vitamin D in
treating asthma and skin cancer.
This is a recent preprint. Expect updates, at least for some typos.
Oral and
Topical Vitamin D, Sunshine, and UVB Phototherapy Safely
Control Psoriasis in Patients with Normal Pretreatment Serum
25-hydroxyvitamin D Concentrations: A Literature Review and
Discussion of Health Implications
Patrick J McCullough, William McCullough, Douglas
Lehrer, Jeffrey Travers and Steven Repas.
Preprint 2021-03-02
https://www.preprints.org/manuscript/202103.0061/v1
|
#vaccines
COVID-19 vaccines and immunity - robust vitamin D supplementation will be far superior to even the most perfect vaccine
Studies
of patients who became infected with SARS-CoV in 2003 suggested that
the infection induced durable T cell responses lasting for 6 years but
no long-term memory B cells. Importantly, these T cells were
shown to cross-react with the SARS-CoV-2 virus 17 years later, but the
extent to which they can provide protection is not known.
In my opinion, the best
way for black people to get adequate levels of vitamin D is by
supplementation. And the research shows that adults should be getting no
less than 10,000 IUs a day. Read more at:
https://www.vanguardngr.com/2020/07/vitamin-d-crucial-in-management-of-covid-19-sickle-cell-disorders-dr-david-ajibade/
In my opinion, the best
way for black people to get adequate levels of vitamin D is by
supplementation. And the research shows that adults should be getting no
less than 10,000 IUs a day.
Read more at:
https://www.vanguardngr.com/2020/07/vitamin-d-crucial-in-management-of-covid-19-sickle-cell-disorders-dr-david-ajibade/
|
This recurrent theme [referring
to vaccines for coronaviruses in cats, other domestic animals,
agricultural animals and species used in vaccine research] of waning immunity and need for periodic boosts following initial infection or vaccination
is relevant to our understanding of human respiratory coronaviruses and
has implications for vaccine strategies against these viruses,
especially SARS-CoV-2, in humans.
In my opinion, the best
way for black people to get adequate levels of vitamin D is by
supplementation. And the research shows that adults should be getting no
less than 10,000 IUs a day. Read more at:
https://www.vanguardngr.com/2020/07/vitamin-d-crucial-in-management-of-covid-19-sickle-cell-disorders-dr-david-ajibade/
In my opinion, the best
way for black people to get adequate levels of vitamin D is by
supplementation. And the research shows that adults should be getting no
less than 10,000 IUs a day.
Read more at:
https://www.vanguardngr.com/2020/07/vitamin-d-crucial-in-management-of-covid-19-sickle-cell-disorders-dr-david-ajibade/
|
The authors discuss mutations which can occur during persistent
infection with a normally mild feline coronavirus which cause it to
infect macrophages in addition to the usual intestinal epithelial
cells. The mutated form - Feline infectious peritonitis virus (
FIPV)
- is universally fatal. Vaccination or prior infection with the
coronavirus can give rise to antibodies which instead of protecting the
cat, enable the virus to infect cells which develop into a particular
type of lymphocyte. (More details
here.) This process of antibodies enabling the virus to infect different types of cell than it normally does is
Antibody-Dependent Enhancement - ADE.
ADE in the context of FIPV vaccination raises concerns about the same phenomenon occurring after SARS-CoV-2 vaccination.
In my opinion, the best
way for black people to get adequate levels of vitamin D is by
supplementation. And the research shows that adults should be getting no
less than 10,000 IUs a day. Read more at:
https://www.vanguardngr.com/2020/07/vitamin-d-crucial-in-management-of-covid-19-sickle-cell-disorders-dr-david-ajibade/
In my opinion, the best
way for black people to get adequate levels of vitamin D is by
supplementation. And the research shows that adults should be getting no
less than 10,000 IUs a day.
Read more at:
https://www.vanguardngr.com/2020/07/vitamin-d-crucial-in-management-of-covid-19-sickle-cell-disorders-dr-david-ajibade/
|
The Wikipedia article on ADE has a
section
on ADE complicating betavirus vaccine development, with examples of
non-human animal research into vaccines for MERS_CoV and SARS-CoV (the
virus which caused the 2003 disease SARS).
A Google Scholar
search for
ADE SARS-CoV-2 returns over a thousand articles. The most highly cited
article
suggests that SARS-CoV-2 infections maybe worsened by ADE from
antibodies raised by previous coronavirus infections - and that is may
be an important reason why particularity populations have worse
outcomes than other populations.
More on ADE:
A widely cited 2014
article
demonstrated ADE in-vitro with dilute neutralising antibodies to
SARS-CoV spike protein. Antibodies from a prior Dengue virus infection
can lead to ADE on a second infection (
Stat 2017) with consequent cytokine storm. A 2020-07-22 Global Virus Network
article on ADE and SARS-CoV-2 links to research articles including
this
one from 2015, in which a monoclonal neutralising antibody attaches to
the MERS (another coronavirus) spike protein, changing its shape.
The antibody then attaches to the Fc receptor [
W]
of lymphocytes and other immune system cells which are intended to
activate phagocytic (pathogen destroying) or cytotoxic (killing
infected cells) actions, but in this case brings the attached virus
into the immune cell, infecting it. The GVN article mentions
interactions with common cold coronaviruses and states:
Epidemiological studies investigating ADE in individuals with multiple
SARS-CoV-2 infections or cross-reactivity to common-cold-causing CoVs
will likely take several years.
In my opinion, the best
way for black people to get adequate levels of vitamin D is by
supplementation. And the research shows that adults should be getting no
less than 10,000 IUs a day. Read more at:
https://www.vanguardngr.com/2020/07/vitamin-d-crucial-in-management-of-covid-19-sickle-cell-disorders-dr-david-ajibade/
In my opinion, the best
way for black people to get adequate levels of vitamin D is by
supplementation. And the research shows that adults should be getting no
less than 10,000 IUs a day.
Read more at:
https://www.vanguardngr.com/2020/07/vitamin-d-crucial-in-management-of-covid-19-sickle-cell-disorders-dr-david-ajibade/
|
Most members of the public, and of governments - and probably quite a
few doctors - have a vision of a vaccine being a safe, well-tested,
highly effective means of creating lasting immunity - akin to a
magic bullet.
However, the safety of any vaccine cannot be known until it has been
used in hundreds of thousands of people, since even rare incidences of
ACE making subsequent SARS-CoV-2 infection much worse are a serious
matter. For more on this, click the aforementioned search link
and see
Out of the frying pan and into the fire? Due diligence warranted for ADE in COVID-19 (2020-06-240
https://www.sciencedirect.com/science/article/pii/S1286457920301246 .
I don't have time to read these articles and I doubt of you do
either. However, if you think that a safe, effective,
vaccine for SARS-CoV-2 can be developed and
tested without
years of work, then you should at least cast your eyes over the
Lessons and
frying pan articles.
Also, some of these COVID-19 vaccines - including the Oxford one the
Australian government is so keen to get - work by injecting an
artificial virus which can infect cells but not reproduce.
The infected cells produce parts of the virus's spike protein, which
together with adjuvants, causes the immune system to recognise these as
other and mount an immune response, just like in a real infection.
How do the virus creators know which cells are going to produce these
fragments? What happens if the vaccine is given to someone who
has already been infected with COVID-19? They may not know it,
and we can't give everyone an antibody test before vaccination to
prevent this. Let's imagine this person having an overly twitchy
immune response - strong immunity from antibodies and/or memory cells
AND genetic differences making them prone to dysregulation AND lousy
vitamin D, boron, omega 3 fatty acid etc. intakes. Why wouldn't
their immune system go bananas with this sudden explosion of spike
proteins and adjuvant and so cause extreme hyper-inflammatory
reactions, including cytokine storm damage to endothelial cells?
This would lead to the same deadly coagulopathy which harms and kills
most or all of the people who are killed by their immune system's
response to a real COVID-19 infection.
Most doctors, ordinary people and governments are operating according to the following "conventional wisdom":
- Infection with SARS-CoV-2 is potentially very harmful or deadly.
- Without a vaccine it can only be stopped with extreme and
unsustainable lockdowns, social distancing etc. or by herd
immunity. (There are numerous arguments that the
early, low-dose use of hydroxychloroquine and some other drugs are
safe, highly protective and inexpensive - and that some government
bodies are unreasonably restricting their use to the advantage of
companies which make vaccines and more expensive drugs. I
tend to agree with this view. I mention it because there is a
growing body of opinion that the early and ICU care of COVID-19
patients could be much better than it is, so rendering the threat posed
by the virus significantly lower than many people believe it
is. I think there is merit in this, but that vitamin D
repletion is a much more powerful, safer and more generally useful
approach than band-aid approaches involving drugs once people are
infected.)
- Herd immunity (something like 70 to 90% or more people being
immune) will stop, or dramatically slow, the spread of the virus, so
even those with no immunity are completely or largely protected.
- Few, if any, governments aim for herd immunity to be achieved via
most of their population being infected, so they have their populations
living in fear, isolation, locked down etc. waiting for a
population-scale vaccination program to achieve herd immunity with
minimal direct infections. This is personally, socially, economically and politically extremely destructive.
Consequently governments and populations alike, are, in general, doing
their civil duty by enforcing and complying with lockdowns etc.
while eagerly awaiting the boffins to develop, test and mass-produce
their magic bullet vaccines, ready for a bevy of hypodermic equipped
nurses to administer to the great majority of the
population. This is reckless and at odds with all we know
about vaccine development and testing, which normally takes many years.
A growing number of people are becoming alarmed and bitterly frustrated
with this mainstream government approach, as supported by most
doctors. There are numerous websites devoted to this.
Tucker Carlson's 2020-08-24
video When do we get America back?
encapsulates quite a bit of this frustration which I think is well
founded and doesn't depend at all on avoidant themes such as the virus
being a hoax. I would really like to bring him and numerous other
influential people up to speed on nutrition for immune system health!
Let's imagine the best case outcome for COVID-19 vaccination:
- A vaccine is available next week, in sufficient quantities to supply the country's entire population.
- The government has convinced (or perhaps will force) most or all of the people to accept vaccination.
- The doctors and nurses are ready to go, including to all corners
of the country - bearing in mind that some of these vaccines involve
two separate injections spaced two weeks apart.
- Although it is impossible to establish, beyond reasonable doubt,
that the vaccine is safe (zero or exceedingly low incidence of serious
ill effects, including especially ADE),
for the purposes of this discussion let's assume that it actually is
100% safe AND highly, perhaps, 100% effective AND produces very low
levels of normal effects, such as headache, GI problems, being unable
to work for a few days etc.
- The financial cost of the vaccine is zero. So to, by some
magical means, is the cost of deploying all these medical personnel,
and the administrative and logistical support for them.
Even with these ideal conditions, vaccination against COVID-19 is absolutely the wrong approach.
It is an attempt to solve the wrong problem.
The problem is not the virus.
The problem is that many people's immune systems are weak and dysregulated.
There are three sets of reasons for this, considering a whole population of individuals:
- Humans now, with rare exception, are no longer infested with
helminths (intestinal worms), which in our ancestors downmodulated
several immune responses. Our immune systems evolved with
helminths and so some aspects of our systems' operation are
dysregulated: overly aggressive, hyper-inflammatory and so (without
helminths downmodulating these responses) cause the cytokine storm
which is a crucial step in the development of severe COVID-19.
See #helminthsgone . (Lack of helminths lead to dysregulation, not immune system weakness.)
We can't easily fix this, since helminths are at least somewhat pernicious and many are extremely harmful.
- Individual genetic variations on the average human genetic
pattern which cause some people to have weaker and/or more dysregulated
immune responses than average.
Again, we can't fix this.
- Nutritional deficiencies and some excesses (such as salt,
high-fructose corn syrup, excessive omega 6 and trans fatty
acids). We can and must fix these since the health benefits
vastly exceed the costs of doing so.
The most important and best researched deficient nutrient is vitamin
D. Only tiny quantities, at very low cost, are required to
bring everyone's 25OHD levels safely into the 40 to 60ng/ml range. See #kp above and #plan below for details of the other deficient nutrients.
A country-wide, ideally global, program of vitamin D repletion will be
much easier, less expensive and safer than any vaccine
program. Although it will take some months to build new
vitamin D3 factories to produce the quantities we need, these
quantities and costs are very small compared to vaccines. An
average weight person needs 1/22 of a gram D3 per year - and it costs
about USD$2.50 a gram.
The same principle applies to influenza vaccines: influenza only causes
serious harm to people with weakened and dysregulated immune
systems. This weakness and dysregulation has several
contributing causes, but in most people it can be largely or completely
overcome with vitamin D supplementation to achieve 25OHD levels of
40 to 60ng/ml.
#cannell
There is well-known seasonality driving influenza and common cold respiratory infections:
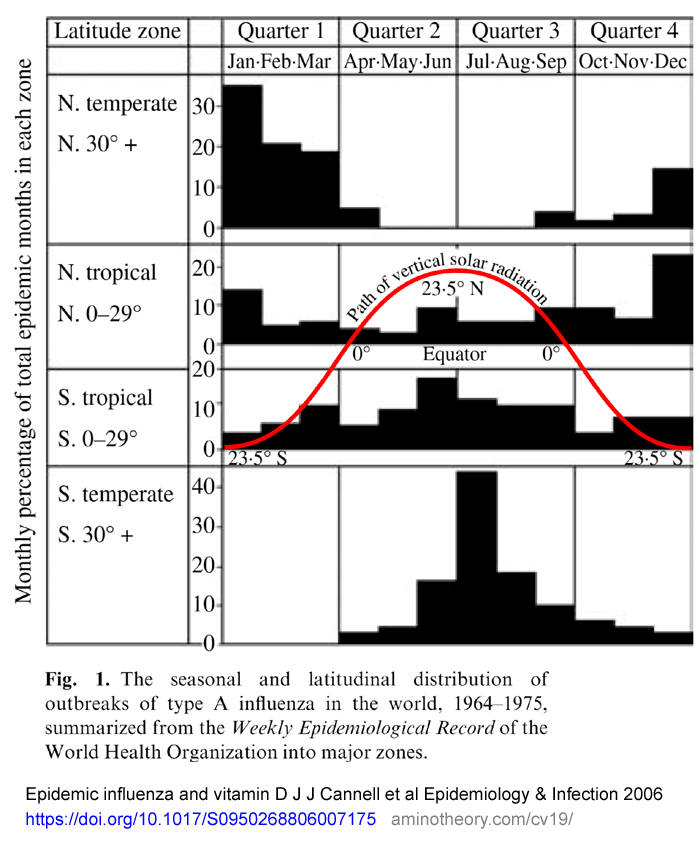
This is from:
* Member of the
NISH discussion mailing list.
The next chart is from correspondence regarding the above article:
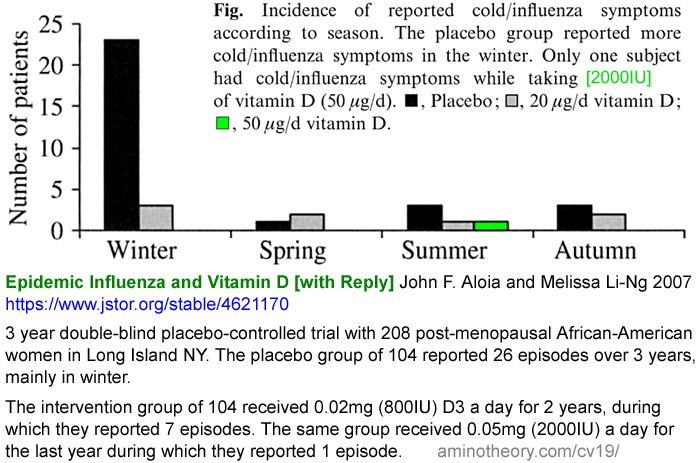
The seasonality of the spread of influenza - and no-doubt COVID-19 -
can be explained in terms of two potentially variable items, assuming
the population mixes and behaves reasonably consistently throughout the
year. (For simplicity I am ignoring other factors like dry air
leading to exhaled droplets drying into 0.12 micrometre virus particles
which stay airborne for longer than the droplets would in humid
air. I am also ignoring sickness keeping people at home,
and so spreading the virus less - which is probably not much affected
by the season.)
I For a given viral insult, the average chance that a person becomes infected.
S The total number of viruses an infected person sheds, at least when in the company of others who have not yet been infected.
The product of these two variables (
I x
S)
has an enormous effect on the spread of the infection. The number
of viruses shed is likely to scale with the severity of the
infection. So even if
I
did not alter throughout the year, we could explain the wide seasonal
variation in spread rate in terms of seasonal changes to the second
variable alone:
S.
The first chart above - seasonality of influenza by latitude - does not enable us to distinguish the degree to which
I or
S
varies, but we know the product of them varies a lot with summer /
winter in locations about 30° or more from the equator, and not much
for locations closer to the equator. (There is, of course,
no summer or winter at the equator.)
The two most obvious mechanisms by which
I and
S
vary at locations 30° or more from the equator (and each could be
affected completely differently by these two mechanisms) are:
W - Summer warmth and comparative dryness vs. winter coldness and wetness, with rain and perhaps snow.
D - Variations in
vitamin D synthesis in the skin due to the Sun shining more directly
downwards in summer, compared to at a shallow angle from the horizon in
winter. (Also, people exposing more skin in the warmer
months.) This directly affects the average vitamin D level of
most of the population. (Even those who get no sun exposure are
caught up in winter waves of infection, due to that year's somewhat
novel flu strain being passed around in most of the population during
winter.)
The second chart is evidence for the hypothesis that the dominant mechanism for changing (
I x
S) is
D, because the women were still subject to strong
W
summer / winter temperature changes in New York State (40.6° north) and
those who took the relatively small 0.02mg (800IU) D3 had hardly any
more episodes of flu or common cold in winter than in any other season.
This second graph also enables us to distinguish whether it
I or
S
which changed most, going high in winter and low in summer. Since
all the women in the trial were a tiny proportion of the population,
their viral exposure was essentially unaffected by being part of the
trial, including when half of them were taking vitamin D.
So, on average, the intervention group suffered the same number of
viral insults, with the same seasonality, as the control
group. This trial's outcomes are unaffected by the viral
shedding of its subjects. So this data supports the hypothesis
that, at least for these women, the variation in their vitamin D alone,
and its effect on their susceptibility to infection alone, was
sufficient for them to escape infection during the winter when they are
most subject to the viral shedding of everyone else.
This doesn't tell us that viral shedding is unaffected by vitamin D, or
by any other seasonal variable. Maybe they are - and it is
obvious that a person who is very sick for a long time will shed more
viruses than someone who has few, if any, symptoms, for a shorter time.
Since these infections were self-reported - not detected by any medical
examination or blood tests - we don't know to what degree the women
were infected with too few symptoms for them to notice as the flu or a
common cold.
What is clear from this data (and there are various other research
studies on vitamin D levels and respiratory diseases, with a range of
outcomes) is that even low levels of vitamin D supplementation greatly
reduced the subjective experience of illness in whatever infections the
women actually had. It is also worth noting that African
American women living in New York state are likely to be generally very
low in vitamin D, especially in winter, in the absence of
supplementation. So even small supplemental quantities
could make a significant difference to the 25OHD levels and to to
improving the strength and regulation of their immune systems.
We also see that 0.05mg (2000IU) vitamin D provided much greater
protection from noticeable infection than 0.02mg (800IU).
This is not surprising.
With SARS-CoV-2, being so infectious and with most people (as far as we
know, and research is continuing on levels of pre-existing immunity), I
doubt if the proclivity to be infected due to a given viral insult
varies a lot between people with low and high 25OHD levels.
The enormous drop in reported flu / cold infections in this trial, due
to 0.05mg (2000IU) D3 a day may not be representative of all people,
but there are numerous research studies indicating that influenza and
viral respiratory tract infections in general (and COVID-19 starts off,
and ideally ends, in the respiratory tract) are made much less likely
and/or severe, for any given viral insult, by higher levels of vitamin
D. For more such research:
I believe that the severity of symptoms and so the degree of viral
shedding will vary enormously between a person with very low 25OHD
levels, such as of these women in New York State in winter without
supplements (perhaps 10ng/ml or less) and such a person having taken
0.05mg (2000IU) D3 a day for a year. We would expect 0.125mg
(5000IU) a day to be still more effective at reducing the chance of
infection and/or the severity of infection and so the amount of viral
shedding.
I am advocating all people - or as many as choose do so with good
information, access their choice of quality supplements at suitably low
cost, and without coercion or unreasonable cajoling or pressure - take
enough vitamin D3 to get their 25OHD levels to the
40 to 60ng/ml
range. This is what we aim for - but there's no time or money,
and not enough labs or doctors, to do 25OHD tests for most of these
people.
The solution needs to scale globally, since I don't know of a single
country where average 25OHD levels are in this range. As you can
read above, this is the range of our ancestors, the range our immune
systems evolved to work from, the level needed for proper autocrine
signaling within immune system cells, and the range recommended by the
best researchers.
By scaling the intake with bodyweight - and probably at a higher
multiplier for weights much beyond average, which indicate overweight
or obesity - we can aim to get people's average 25OHD levels into this
safe and healthy range, without prior knowledge or subsequent testing
of their levels. Some will arrive at levels below 40ng/ml and
some will get to levels well above 60ng/ml, which is OK. See the
d3/
page. This is the best we can do without global testing, which is
vastly more expensive than the actual D3 supplements. The
150ng/ml threshold above which toxicity
might be a problem can only be reached with much higher intakes than are needed when aiming for 40 to 60ng/ml.
It is no good advocating a scheme which works for middle-class people
in developed countries, but not for their poor, remote and/or
indigenous people, or not for developing countries with limited health
infrastructure. The plan has to work for all people.
It need not be expensive - its just a few cents a year per person of
D3, packaged into weekly or fortnightly capsules. Average
weight (say 55 to 75kg): get a pack of 52 capsules each with 0.125mg
(5000IU) and take one a week. Other sizes would be made for
children and young adolescents, and for overweight and obese
people. Morbidly obese people need medical care urgently, so
their doctor can sort out their vitamin D and numerous other
nutritional and medical needs. Sick people need medical
care too. The mainstream program would be to make such capsules,
independently tested, available from multiple manufacturers with good
advice about how to use them. In these quantities, they
need not cost much. However, new pharma grade D3 factories
will need to be built.
As you can read in
https://sci-hub.se/10.1016/B978-0-12-381978-9.10006-X , in
2010 about 90 tonnes of vitamin D3 (cholecalciferol) was
manufactured. About 20 tonnes of this was refined for human
pharmaceutical use and the rest was for agricultural animals.
This 20 tonnes is about 0.009 milligrams (360IU) a day per person,
though of course most of it went to only a few people.
Pharmaceutical grade vitamin D costs about USD$2.50 a gram ex-factory
in 1kg lots. So 0.125mg (5000IU) a day, would cost USD$0.12 a year.
Assume 0.125mg/day (1/8000th of a gram) for 7 billion adults (more
for the overweight, less for children, and some people will choose not
to take it) = 875kg/day = 320
tonnes a year. So we need new D3 factories. There's
no reason to expect the major factories in China and India to export to
other countries once everyone realises how their current production
meets only part of the needs of their own people.
Even a fraction of this would make a big
difference, since (as far as I can tell, based on limited research to
date) the people most at risk have very low vitamin D levels, and even
small daily doses would raise these levels significantly and so reduce
the chance they would suffer serious harm or be killed by their body's
own weakened and dysregulated immune response to what is, for most
people, the relatively benign SARS-CoV-2 virus.
The difficulty, disruption (to medical care, with so many doctors and
nurses vaccinating rather than working in their regular roles), expense
etc. of a global vaccination program can be imagined. It is
far, far, beyond the cost and difficulty of the D3 repletion plan I
propose.
For the sake of the argument, lets assume that global scale vaccination
was about as easy as D3 repletion. Let's assume it is a single
injection and that there is usually no need for medical supervision or
care to deal with serious side-effects.
Here are the arguments which show that even then, vaccination is vastly
inferior to D3 repletion - and why D3 repletion makes vaccination for
both COVID-19 and influenza unnecessary. This is
not
a generalised argument against vaccination. There are good
reasons for vaccinating against other diseases which are still deadly
or exceedingly harmful with perfectly good immune responses and all the
best nutrition. Its just that COVID-19 and influenza are
generally benign viruses (or at least not seriously harmful, in the
case of influenza) and that the whole reason people want to vaccinate
against them is because a small subset of people can be harmed or
killed by the disease AND because that subset is harmed due to
inadequate vitamin D (most importantly, of several nutrients) causing
their immune systems be weakened and dysregulated.
So here we contemplate a vaccination scheme as lightweight as giving
most people about 1/22 of a gram of D3 a year, in weekly capsules,
without need for direct medical supervision.
|
Vaccination
|
D3 repletion aiming for 40 to 60ng/ml 25OHD
|
COVID-19 current and very similar strains
|
Assumed to be effective at
stopping infection, or greatly reducing its severity, to the point
where there would be almost no serious symptoms if people were infected
AND there would be very few people infected anyway, due to herd
immunity. In reality, there are dangers of adverse
reactions, inadequate immunity, variations in how many years immunity
lasts and potentially serious outcomes if the vaccine causes
Antibody-Dependent Enhancement in some people.
|
In the case of infection, will
generally lead to no or mild symptoms, and will make serious symptoms,
harm, and death unlikely except in rare cases where people have
multiple serious comorbidities and immune dysregulation which remains a
problem even with adequate vitamin D. The generally low levels of
viral shedding by most people, if they
are infected, means that the disease cannot spread very far except in
the most extreme situations of close personal contact.
|
A new strain of COVID-19 which evades the immunity elicited by the vaccine
|
The current strains will be
under strong selection pressure to evolve a spike protein which still
attaches to ACE2 but which is not recognised by the antibodies which
vaccinated people produce. Given the global scale of the disease,
this cannot be ruled out. On the other hand, coronaviruses mutate
less than flu viruses and there is at least some cross reactivity
between antibodies raised by SARS-CoV and the SARS-C0V-2 spike protein,
which is functionally different and superior in how it attaches to ACE2.
|
People will handle all new
strains of COVID-19 as they do the current ones, unless the new strain
has evolved to cause far more symptoms with increased viral
shedding. The virus is already highly infectious for a given
viral insult, so there's not a lot of scope for it improving its
performance in this respect. There should be no problems unless
the virus develops an entirely new mode of operation, evading healthy,
strong, well-regulated innate defenses so it causes lots of shedding,
presumably stronger symptoms and so it gets to the lungs and causes
damage there even with well regulated, strong responses,
The virus already attaches strongly to ACE2. Even if it attaches
more strongly, it will be basically the same disease and D3 replete
people will be infected briefly, with the infection being halted in the
upper respiratory tract, at it is for most people today.
|
Influenza
|
No protection against infection or serious symptoms and death.
|
All the above applies to influenza as well.
|
Common cold and other respiratory diseases
|
No protection.
|
All the above applies.
|
Sepsis and ARDS
|
No protection.
|
All the above replies.
Hardly anyone - except those with profoundly damaging pre-existing
conditions - will get sepsis or ARDS. (Still, those who smoke and
abuse their bodies may harm their lungs.)
|
Numerous other chronic and acute diseases
|
No protection.
|
Partial or very substantial protection against dozens of diseases and chronic conditions. See the list above at the end of the #kp section. See also the long list of diseases on the left of the Vitamin D Wiki main page.
|
Need
for medical personnel, syringes, hypodermic needles, refrigerated
transport, privacy invasive record keeping etc. to fan out over whole
cities and sparsely populated areas?
|
Yes.
|
No, but there needs to be good,
well-labeled, inexpensive (or zero cost through government subsidy)
supplement capsules and drops for babies, with a really good,
multi-lingual, education campaign funded by the government and either
approved by or paralleled by similar educational campaigns by
internationally and locally trusted NGOs. This must not be seen
as a purely government initiative, and there must be no coercion, or
any other crap such as only allowing people to travel or work if they
do a 25OHD blood test to prove they are replete.
The same education and supply programs could also support increased
intake of omega 3 fatty acids, boron, vitamin C, B vitamins, zinc, iron
etc.
|
Longer term maintenance
|
Ongoing program for children and
any new arrivals from overseas if not already vaccinated.
At present we have no idea of how long vaccine elicited immunity would
last for. Since it will be impractical to test people
individually, research will show, for particularly sub-groups of the
population, how often vaccination needs to be repeated. Maybe it
will last a lifetime - but this seems unlikely.
|
D3 supplementation needs to be maintained from birth (except for babies breastfed by replete mothers).
|
Other opportunities
|
If medical teams comb the
countryside and reach most settlements, there would be opportunities
for medical checkups and other healthcare services.
|
No such medical contact, except perhaps to reach particularly vulnerable people in remote areas.
|
Overall health benefits for people, and so reduced health costs for governments and better national productivity
|
No improvement on the
pre-COVID-19 situation, which is very poor compared with the levels of
health which can and should be achieved with proper nutrition.
|
There will be profound,
long-term, improvement in health in numerous respects, so boosting
happiness, productivity, reducing health care expenditure, taxation,
poverty and crime.
|
Dependence upon or government?
|
As currently conceived, most
national vaccination plans seem to be the work of government, though
middle-class and wealthy people might have the opportunity to choose between multiple vaccines if
such vaccines exist, are sold in their country and have made it through
government approval mechanisms. Otherwise, this is likely to be a
highly government -centric operation, with all the privacy problems
this entails, and profound resistance by many people (myself included)
against getting injected with some concoction because the government
says it is good.
|
I envisage government support,
but multiple sources of D3, all independently tested and available at
low or perhaps government subsidised zero cost.
There's no need for privacy invasive record keeping or medical involvement for the vast majority of people.
In chaotic third-world countries, it is possible that NGOs might do a lot of the work even if the government is not supportive.
There is technically no need for government support, other than to
allow the sale of this nutrient in the quantities required. For
instance, in Australia, the maximum D3 content of any one capsule is
0.025mg (1000IU) which would make proper supplementation awkward and
expensive.
|
#disclaimer
Disclaimer!
I am
not a doctor. I have no medical training.
I have not even done a first aid course, though I think everyone
should learn this in high school. My positive view of the
research and ideas you read here should not affect your own decisions
about healthcare for
yourself and your loved ones .
You
should read and consult very
widely.
By all means ask your doctor, nurse or naturopath to read this material.
Through their training and day-to-day work, medical professionals
develop a vast knowledge of interrelated considerations about human
health, and use this for your benefit after individually assessing your
condition.
Their knowledge may be incomplete. The medical conventions they
rely upon may be out of step with current research. They may be
excessively wary of supplements and more confident about using drugs,
due to the constant schmoozing of drug companies. Their patients
may be generally tired of dietary advice, and expect quick drug fixes
for whatever ails them. For reasons of professional liability
insurance, and to protect their reputation, doctors may be reluctant to do
anything different from what the main body of medical professionals
seem to be doing - so many of them are bound by a strong herd mentality.
I provide information by way of linking to and quoting from research
articles and - in some instances which I intend to make very clear -
with my own interpretations and hypotheses. But even if I knew
all there was to know about your individual condition, I do not have
the knowledge and experience to do what medical professionals normally
do so well: give reliable guidance tailored to your particular
situation - because I lack their training and experience.
Furthermore, I don't want that sort of responsibility.
If your decisions are influenced by what you read below, it should be
because you have evaluated the arguments, read
the research articles I cite and because
you take responsibility for your own health.
If you
don't
understand what you read here, please rely on the judgment of someone
who does - someone with a broad knowledge of science in general,
biology, nutrition and human health to evaluate the
observations and arguments in the broadest possible context.
I have expanded on a few acronyms with
fuller text and/or [
WP]
Wikipedia links.
Paracetamol (Panadol) is the
same as
acetaminophen (Tylenol
etc.) It reduces fever and is generally not regarded as an
NSAID https://en.wikipedia.org/wiki/Nonsteroidal_anti-inflammatory_drug
- a class of drugs which includes
aspirin
and
ibuprofen.
About
I am an electronic technician working with electronic musical instruments
http://www.firstpr.com.au/rwi/dfish/ .
I also work in computer programming: C++ for mine schedule
optimisation, continuing the work of my father Jeff Whittle. My
wife Tina and I live in Daylesford, north west of Melbourne, Victoria,
Australia.
I created
this website
http://aminotheory.com in 2011
primarily for my new observations and
etiological theory of Restless Legs Syndrome / Periodic Limb Movement Disorder, which I suggest should be known as
Restless Limbs Sensorimotor Disorder:
This is not a commercial site. It generates no revenue.
These web pages set no cookies in your browser. It is a static
site made with
KompoZer.
Contact
I update this material according to new information and any feedback I receive from
clinicians, researchers, or anyone at all.
Please email constructive critiques to
rw@firstpr.com.au
.
Copying
Please quote selected passages in your social media feeds, discussion
forums etc. - always with a link to this page's URL:
Please
do not copy the entire page,
or substantial parts of it, to other sites, since I may update
the text at any time, and I don't want out-of-date versions of this
text floating around the Web.
Plan for better nutrition and guidance regarding fever
(This section was written 2020-05-26 and revised a little on 2020-06-15.)
We insist on proper operating conditions (fuel, oil, water, tyre
pressure, ignition timing etc.) for our cars. We insist on
feeding our cats a diet which makes them replete in all known nutrients
(though boron is not yet recognised as one of them). We insist
the AA batteries which run our devices are 1.5 volts, not 1.3.
Yet only a small fraction of 7.79 billion humans get their proper
operating conditions, which begin with adequate quantities of dozens of
nutrients.
Primary problems concerning immunity, health in general and COVID-19 in particular
Problems and
Solutions:
P1:
COVID-19 spreads quickly unless unsustainable - and ultimately harmful
and deadly - lockdown measures are enforced. If the disease only
caused a week or two of suffering and inability to function properly,
this would not be such a serious matter.
I have broken
P2 into three
sub-types. All these are strongly associated with very low levels
of vitamin D and of other nutrients. However, there is much more
to the interrelated set of health problems we are trying to solve than
lack of vitamin D.
P2c:
Coagulation. With current (generally inadequate) approaches to
nutrition and hospital care, a significant number of people who
contract
COVID-19 die (0.5 to 5%) or suffer
serious harm (5
to 20%). (2020-06-15: The UK death rate is 14% of the confirmed
cases! While the latter is surely an underestimate, the death
rate will rise even if new infections stopped today.) Most of these are
elderly people with known health
problems, but there are lots of people in middle age, in their 20s and
30s - and some children - who are suffering lasting harm and
death.
The main reason for all this harm is
the SARS-CoV-2 virus' ability, once it is replicating in the lungs
(which would not occur if the immune system successfully fought it in
the throat), to elicit a dysregulated immune response which damages the
epithelium (inner lining of blood vessels and capillaries) in the
lung. The fragments of epithelial cells cause the blood to become
hypercoagulative - the natural, evolved, response to these signs of
broken blood vessels.
This hypercoagulopathy causes blood clots (including thousands or
millions of micro-embolisms) to form in the lungs. These, plus
the viral and immune system damage, reduces oxygen and CO2
exchange progressively over a week or so. Beyond a certain point,
unless their breathing is assisted in hospital (with oxygen via nasal
canula, trying as much as possible to avoid mechanical ventilation,
with its sedation, invasive plumbing and lung damage) the person will
die.
Even without significant breathing difficulties, the hypercoagulative
state causes blood clots all over the body, resulting in permanent harm
or death.
P2i:
Inflammation. Many people, particularly as we age, suffer serious harm or are killed by a long list of
chronic and acute illnesses caused by excessive inflammation.
These include diabetes (type 2 and type 1 which strikes in childhood),
asthma, inflammatory bowel disease, neurodegeneration (dementia), some
forms of cancer and the mechanisms by which it metastasizes, multiple
sclerosis, coeliac disease etc.
P2s:
Sepsis. Many bacterial and viral diseases - and some injuries such as
near-drowning and burns - if severe enough, can prompt the immune
system to respond in an overly-aggressive, pro-inflammatory way known
as
sepsis. This develops
rapidly and even with ICU hospital care, often leads to permanent
disability and death. (Though see the Marik Protocol in
icu/
for techniques which achieve better outcomes, in part by fixing the
extreme vitamin C deficiency which afflicts sepsis and most other
patients who need critical care.)
Most deaths caused by influenza are due
to sepsis, in the form of Acute Respiratory Distress Syndrome (ARDS),
in which the lungs are flooded (pneumonia) due to
over-inflammation. This fluid reduces the ability to breathe,
potentially killing the person. Even if this inflammation does
not kill, it may lead to later bacterial infection - bacterial
pneumonia - which again can flood the lungs, damage other organs and
kill.
(Initially, it was assumed that COVID-19 produced a similar form of
sepsis and ARDS. We now know that the virus's direct harm to the
epithelium of the lung, together with the overly-inflammatory response
there, drives an extremely destructive hypercoagulative state, which is
not found in traditional sepsis or ARDS.)
P2c and
P2s are caused to some extent by existing illness and injuries, such as to the lungs, but are primarily caused by
P3w and
P3d:
P3w: The immune system has one or more of its many antiviral, antibacterial, antifungal or antiparasite mechanisms
weakened. This causes no direct harm to the self.
P3d: The immune system has one or more of these mechanisms
dysregulated.
Overly aggressive, overly inflammatory, immune responses ensue, often taking place at the wrong time or the wrong place.
These responses are typically ineffective at combating the
pathogen, but the most important result of this immune system
dysregulation is inappropriate inflammation, including
destruction of cells of the body which do not really need to be destroyed in order to stop viral or bacterial replication.
P2i is caused primarily by:
- P3d on its own.
- P4 (wheat, below).
- By P3d exacerbating the problems caused by P4:
P4 The noxious properties of
gluten proteins in wheat and related grains. Rice and oats are fine.
These grains evolved sulphur
cross-links in the protein of the wheat grain to make them difficult to
digest by birds, animals and insects which would otherwise eat the
grain. These links give rise to wheat's dough's unique stretchy
nature which is essential to bread-making. The linked
sections of protein cannot be broken into separate amino acids by our
digestive enzymes. The resulting protein fragments (the most
notorious one is called
33-mer,
with 33 amino acids) disturb the lining of the intestine and trigger an
immune response there. The whole intestinal lining is in a
constant state of inflamed preparedness, to accept food and defend
against pathogens. This opens gaps in the tight junctions between
the brush-border cells [
W],
allowing lumen (digestive juices, food fragments and bacteria) to enter
the bloodstream, so causing inflammation and other problems throughout
the body. For instance, in some people, wheat causes neurological
problems, such as gluten ataxia [
W] even though the problems in their digestive tract to not result in any noticeable symptoms.
While the sourdough processes used for all bread until the early 20th century
reduces this
disturbance by breaking down the noxious protein fragments, our taste
for wheat condemns many of us to a lifelong struggle against the
ill-effects of these indigestible fragments.
Other plants we eat contain noxious
substances too. Wheat gluten would still cause us some harm even
if our immune system was working perfectly. Today, due to human
genetic variation and unknown triggers, some people suffer intense harm
with coeliac disease, while most of us other wheat-eaters suffer more
subtle forms of harm over a lifetime of eating non-sourdough wheat
products.
There are several contributing causes to
P3w (weak immune responses) and
P3d (dysregulated, overly-aggressive, proinflammatory responses):
P5:
P3w -
Generally poor nutrition (including the separately listed problems of inadequate intake of macronutrients omega-3 fatty acids
P15 and potassium
P16 and of multiple micronutrients, such as vitamin D and boron
P14),
lack of exercise and lack of other essentials for health and happiness
including clean air and water, sunshine, close friends and loving
relationships, social contact, good medical support when needed etc.
P6:
P3w - Prior
injuries and
illnesses.
P7:
P3w &
P3d - Nutritional excesses, such as
salt, omega-6, saturated and trans fatty acids.
P8:
P3w - Use of
recreational drugs
which harm health in general and immunity in particular, including alcohol and
no-doubt tobacco, cannabis, cocaine etc. (Though there are
suggestions that nicotine has anti-inflammatory effects which protect
against severe problems with COVID-19:
#nicotine .)
P9:
P3w
- The use of prescription drugs which weaken immune responses
(immunosuppresants are helpful in some medical conditions, often due to
our lack of helminths) or which cause particular problems with
COVID-19. There has been discussion about particular
hypertension drugs making things worse for COVID-19 patients.
Some drugs such as hyroxychloroquine (for lupus) or others which dampen
down excessive immune responses, such as for asthma or Crohn's disease,
may be protective against severe COVID-19 symptoms. (
Mehra et al. 2020-05-22 report (hydroxy)chloroquine apparently causing heart arrhythmia and being associated with higher death rates and an
earlier RCT showed no antiviral or other benefits.)
Prescription drugs should be continued unless advised by your doctor.
P10:
P3w - Some people seriously curtail their body's initial attempts to fight the virus by
lowering their temperature when they have a fever. See the
fever/ page.
P11:
P3w and
P3d - Individual immune responses differing from from the norm due to
genetic variations. These variations are primarily in the codons of our DNA, but there is also an
epigenetic [
W]
component, in which long lasting (and impossible to change, as far as
we know) methylation and other additions to the DNA occur due to life
experience - including especially in-utero - affect how our bodies
interpret the genes we inherited from our parents.
P12:
P3d - Assuming that the person
does not have any helminth infections (intestinal worms, as described in the previous section), some aspects of their
immune system, due to evolution, being set up for overly-aggressive actions which are not being downmodulated by the helminths our ancestors had. See above:
#helminthsgone . This is the condition of essentially all people in developed
countries - our immune systems, in general, are primed to respond in
damaging, overly-aggressive, proinflammatory ways to many stimuli,
including especially SARS-CoV-2 infection of the lungs.
P13:
P3w and
P3d - People
with helminth infections face
P12 in general, but to some extent these
P3d
excesses will be moderated by the chemicals their helminths
exude. These people may have weak responses to the virus due to
helminthic downmodulation of normally effective immune responses.
Their (without helminths) overly-aggressive responses may persist, may
be downmodulated to being about optimal, with a good balance between
fighting infection and harming the self. These responses may also
be downregulated below the point of optimality - being ineffective
against the virus, and hopefully being still less harmful to the
self.
P14:
P3w and
P3d
- Deficiencies in nutrients which cause significant weakening and/or
dysregulation of the immune system. Of course all nutrition
affects general health and so the immune system, but there are a number
of micronutrients which are important here:
vitamin D,
boron,
vitamin C,
zinc,
magnesium and probably quite a few others.
There are also two macronutrients of
interest in this regard - macro because we need grams of them per day,
not milligrams or micrograms: omega-3 fatty acids and potassium.
Most of what follows on this page, and in the forthcoming 5 Neglected
Nutrients website, concerns vitamin D, boron, vitamin C, omega-3 fatty
acids and potassium. These are all of widely neglected, but are
vital to immune system functioning and to avoiding hypertension and
stroke.
This article is highly relevant, but I haven't read it yet. It
mentions vitamins A, D, C, E, B6, and B12, folate, zinc, iron, copper,
and selenium.
A Review of Micronutrients and the Immune System–Working in Harmony to Reduce the Risk of Infection
Adrian F. Gombart, Adeline Pierre and Silvia Maggini Nutrients 2020, 12(1), 236 2020-01-16
https://www.mdpi.com/2072-6643/12/1/236
|
P15:
P3w and
P3d - We generally don't eat enough
omega-3 fatty acids.
These are synthesized by algae and
eaten by fish - so with oily fish, fish-oil capsules and/or algae oil
capsules, we can obtain decent amounts of omega-3 fatty acids.
Most of the fat we eat in food other than fish contains mainly, or
exclusively omega-6 and saturated fatty acids. Fats are
controversial, but as far as I can tell, we generally eat too much
omega-6 and saturated fat and too little omega-3 fatty acids.
Omega-3 fatty acids [
W]
perform at least two crucial functions. Firstly, they are used to
make some of the prostaglandins (others are made from omega-6s) and
other compounds, which are necessary for proper immune system
regulation.
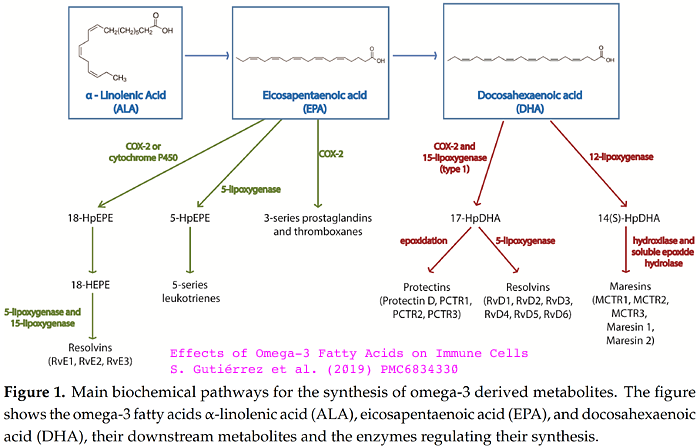
Secondly, the two-fatty-tail phospholipids [
W]
- which make up (with cholesterol) the lipid bilayer cell membrane of
all our cells - have their fatty tails composed of oily tails from the
fats we eat. So the ratio of omega-3 tails to other types of
tails in our cell membranes reflects what we have been eating in the
last few months or year or so. These tails' mechanical properties
vary, and the exact mechanical properties of the lipid bilayer affect
the operation of the complex transmembrane proteins through which many
molecules and ions enter and leave the cell and which form many types
of receptor. These effects are directly mechanical on these major
transmembrane proteins and by way of altering other transmembrane
proteins which, ideally, sit alongside the major ones.
So the exact, mechanical, electrical and chemical behaviour of all our
cells' membrane-bound receptors, calcium channels etc. depend, in some
ways
on the ratio of omega-3
to other fatty acids in our diet. This is especially true of our
neurons. So the ratio of the various types of fat in our diet
affects every aspect of our emotions mood and cognition. Most
people in the West would benefit from less omega-6s [
W], saturated fatty acids [
W] and especially trans-fats [
W]and more omega-3s in our diet.
This article describes the importance of dietary omega-3 fatty acids
for improving immune system regulation, including by decreasing
excessive inflammation, by way of these fatty acids forming part of
lipid rafts which support the transmembrane proteins of CD4+ T-helper
lymphocytes [
W], which play an important role in regulating inflammation, by their secretion of anti-inflammatory cytokines:
P15:
P3w and
P3d - Except for hunter gatherers, some vegetarians and perhaps some people
with modern diets who eat lots of yams, sweet potatoes etc. none of us
get enough
potassium in our diet. This is exacerbated by the fact that we generally consume excessive amounts of salt.
The following account is written from memory after partially reading a
large box full of research articles on salt and potassium metabolism,
hypertension, stroke etc. and especially this excellent book from 2001:
The High Blood Pressure Solution: A Scientifically Proven Program for Preventing Strokes and Heart Disease
Richard D. Moore MD Healing Arts Press; 2nd edition 2001-06-15
https://www.amazon.com/dp/0892819758
|
Our ancestors found it very hard to
obtain enough sodium (and so chloride) through salt, so their tastes
(now ours) evolved to included a strong liking for salt - and our body
has evolved to conserve it.
Potassium was plentiful in the ancestral diet (going back to common
ancestors with chimps etc.), with a potassium to sodium ratio
(by mass) of 20 to 40. We have no taste for potassium and our
bodies do not
conserve it.
Every cell in our body relies on pumping potassium ions into the cells
and sodium ions out for its trans-membrane voltage, and ionic
balance.
This voltage and the two opposing ionic concentration gradients powers
the operations of many
trans-membrane proteins. So the exact voltage and concentrations
of
the two ions on either side of the membrane constitute some of the most
important operating conditions for each cell. Some cells, such as
neurons, devote 70% or so of their entire energy budget to pumping
these ions, with various transmembrane proteins powering their
operation by letting sodium ions back in and the potassium ions out
again.
Now salt is easy to obtain (actually almost impossible to avoid,
since it is needed in bread-making, and is in most manufactured foods),
we eat lots of it.
Potassium is primarily found in vegetables and fruits. There is little in grains, eggs, dairy, fish, poultry or meat.
Consequently, many people ingest 2 to 4 grams of sodium a day, and only
2 grams or so of potassium. Ideally we would have 1 to 2 grams of
sodium and 5 or more grams of potassium.
The very low - below 1.0 for many people - potassium to sodium ratio in
our diet directly drives ill health in general and hypertension and
stroke in particular. For more information on this, with research
references, and for the little known option we have for supplementing
potassium via potassium gluconate solution, please see the
kna/ page.
COVID-19 is causing stroke in many people, including younger people who
do not get particularly severe symptoms. A contributing factor to this
is surely excessive sodium and insufficient potassium. I advocate
reducing salt, but not, in the short term, supplementing potassium.
While it is surely better to supplement potassium, and so avoid
hypertension and so hypertension drugs, and to reduce reduce the risk of stroke, there are some tricky
aspects to it and I an not suggesting people rush into this without
their doctor's supervision.
Unfortunately, I think most doctors are
unaware this ability to supplement with 2 or 3 grams of potassium a day
- and quite a few would find the prospect alarming. Richard
D. More explains that in medical school, it is impressed upon all the
trainee doctors, how careful they must be with intravenous potassium -
because excessive input (faster than the cells can absorb it) will
raise blood levels and so cause potentially deadly heart disturbances.
We can't stop the virus spreading, or change the genes which evolved in our ancestors
We can't stop the virus from spreading to most people, in all countries, since:
- It is highly infectious and (with possible partial exceptions due
to previous SARS or other infections - and perhaps BCG vaccinations) we have no immunity to it.
- There is no prospect of an antiviral drug preventing infection.
- It is unlikely that a safe, effective vaccine will be deployed to
most of the population of all countries any time soon, or at all,
because it is very difficult to devise such a vaccine (especially with
viral mutation) and to prove beyond reasonable doubt that it is
effective for most people and is highly unlikely to cause any harm,
including by making future infections more severe.
- The only effective measures against spread are intolerably costly
and deadly for more than a month or so: lockdown and other economically
and socially crippling restrictions.
We can't change people's DNA or its epigenetic attachments.
We can't stop the virus from causing a substantial proportion of the
population to suffer fever, cough and other moderate symptoms for a few
weeks.
Nor can we coexist with COVID-19 by using vaccines, antivirals or lockdowns
Even if there were drugs with powerful antiviral or
inflammation-dampening properties, we can't manufacture or distribute
them in sufficient quantities, with sufficient medical oversight, to
most people in the world in a few months - or probably over years.
We can - and must - improve nutrition to correct many of the
failings which cause people's immune systems to be weak and/or
dysregulated
Problems and
Solutions:
S1: The
public should be advised, in general (with whatever exclusions properly apply) that they should
not lower their fever, with drugs or other means. This is potentially a complete solution to
P10.
However, since it is impossible and
generally undesirable to advise people to do this against the wishes of
most doctors in general, and their doctor in particular, and since many
doctors (I don't know the proportion - I guess 20% to 80%) still
support the use of anti-pyretic drugs in general, and so I guess with
COVID-19, this could only be fully achieved if we somehow solve another
problem:
P20: How to
convince the great majority of doctors of the need for this advice, in the next few weeks,
so their united position will cause health authorities to promptly
issue the required advice to the public, with the backing of almost all
doctors. There is an urgent need for this, since the next
wave of COVID-19 infections are coming, with lockdowns impossible to
extend. (At least in the northern hemisphere, I hope people will
get some sunlight on their skin over their summer and so boost their
vitamin D levels a little.)
In principle this could be done by having them all read the research, such as that which I found and link to at the
fever/ page. However, there are challenges regarding doctors changing
their minds, rapidly, about a matter on which they have long held a contrary
position. Arguments against lowering fever with antipyretics have
been controversial for decades, and some doctors recognise the
essential role fever plays in fighting infections. There is a
long way to go, and here we run into numerous reasons - not all of them
good - for the great resistance to change and new information which for
many or most members of the medical profession constitutes a profound
herd mentality.
Ideally there wouldn't be any urgency, and the doctors who still
advocate lowering fever could be gently cajoled and convinced of the
need to (generally) let fever do its work, over decades. This
would be the polite thing to do, and would respect doctors' dignity and
professionalism.
The trouble is, that with COVID-19 inducing protective fever in a large
fraction of the population in the months to come, waiting and hoping
for doctors to change their mind would vastly increase suffering, harm
and death.
I think
P20 is
insoluble. Therefore, any improvement on the currently parlous situation - (
P10)
of people lowering their fever and so frequently suffering a more
prolonged illness with more harmful and deadly hypercoagulation - will
result from partial or full solutions to
P21 and/or
P22:
:
How to convince health authorities to issue good advice against lowering fever for COVID-19 and perhaps other diseases, with suitable exceptions) despite a lack of consensus on this among doctors.
I regard P21 this as insoluble,
since authorities generally would only advise according to broad
consensus among doctors, and since many people would not accept such
advice even if it was contrary to their understanding of doctors' consensus views.
P22:
How to convince most people to ignore the opinion of many doctors, including perhaps their own AND the absence of suitable guidance by health authorities, with them
placing more trust in the advice of particular doctors they know to be respected, and who advise (with suitable exceptions)
against lowering fever for COVID-19 and/or in general.
This can probably be achieved to some limited extent, with Internet communications. It
would be a pretty dodgy for this to be done by people like me who lack
medical training, so I hope that the solution will be along the lines
of:
S2: Directly to
P22, indirectly to
P21 and
P20 and so towards fully achieving
S1:
Well-respected
doctors and nurses communicate their advice on letting fever (in
general, with suitable exceptions) do its work - primarily to the
public, and secondarily to other doctors and nurses.
On paper, the Ivory Tower Academics [who want RCTs before introducing any new treatment]
will always look better. Their arguments are technically
impeccable. It’s easy for them to paint themselves as the paragon
of scientific virtue, while shaming others as irresponsible
dilettantes. However, the closer one gets to the bedside struggle
against COVID-19, the less compelling these intellectual arguments
become. Thus, I daresay that among frontline providers actually
caring for patients with COVID-19, the rogue cowboy mentality [who use RCT-unproven therapies which seem safe and effective] often has greater appeal.
|
I think
emcrit.org articles and discussions I have read are the very heights of erudition, thoughtfulness and pertinence.
However, see Dr Roger Seheult's
Update 74
in which he cites a CNN interview with YouTube CEO Susan Wojcicki, who
states that videos which contradict the WHO's COVID-19 advice
contravene YouTube's Terms of Service - so raising the spectre of academic censorship in the middle of a crisis.
: Directly to
P7 and
P8, and so in part to
P3w &
P3d - Everyone should be advised
not to drink alcohol (or at least not to drink it regularly or to the point of intoxication)
or use excessive salt - and of course not to harm their immune systems with other recreational drugs.
This is basic, uncontroversial, medical
advise which can safely be given to everyone. So there should be
no problems with changing doctor's thinking, or any controversy.
Again, it is unseemly for non-medicos such as me to be leading the
charge here. So doctors and nurses should communicate directly
and urgently with the public, and with their patients, as well as
advocating health authorities to issue suitable directives.
Only a subset of people will take any notice, but it will help.
(There is a
suggestion
that some cannabis compounds might reduce COVID-19 severity. Maybe so,
but this is of no interest to me since there's no way of deploying such
compounds or any other drugs to the population in general in any time
frame, let alone the months we have to cope with the second
wave of COVID-19 infections.)
: We
can and should urgently reduce the toll of harm and death for
hospitalised patients, even within the currently poor nutritional
arrangements by which most people live. See the
Marik Protocol icu/ .
However, this would only relevant for the general population if all the
people who start to develop the hypercoagulative state are able to be
treated in hospital very promptly. People at home with symptoms
continuing beyond a week or so, beyond the throat infection stage, with
the virus replicating in their lungs, develop this hypercoagulative
state and so are at high and ever-increasing risk of serious harm or
death from blood clots forming in their lungs, brain, spinal cord,
heart, liver, kidneys etc. People at home are suffering permanent
neurological damage, stroke, heart attack etc. Children and babies are
suffering and dying from a form of Kawasaki disease.
Generally (New Zealand potentially excepted) national governments can't
slow the spread of the disease sufficiently to ensure that the 20% or
so of their people who do get lung infections can all go
immediately to hospital. If they could, then in principle it
would be possible to fully achieving S4, which would have huge benefits and largely solve P2c.
In order to achieve S4 (ignoring for the moment that we can't generally slow the infection rate as just mentioned) we
face problems regarding conservatism, herd mentality and getting
changes made to departmental guidelines in a hurry similar to those
mentioned above regarding fever (S2). As with S2 and S3
it would be unseemly for non-medicos like me to be advocating change,
so it is vital that doctors and nurses work within their professions,
and by communicating to the public in general, about the need for
hospital treatment protocols such as those pioneered by Dr Marik, which
result in far less harm and death than is the norm in most hospitals so
far (to May 2020 at least).
However, even if S4 was fully achieved, this is only relevant for the general population to the extent that all the people who start to develop the hypercoagulative state are able to be treated in hospital very promptly.
People at home with symptoms continuing beyond a week or so, beyond the
throat infection stage, with the virus replicating in their lungs,
develop hypercoagulopathy and so are at high and ever-increasing risk
of serious harm or death from blood clots forming in their lungs,
brain, spinal cord, heart, liver, kidneys etc. People at home are
suffering permanent neurological damage, stroke, heart attack
etc. Children and babies are suffering and dying from a form of
Kawasaki disease.
The Marik protocol works, in part, by solving a severe nutritional
deficiency, of vitamin C, by way of intravenous vitamin C (ascorbic
acid) around 10 grams per day.
I believe these techniques could be improved by repleting patients'
deficiencies of vitamin D, boron and other nutrients as well.
However, the earlier all these nutritional deficiencies are fixed, the
better - so that the people don't get seriously ill and never need to
go near a hospital.
Other solutions having been highlighted, we now focus on nutrition
to improve the function of the immune system, general health and to
reduce hypertension and the risk of stroke
So the remaining solutions to the problem of COVID 19 - beyond
sustainable
hand-washing, social distancing etc. - all concern improving the
nutrition of adults and children so that their immune systems are
strong and well-regulated, to solving, to the greatest extent possible:
- the central problem P2c/i/s (Coagulation, Inflammation and Sepsis) - COVID-19 causing serious harm and death - by solving, to the greatest extent possible:
- P3w/d - weak and dysregulated immune systems - by solving, to the greatest extent possible:
- P14 and so P3a and P3b
- Deficiencies in nutrients which cause significant weakening and/or
dysregulation of the immune system.
Unfortunately, we can't fix the fact that human immune systems are
bound to be dysregulated in the absence of helminths. I believe
that for most people, a great deal of currently lacking immune system
regulation can be restored by repletion of micronutrients, especially
vitamin D and boron, even though are genes predispose us to
overly-aggressive inflammatory responses.
There are several levels on which this can be achieved:
- As individuals and families, deciding to take the relevant
supplements, being able to do so (the supplements being available and
affordable) - either due to personal decisions or in accordance with
advice from doctors or health authorities. Initially, this
will need to be in accordance with the subset of doctors who advocate
such supplementation, since I have no idea how long it will take for
most doctors and authorities to overcome their long-established pattern
of avoidance and ignorance of nutritional supplements.
The extent to which doctors' caution about supplementation is valid (is) will be
the subject of a section below. There are reasons to be
concerned, but overall, I believe these concerns are blown out of all
proportion, especially given the urgent need to deal with COVID-19
triggering a billion or so people's dysregulated immune system into
harming and killing them.
- At the level of individual doctors, clinics or hospitals and so
their their patients, including especially those at home who need to
prepare for COVID-19 infection in the weeks and months to come.
- At the level of countries, where governments act decisively to
facilitate the practical, educational and other aspects (medical
guidance, identification of individuals with unusual nutritional needs
etc.) of a campaign to get all their citizens replete in the nutrients
they need to protect them from COVID-19 harm and death.
I am not advocating mandatory
supplementation - just clear advice and logistical and economic support
for the entire population to become replete in these nutrients, in the
hope that most people will follow this advice.
So
S5 is the project which these web pages are intended to facilitate:
Getting
people - individuals, families, countries and ideally all humans -
replete in the nutrients which are essential for proper health, in
particular immune health.
This will largely protect them against the worst symptoms of COVID-19, so we can let the virus run
and do away with unsustainable measures which attempt to slow the
spread of the virus. This will also greatly reduce the death toll
from influenza - so reducing the need for vaccinations. This will
also greatly reduce the prevalence of chronic illnesses due to immune
system dysregulation. This is a far bigger problem, in the long
run, than COVID-19.
In order to achieve this, there are a number of problems to solve:
P30:
Identify which nutrients are required, and in what quantities in
general - and for particular individuals and people with particular
medical conditions.
P31: Entwined with
P30,
get enough doctors to agree on this, since - except for a few
individuals and families who trust either their own judgment or that of
remote (via the Internet) doctors who advocate proper supplementation -
most people and all governments will take the required actions only when
there is broad consensus to do so among doctors.
P32: Entwined with
P30 and
P31,
review all available research and arguments and come to the right
conclusions regarding what the nutritional advice should be, despite
this differing significantly from the consensus view of the medical
profession in recent decades.
For instance, the dosages of vitamin D3
we need for COVID-19 survival (and for general health, avoiding to the
greatest extent possible, without helminths, the plethora of
inflammatory disorders) exceed not just the recommended dosages many
doctors and government health authorities recommend, but their maximum
tolerable doses too.
Likewise the desired 25OHD levels. Some doctors are happy to aim
for getting most people above 12ng/ml (30nmol/L). This might be
enough to avoid rickets, but to make people safe from COVID-19, we need
to get everyone safely over 40ng/ml. So we should be aiming for 40
to 80ng/ml. Toxicity may
occur, for most people, above 150ng/ml, which can only be achieved by
long-term usage of much higher doses of D3 than are required to get
most people to > 40ng/ml. There may
also be problems with the subset of people with unusual genetics for
vitamin D enzymes, with granulomatous diseases or tumors.
In the case of boron, only some researchers and a few doctors recognise
it as nutrient - though it has long been recognised as safe in daily
doses up to 20mg. As far as I know, we probably need 6 to 12mg a day to be boron
replete. (Tina and I take 12mg.)
In trying to solve these problems, the material at this website (below,
I will work on completely revised versions for vitamin D and boron) is
concerned with
biological reality, as best we can understand it from all research and
observations AND the beliefs of most doctors - not least because their
general wariness about nutritional supplementation has some basis in
reality, at least for some subsets of the population.
Recent updates are above this point.
Below is what I will work on next, when I get time. All that follows will soon be greatly revised and reorganised:
#msg
Updated version of the message I wrote to clinicians and researchers in late March
Contents
#00-survival
Poor survival rate once people need breathing assistance
Most people's battle against the virus will be lost or won at home,
not in hospitals or doctors' clinics. Zhou et al. (below) report
that of 34 patients receiving invasive mechanical ventilation or ECMO [WP], only 1 survived. The
survival rate for non-invasive ventilation was 2/26 and for nasal
breathing support, 8/41. Antivirals and antibiotics help, but we
will soon run out of these.
Coronavirus home remedies as suggested here - nutritional supplements
to enhance immune system function, especially by reducing the
overly-aggressive pro-inflammatory responses which cause sepsis -
can make a substantial contribution to public health in this
disastrous situation, given doubling times of half a week, and the
impossibility of retaining sufficient social distancing for 6 months or
more.
#01-fever
Clear guidance regarding paracetamol, ibuprofen, aspirin and NSAIDs
in general
Please see the separate page on this: http://aminotheory.com/cv19/fever/
.
#02-sepsis
Reducing the cytokine storm of sepsis
The cytokine storm, lead by
IL-6, TNF-alpha and other
pro-inflammatory cytokines is the primary or sole cause of death - and
probably of pneumonia and so most hospital admissions. The graphs
in Fei Zhou et al. Clinical course
and risk factors for mortality of adult inpatients with COVID-19 in
Wuhan, China: a retrospective cohort study
www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30566-3/fulltext
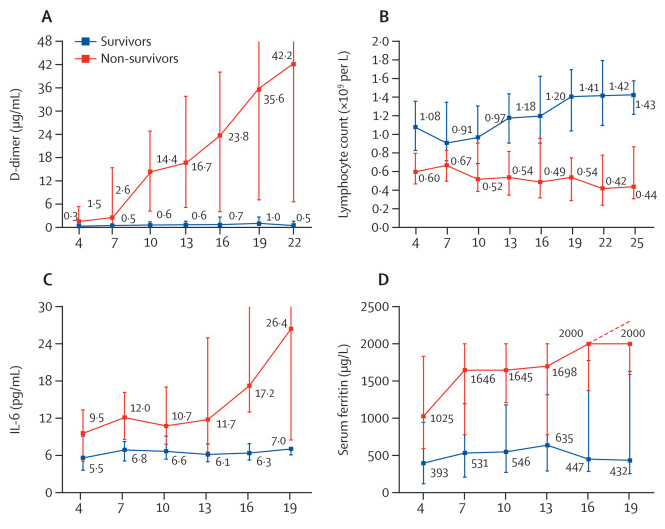
show that those who survived usually did so without radically
elevated IL-6 levels, and that those whose IL-6 levels kept on rising
died. Thrombosis (D-dimer) increased progressively in those who
died, but not in survivors. These averages are extremely
divergent. Serum ferritin kept rising in those who died,
indicating not iron overload, but (www.bmj.com/content/351/bmj.h3692.full)
excessive inflammation.
The real enemy with COVID-19 is not the virus itself, but the
excessive and inappropriate inflammatory response to it - the
same thing which drives sepsis, neurodegeneration (Alzheimers,
Parkinsons), osteoporosis, diabetes etc. One probable cause of
this is that some aspects of our immune system are far more aggressive
than they should be, due to them evolving in the presence of ubiquitous
infection with intestinal parasites and/or H. pylori, both which
attenuate these mechanisms. However, now is not the time for
helminthic therapy. (Google
search for helminthic therapy.)
Another set of causes, which can be fixed - and must be fixed in the
next few weeks in order to prevent millions of deaths - are nutritional
deficiencies, particularly in vitamin D, boron, omega 3 PUFAs and
probably other nutrients such as vitamin C. For brevity I state
the following arguments as if they were facts.
The overly-aggressive
inflammatory response which drives sepsis is supposedly not
understood: www.sepsis.org/sepsis-basics/what-is-sepsis/
. However, a Google scholar search for inflammation
and helminths makes it clear that our lack of intestinal parasites
now plays a major role in the excessive,
inappropriate, inflammatory response which drives asthma,
Alzheimers
/ Parkinsons
disease (and other forms of neurodegeneration),
osteoporosis
, Crohn's
disease, periodontal
disease, atherosclerosis
etc. etc.
It is also clear, as you will read below, that common nutritional
deficiencies also drive this inflammation.
Perplexed sidebar:
Why,
given all this research, do so many disease support groups, clinicians
and some researchers fail to recognise that inadequate nutrition (and
with salt, inappropriate nutrition) drives our overly-aggressive
inflammatory response?
Electronic
technicians make sure power supply voltages are correct before
attempting serious fault-finding. Motor mechanics don't work on
poorly performing engines without checking the fuel. Farmers fix
problems with their animals by feeding them correctly. For
instance lameness in pigs is routinely fixed with borax: 2005 article Boron
Supplementation Prevents Osteochondrosis in Growing Swine.
Why do doctors put so much
effort into drugs and acute interventions and so little into nutrition
to ensure the body works well in the first place?
A possible answer is that highly
skilled clinicians, researchers and disease support group people
dedicate their lives to helping people with complex, devastating
diseases and
can't believe that the primary or sole cause of the disease is several
well-researched nutritional deficiencies and excesses which can be fixed.
I have no problem believing this. Electronic devices can
misbehave in all sorts of complex and perplexing ways due to simple
causes such as electrical leakage on the circuit board, temperature
sensitive intermittent failure inside an integrated circuit etc.
Many fault symptoms are complex, and there is usually one or sometimes
two simple (once you find
them) underlying problems which explain it all. Electronics is
complex, but it is child's play compared to cell biology, multicellular
life forms, genetics, immunology, neuroscience etc.
It makes perfect sense to me that human health is terribly impacted due
to one or more nutritional conditions not being met for most people in
our normal lifestyle. We have hundreds of operating conditions
and if only one of them is outside of a proper range, bad things will
happen. There's probably dozens of inputs not being adequately
met. I believe boron is the nutrient most people are most
deficient in. Then vitamin D, potassium, omega 3 fatty acids.
After that are the better known deficiencies such as iron.
It is so much easier to fix these things than live with the
consequences. The fix can't be achieved entirely with food - we
need supplements.
Most people wouldn't tolerate such ill-care for their car. It
would be unethical for a mechanic to be changing valves and pistons on
the engine, adding additives to the oil etc. in an attempt to solve the
problems caused by a fuel or air blockage, or contaminated fuel or
lubricating oil.
T
here can be enormous inertia in
some areas of medicine. See the section #ssc
below for 22 pulmonologists
raising 6,267 signatures in a petition to change what they argue is
damaging guidance on treating sepsis from a major international sepsis
treatment authority.
Starting in March 2020 and peaking in May, June and beyond, billions
of people will contract COVID-19 and a substantial fraction of them
will be pushed into sepsis-induced pneumonia, respiratory distress and
organ failure - with a high risk of lasting disability and death.
Doctors, nurses and health
organisations have an urgent responsibility to read the research and
make the
connections so they can advise
everyone on readily available nutritional supplements which will reduce
the incidence of sepsis in the months to come. These
levels of nutrition are known to be safe. There is no need, or
time, for RCTs.
#03-vit-d
Vitamin D3
Please see the section below #03-vit-d-dose
which lists doctor's vitamin D3 recommended doses for prophylaxis and
for those with COVID-19 infection. Dr Paul Marik recommends
5000IU in both cases.
Vitamin D
deficiency is a major causative factor for Acute
Respiratory Distress Syndrome, which is what kills most people with
COVID-19.
This
boldly titled open access article makes it abundantly clear that very
low levels of vitamin D3 are an essential precondition for most cases
of ARDS. This is cited by 62 other articles.
Dancer RCA, Parekh D, Lax S,
et al.
Vitamin
D deficiency contributes directly to the acute respiratory distress
syndrome (ARDS)
Thorax 2015;70:617-624.
thorax.bmj.com/content/70/7/617
Patients
with and at risk of ARDS are highly likely to be deficient, and
severity of vitamin D deficiency relates to increased epithelial
damage, the development of ARDS and survival.
Following adjustment for gender, age, diagnosis, staging data, and
pack-years [smoking], patients with
vitamin D3 less than 20 nmol/L
had a 4.2-fold higher odds of ARDS
than patients with vitamin D3 greater
than 20 nmol/L (p=0.032).
|
20nmol/L = 8 ng/ml. This is a very low vitamin D level.
Many of these people are dying due to an easily correctable, extreme,
nutritional deficiency! Every supermarket has vitamin D3
capsules. If they took one or two of these a day they probably
wouldn't be in hospital at all.
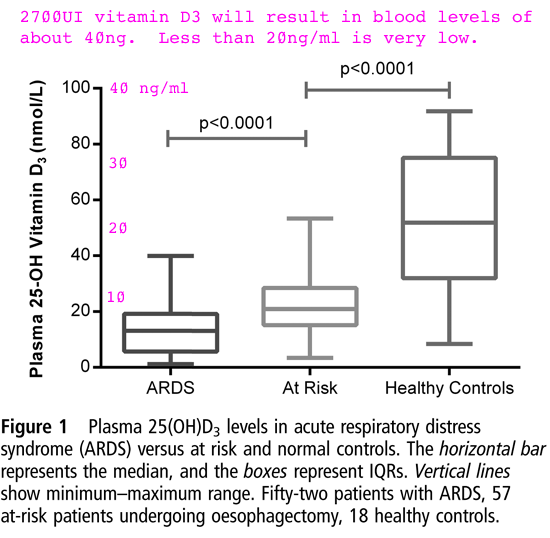
COVID-19
kills most of its victims due to ARDS (WP).
This results from the same overly-aggressive
pro-inflammatory sepsis which kills people with heart, kidney or liver
failure even if their lungs fail and they are on a ventilator or ECMO.
COVID-19
is just another triggering condition, one of many, for ARDS.
However,
it may have unique characteristics which make it a particularly severe
trigger. One such mechanism, which it shares with SARS, is that
the
virus attaches to ACE2 (WP)
transmembrane proteins in particular types of
cells in the lungs, liver and other organs. When it attaches it
causes
the ACE2 molecule to be pulled into the cell, with the virus still
attached.
COVID-19 sufferers surely have significantly fewer active ACE2
molecules available to play their role as an enzyme in the
renin-angiotensin system, where moderates processes which increase
blood pressure and have numerous other local effects in particular
organs
A 2008 explanation of this system is: journals.physiology.org/doi/pdf/10.1152/physrev.00036.2005
.
The extremely low vitamin D level of ARDS sufferers might, in part, be
explained as an effect of ARDS or of other processes which accompany or
drive it. A much more important explanation for this relationship
is that vitamin D deficiency directly causes
or at least significantly
contributes to
the sepsis - the overly-aggressive pro-inflammatory response - which in
this scenario manifests as the condition we know as ARDS.
A Google Scholar search
for ARDS and vitamin D turns up plenty of
articles, but none yet on an RCT involving vitamin D supplementation.
Another perplexed sidebar 2020-03-31 - this time really perplexed:
With
its current rate of spread, and the health and vitamin D status of the
population as it is now, this disease can be expected to kill millions
of people in these ways in the next few months.
Research clearly
shows that ARDS sufferers - due to a variety of causes other
than COVID-19 - are highly deficient in vitamin D3.
There's no
reason to think that the subset of people who COVID-19 kills in this
way are not also, on average, highly vitamin D3 deficient.
We are now 3
months into this global pandemic.
Why hasn't the
WHO told everyone to supplement vitamin D3?
If they had
issued such advice, it would have been followed very widely by now, and
would probably save millions of people's lives in the next few months.
The causative
role of vitamin D in ARDS is no secret. See below for articles
which confirm it.
Vitamin D is not
controversial, obscure, expensive or dangerous.
It is not a drug with side-effects. It is safe and very well
researched nutrient. So there's no need for an RCT to prove
beyond reasonable doubt that supplementation would reduce the incidence
of ARDS deaths and disability due to COVID-19.
ARDS isn't the only lung problem caused by vitamin D deficiency.
Vitamin
D deficiency (VDD) is closely associated with lung diseases, including
asthma, cystic fibrosis, interstitial lung disease, chronic obstructive
pulmonary disease (COPD) and respiratory infections.
|
#2016-Han
Here is a 2016 placebo-controlled double-blind RCT giving ICU patients substantial loading (bolus) doses of vitamin D3. Of
course it would have been better still if they had taken vitamin D
supplements all their lives. Then they probably would not be in
ICU at all.
There is a
high prevalence of vitamin D deficiency in the critically ill patient
population. Several intensive care unit studies have demonstrated an
association between vitamin D deficiency = less than 20 ng/mL (see
above and below, this is a very low level) and increased
hospital length of stay, readmission rate, sepsis and mortality.
Subjects were administered either placebo, 1.25mg (50,000 IU) vitamin D3 or 2.5mg (100,000 IU)
vitamin D3 daily for 5
consecutive days.
There was
a significant decrease in hospital
length of stay over time in the 6.25mg = 250,000 IU
and the 12.5mg = 500,000 IU
vitamin D3 group, compared to
the placebo group:
25 ± 14
and 18 ± 11
days compared to 36 ± 19
days, respectively.
(p = 0.03). (This means that an outcome would only have
occurred by chance once in 33 such trials.)
|
With the knowledge from this trial, how is it ethical to admit
people to hospital like this and not
give them 500,000IU (12.5mg) vitamin D3 in the first 5 days?
Its not expensive, or risky.
Tina and I take one 1.25mg (50,000 IU) capsule a
week. We also
get some vitamin D in multivitamins and calcium citrate tablets.
(We also take magnesium citrate, B complex, zinc multivitamins and 4
grams of fish oil a day.)
Until 2021-08-20 we linked to the manufacturer's site and had a picture
of the 100 capsule bottle. However, due to FDA rules prohibiting
advertising of any non-approved treatment for COVID-19, the
manufacturer asked me to remove such references. Please email me
if you want to know what the product is.
The cost is USD$30 for 100 capsules. The cost
of giving ICU patients 500,000 IU
vitamin D (12.5mg) is USD$3.00. To save:
36
- 18 =
18 days in hospital
So the cost of avoiding one day in
hospital, with vitamin D supplementation = USD$0.17.
If the drug companies found a patentable compound with this
effectiveness and safety profile, they would be selling it for $100 per
capsule AND they would be advertising it to doctors and the public AND
everyone would think it was a modern marvel and be very happy to pay
good money for it.
Instead, because it is a cheap nutrient, which no-one makes much money
from, hardly anyone sings its praises - and year after year, people
suffer grave illness and death, with billions of dollars of hospital
and drug costs, since only a subset of the population use it.
Doctors do, at times, advise their patients to take vitamin D3, omega 3
fatty acids and other nutrients. However, it is my impression
that the dosage can be rather low, such as 2000IU or less, when
research (below) indicates that about twice this would better protect
against numerous diseases.
Vitamin D3 is exceedingly inexpensive. At PureBulk a powder
made
up of 0.2549% vitamin D3 sells for USD$93 per kilogram. This
contains 2.549 grams of vitamin D3, at a cost of USD$36.48 per
gram. At 4000IU a day, this would last for 69 years. At
this rate, the 5 million IU (125mg) in the above bottle would cost
USD$4.56.
At this price, the cost of saving 18 days in hospital would be USD$0.46.
In bulk, a kilogram of pharmaceutical grade vitamin D3 (colecalciferol
USP) costs USD$13,553 from a US supplier (link),
or USD$2500 from a Chinese
manufacturer (link).
100 years supply at 4000IU a day is 3.7 grams, which is USD$9.25 at the
Chinese wholesale price. So, not counting the cost and effort of
splitting it into 5,200 weekly capsules (there's no need to take it
every day), a vast array of diseases and chronic conditions could be
largely or entirely avoided, for 9
cents a year.
It is clear that vitamin D deficiency plays a crucial, causative, role
in many lung diseases. It is reasonable to assume that it plays a
crucial role in most of the suffering and death caused by
COVID-19. The same would be true of the most serious consequences
of influenza.
If everyone in the world took a decent amount of vitamin D, such as
4000IU, it would be reasonable to expect that COVID-19 wouldn't be such
a big deal. It would be a new virus, which makes some people ill
for a while, and it would cause few if any deaths worldwide.
So the entire human world is being
disrupted, and hundreds of thousands or millions of people are going to
die because they didn't take an adequate vitamin D supplement?
As far as I can see, this is true.
So why are our health authorities not urging everyone to take vitamin
D? Now? Or years ago? Hopefully they will.
There would be far less work for doctors and hospitals, and billions of
dollars less spent on drugs. One can imagine a conspiracy of drug
companies suppressing vitamin D, boron etc. but I don't think they are
doing this.
It is as if the medical profession is focussed on sick people, the
complexities of their illnesses, and the costly, difficult and
sophisticated acute interventions they have learned to help these
people get well again.
Yet it is easy and inexpensive to fix these nutritional deficiencies
such as for vitamin D - which would save so much suffering. It is
a easier than supplementing with potassium, (see kna/
) but that is easier and better than using blood pressure drugs.
It is a lot easier than getting people to give up smoking. And
that is easier than having to cope with the damage smoking causes.
A 2014 article PMC4220998
relates blood levels to vitamin D3
supplement quantities for underweight, normal, overweight and obese
people. For normal weight people, 4000 IU/d provides 117 nmol/L,
which is 47 ng/ml. Toxicity (PMC6158375)
occurs with blood levels more than three times this.
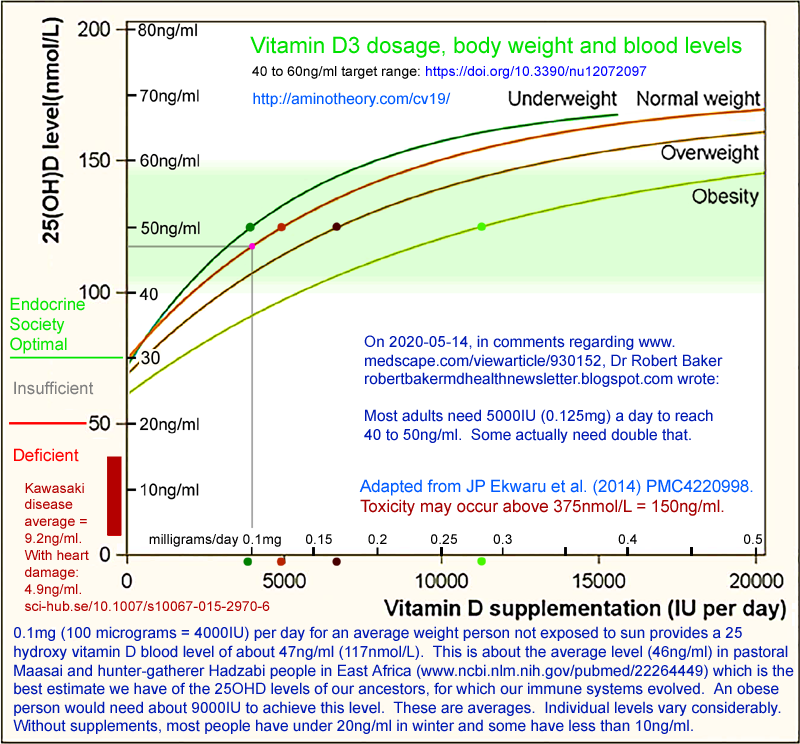
If all adults (who wisely have little UVB exposure) took 4000IU
vitamin D3 a day (a gram every 27 years) then they would avoid most of
the diseases caused by vitamin D deficiency. This
chart from Garland et al. 2014 PMC4103214
shows the importance of achieving at least 40ng/ml.
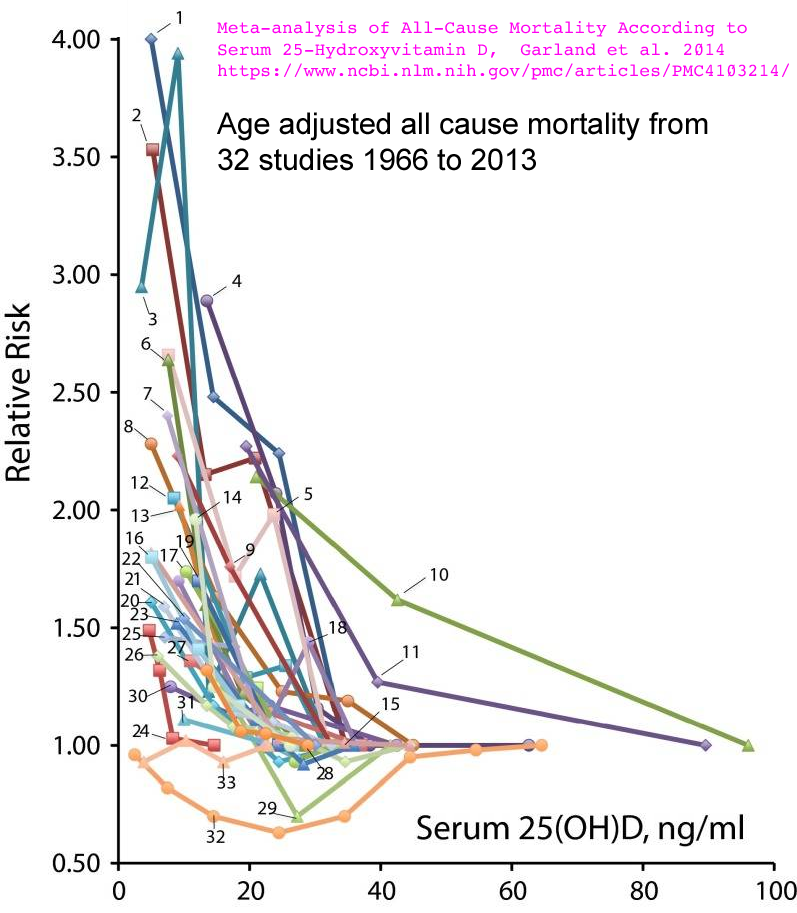
A chart from one of the co-authors, (vitamindwiki.com/Chart%20of%20Vitamin%20D%20levels%20vs%20disease%20-%20Grassroots%20Health%20June%202013)
labels the various conditions:
(Right click the image to see it at full size.)
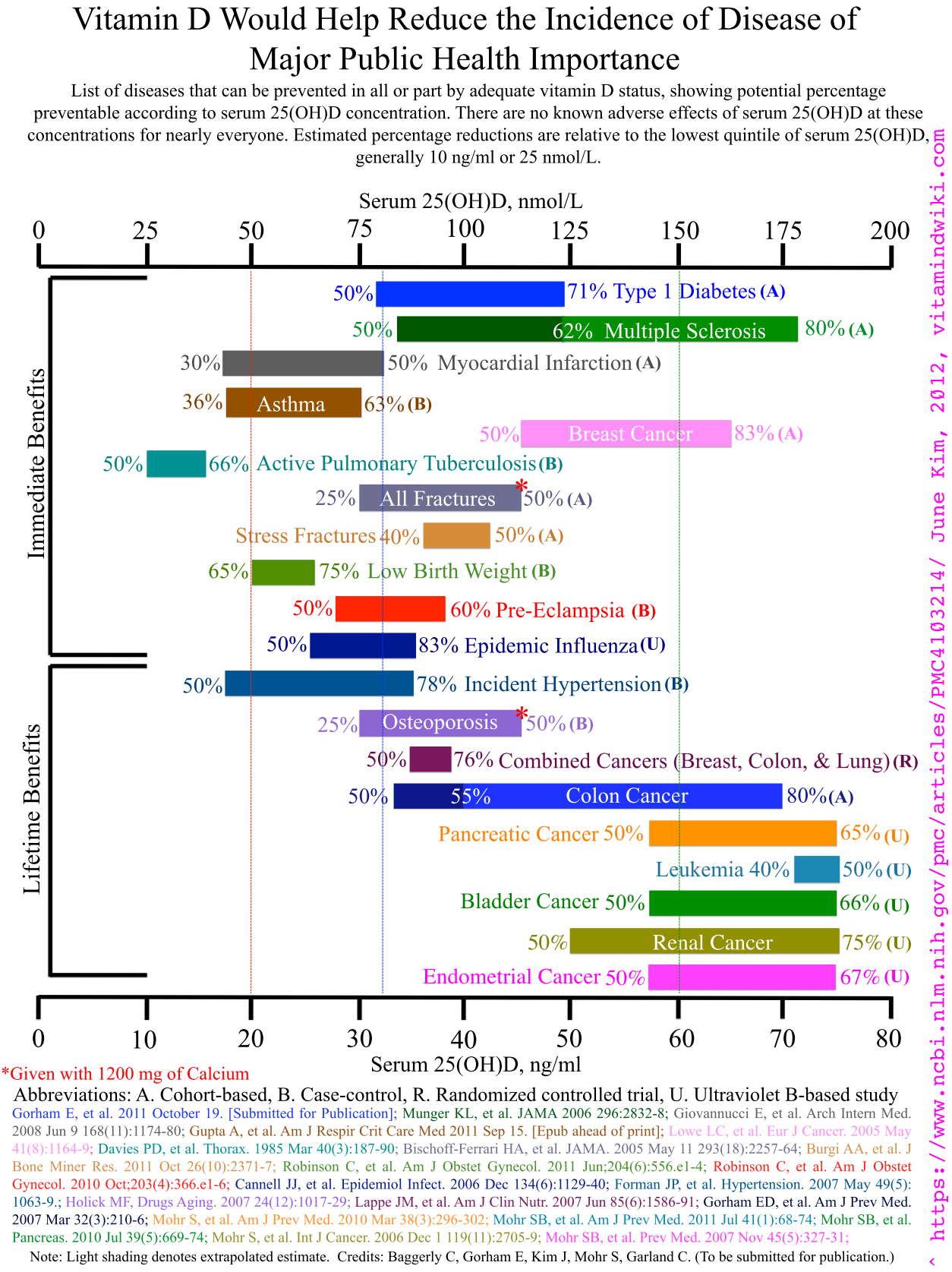
Numerous peer-reviewed journal articles showing adequate vitamin D reduces inflammation AKA sepsis
can be found at:
vitamindwiki.com/Inflammation
vitamindwiki.com/Vitamin+D+reduces+sepsis
www.ncbi.nlm.nih.gov/pmc/articles/PMC4070857/
(Vitamin D and inflammatory diseases, 2014. Google reports 227
citations.)
#03-vit-d-dose
COVID-19 Vitamin D dose recommendations from doctors
See the d3/ page for supplemental intake quantities according to body weight.
Please let me know any published recommendations not listed here, from
doctors or health authorities - for the public in general, and
especially for the public preparing for COVID-19 infection. These
are implicitly for adults, since children seem not to have much trouble
with COVID-19.
- A 2020-03-25 article by John C. Umhau MD (ex-NIH) discusses
studies of vitamin D's ability to protect against respiratory
infections. It includes a link to very widely cited 2007 article
he co-wrote Epidemic Influenza and
Vitamin D - in which up to
5000IU was recommended for adults to achieve the 50ng/ml blood
levels which appear to protect against viral respiratory infection.
www.medpagetoday.com/infectiousdisease/covid19/85596
Both the article and the comments are
interesting - however, I think vitamin D will at best slow down the
progression of the infection, rather than prevent it, and that its real
value will be in reducing or eliminating the overly-aggressive
pro-inflammatory immune response which causes the sepsis.
In the comments, Donna Hurlock MD recommends 4000IU to 5000IU.
There is discussion of magnesium, calcium, vitamin K2 and other
nutrients.
- Version 2 (2020-03-30) of an extensive review article:
Evidence That Vitamin D Supplementation
Could Reduce Risk of Influenza and COVID-19 Infections and Deaths
(2020)
William B. Grant et al.
www.preprints.org/manuscript/202003.0235/v2
To
reduce risk of infection, it is recommended that people at risk of
influenza and/or COVID-19 consider taking 10,000 IU/d of vitamin D3 for a few
weeks to rapidly raise 25(OH)D concentrations, followed by 5000 IU/d. The goal should be to
raise 25(OH)D concentrations above 40–60
ng/ml (100–150 nmol/l). For treatment of people who become
infected with COVID-19, higher
vitamin D3 doses might be useful.
|
The highest recommendation is 10ug,
which is only 400IU.
- Helga M Rhein GP (retired) of Edinburgh wrote comment at the BMJ
site: www.bmj.com/content/368/bmj.m810/rr-9
that one third of the Scottish population is severely vitamin D
deficient. She recommends up to
100ug = 4000IU vitamin D a day and cites a 2011 survey
which reports an average of 37.5 nmol/L. This is an alarmingly
low average of 15ng/ml. They regarded anything above 10ng/ml as
"optimal" and one third of the population had levels below this:
>= 25nmol/L
(10ng/ml) 67%
< 25nmol/L
(10ng/ml) 33%
< 15nmol/L ( 6ng/ml) 12%
Looking at the chart above regarding ARDS, these levels place a
significant proportion of the population at high risk of ARDS when they
contract COVID-19. Likewise looking at the all cause mortality
and burden of disease charts above - only a subset of the population
would have a level which offers them significant protection from a
variety of diseases.
#04-omega-3
Omega 3 PUFAs
The same is true of omega 3 fatty acids.
I believe that if the WHO et al. recommended adults take 2 grams of
fish oil a day and 4000IU vitamin D3, that this - to the extent that
people were willing and able to comply - would significantly reduce
disease severity and death for hundreds of millions of people,
especially those with a Western, indoor, lifestyle.
openheart.bmj.com/content/5/2/e000946
Importance of maintaining a low
omega–6/omega–3 ratio for reducing inflammation (2018)
A
systematic review of 26 randomised controlled trials (RCTs) concluded,
‘Dietary omega-3 fatty acids are associated with plasma biomarker
levels, reflecting lower levels of inflammation and endothelial
activation in cardiovascular disease and other chronic and acute
diseases, including chronic renal disease, sepsis and acute
pancreatitis’.
Indeed, supplementing with fish oil is known to inhibit inflammatory
cytokines such as TNF-alpha and IL-1 beta and
proinflammatory/proaggregatory eicosanoids such as thromboxane-2 and
prostaglandin E2.
|
(2017) N-3 PUFAs induce inflammatory
tolerance by formation of KEAP1-containing SQSTM1/p62-bodies and
activation of NFE2L2
www.tandfonline.com/doi/full/10.1080/15548627.2017.1345411
#05-zinc
Zinc
It may be best to recommend zinc
supplements, since Zn++ in the cytoplasm inhibits viral RNA synthesis -
including zinc
lozenges to slow the initial infection in the throat, before it gets
into the lungs. Zinc is needed for hundreds of enzymes. Please
see what Google scholar returns for zinc
inflammation immune.
Another potential reason for advising people take, for instance, 25mg
zinc per day as chelate is that oral zinc 225mg a day (as best I
understand it) is recommended for patients who do not yet need
breathing support. Paul Marik's
COVID-19 Treatment Strategy - see icu/#Marik-protocol .
#06-vit-c
Vitamin C
I suggest you recommend a substantial but safe level of vitamin C
oral supplementation, since it is known to reduce respiratory
infections and to reduce sepsis when used intravenously. A vet
reports IV vitamin C is routinely used for saving animals from sepsis (medium.com/@anmldoc/i-really-do-not-know-d657e669e749).
She cites Paul Marik MD (www.pilotonline.com/news/health/article_7a3063e5-24cf-56c1-b25c-142731604196.html)
who uses IV vitamin C and hyrdocortisone with success against sepsis in
humans.
Paul Marik's COVID-19 Treatment
Strategy - see icu/#Marik-protocol
- recommends 500mg oral vitamin C 2 or 3 times a day for patients who
do not require breathing support, and for those in ICU, intravenous
vitamin C 3 grams every 6 hours. From (2017) Vitamin C and Immune Function :
Vitamin
C deficiency results in impaired immunity and higher susceptibility to
infections. In turn, infections significantly impact on vitamin C
levels due to enhanced inflammation and metabolic requirements.
Furthermore, supplementation with vitamin C appears to be able to both
prevent and treat respiratory and systemic infections.
Prophylactic
prevention of infection requires dietary vitamin C intakes that provide
at least adequate, if not saturating plasma levels (i.e., 100–200
mg/day), which optimize cell and tissue levels.
In
contrast, treatment of established infections requires significantly
higher (gram) doses of the vitamin to compensate for the increased
inflammatory response and metabolic demand.
|
Soon, hundreds of millions of people with COVID-19 breathing
difficulties will be at home, unable to access care in hospitals or
doctors' clinics. Should uninfected people be advised to take
250mg vitamin C a day, and those with fever, sore throats and/or
breathing difficulties (sepsis induced pneumonia) be advised to take
1000mg or more, subject to concerns about diarrhea? (I assume
that for the duration of the illness kidney stones are not a
significant concern: www.ncbi.nlm.nih.gov/pmc/articles/PMC4769668/
)
Intravenous vitamin C 1500mg 3 or 4 times a day (with
hydroxychloroquine, azithromycin and other drugs) is helping COVID-19
patients in New York: nypost.com/2020/03/24/new-york-hospitals-treating-coronavirus-patients-with-vitamin-c/
Dr Andrew G. Weber said:
The
patients who received vitamin C did significantly better than those who
did not get vitamin C. “It helps a tremendous amount, but it is
not highlighted because it’s not a sexy drug.
Vitamin C levels in coronavirus patients drop dramatically when they
suffer sepsis, an inflammatory response that occurs when their bodies
overreact to the infection. It makes all the sense in the world
to try and maintain this level of vitamin C.
|
#07-vit-b1
Vitamin B1 thiamine
(Not to be confused with theanine, as found
in green tea.)
I have not studied thiamine (WP), but a Google
Scholar search
for thiamine inflammation
turns up plenty of articles, such as:
(2014)
The effect of thiamine deficiency on
inflammation, oxidative stress and cellular migration in an
experimental model of sepsis
link.springer.com/article/10.1186/1476-9255-11-11
This begins with numerous references regarding thiamine deficiency and
critically ill patients, neurodegeneration etc.
My reason for including it here is that vitamin B1 is a component of
the
Paul Marik's COVID-19 Treatment
Strategy - see icu/#Marik-protocol ,
though not for patients with mild symptoms. Those with breathing
difficulties, in ICU, are given 200mg thiamine every 12 hours, orally
or intravenously. This seems a lot, considering the RDA is 1.0 to
1.2mg. This search
turns up various relevant articles.
www.ncbi.nlm.nih.gov/pmc/articles/PMC6206928/
(2018) Ascorbic
acid, corticosteroids, and thiamine in sepsis: a review of the biologic
rationale and the present state of clinical evaluation
The ordinary retail B complex tablet my wife Tina and I take every day
has 15mg of vitamin B1. Our multivitamin has 2.2mg. Given the
correlation between low vitamin B1 and sepsis, it seems prudent to take
ordinary vitamin B1 supplements, especially since it is "relatively
nontoxic" www.drugs.com/monograph/thiamine-hydrochloride.html
.
#08-boron
Boron
Two sections below concern:
Since 2018 my wife and I have also been supplementing our cat's
diet with boron, in similar amounts per bodyweight as we take. We
take ~9 to 12 mg a day and he weighs about 1/10th of what we do and has
0.6mg a day. We did this in an attempt to reduce or prevent his gingivitis and associated feline tooth resorption, for which there is on accepted etiological theory: https://wagwalking.com/cat/condition/tooth-resorption
. This has been a complete success - no more than the original
two teeth have crumbled (the vet had to extract them under anesthetic -
what a miserable business) and his gums are better. This is a sample of
1, but it makes sense and we will continue this supplementation.
Please write to me at rw@firstpr.com.au about this. I have no
training or experience in medicine or veterinary science, but I have
researched this in ways not described here. I believe it is safe
and it is our impression that it is highly beneficial.
2020-06-15: I have a box of boron research papers and am keen to
write them up as an annotated bibliography. I don't know when I
will have the time for this. I will do it on the new website.
For now, please start by reading this excellent review article from
2018, which has a lot of links to research on boron's role in the
immune system, especially regarding inflammation.
In this section I want to raise your awareness of boron as an essential nutrient which
could save hundred of millions of people from sepsis-induced illness
and death with COVID-19. Please take a look at a recent review
article:
PMC4712861/
Nothing Boring about Boron
(2015)
the work of long-time US Department of Agriculture boron researcher,
Forrest Nielsen, such as:
www.researchgate.net/publication/254082639_Growing_Evidence_for_Human_Health_Benefits_of_Boron
(2011, cited by 60.)
scholar.google.com/scholar?q=Forrest+Nielsen+boron
and the research cited at: ods.od.nih.gov/factsheets/Boron-HealthProfessional/
.
One
advantage of boron over the other micronutrients mentioned here is that
while supplies of the others could easily be snapped up if everyone
wanted them, there is plenty of boron for the whole population sitting
on supermarket shelves, in the form of laundry borax.
It is a scandal that boron is not officially recognised as an
essential nutrient. Most people turn their noses up at the
thought. The word sounds like "boring" and rhymes with "moron".
They know borax is used in laundry, as a welding flux, as an ant and
cockroach poison and in children's slime. Many people recoil at
the idea of ingesting boron, because they see borax is the active
ingredient of Ant Rid (8.5%
borax). But boron is in many foods, and vitamin D3 is a
widely used rat and mouse poison. (See my second comment at quillette.com/2020/03/22/covid-19-statistical-and-science-update-for-march-22/
.)
The naturally pure mineral borax - sodium tetraborate - is
mined at large scale in Turkey and California, and then refined into
the bright crystals sold in supermarkets. USP boron is used in
nutritional supplements and medication, but it is difficult to obtain
at a retail level.
If a drug company found a patentable compound with boron's health
benefits and safety profile - including especially its ability to
restrain the body's overactive, sepsis-causing, inflammatory response -
then we would all be singing its praises and paying top dollar for it.
Borax, 100mg a day, in water solution, provides 11.36mg boron a day,
and I believe this will significantly reduce the inflammation which is
killing COVID-19 patients. (I have a box of journal
articles on boron, and no time now to write up an annotated
bibliography of boron nutrition.)
Side note on borax regulation in the EU, including the UK:
I have not yet fully researched this,
but as best I can tell, the EU banned borates, including borax for many
purposes including laundry, around 2010. A laundry borax
substitute sodium sesquicarbonate is sold in its place.
Yet according to
http://www.caviarfactory.ro/en/caviar-preservative-borax/ borax is authorised as a food additive E285 for preserving caviar in the EU, but not in the USA. An extensive 2013
report .
Laundry borax is available by the kilogram in most
supermarkets in Australia and the USA. My wife Tina and I use this - plain laundry borax
is plenty pure enough. (The Eti mine in Turkey, which produces 47% of
the world's borax,
specifies its technical grade borax to have no more than 15ppm
Fe: www.etimaden.gov.tr/storage/uploads/2018/01/10-2017-Borax_Deca_Powder.pdf)
We use: www.blants.com.au/product/natural-pure-borax-900g/
.
Our 12mg boron a day greatly improves on the typical 1mg a day in
the average American diet (ods.od.nih.gov/factsheets/Boron-Consumer/
& ods.od.nih.gov/factsheets/Boron-HealthProfessional/),
and is well within the tolerable maximum of 20mg a day (nap.edu/10026/):
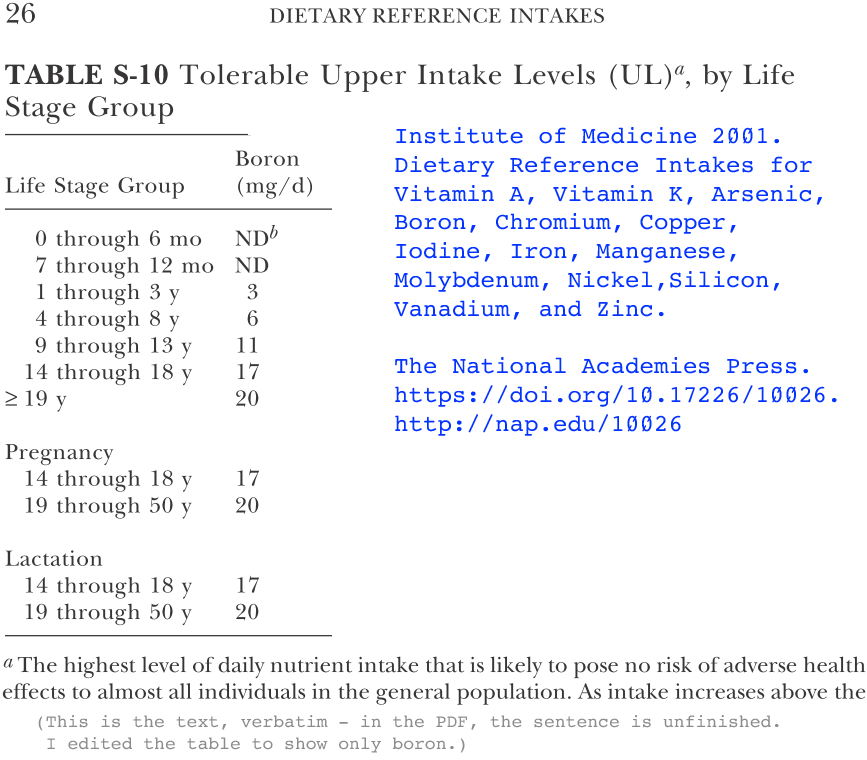
From Nothing Boring about Boron:
A
number of papers have indicated that boron reduces levels of
inflammatory biomarkers. In a recent human trial involving healthy male
volunteers (n = 8), a significant increase in concentrations of plasma
boron occurred 6 hours after supplementation with 11.6 mg of boron,
coupled with significant decreases in
levels of hs-CRP and TNF-α. One week of boron supplementation 10
mg/d resulted in a 20% decrease in the plasma concentration of TNF-α
[tumor necrosis factor alpha], from 12.32 to 9.97 pg/mL, and in
remarkable decreases (approximately 50%) in plasma concentration of hs-CRP [high-sensitivity C-reactive
protein], from 1460 to 795 ng/mL, and of
IL-6, from 1.55 to 0.87
pg/mL.
Is boron adequacy important? Consider that elevated hs-CRP is
associated with an increased risk for breast cancer, obesity and
metabolic syndrome (MetS) in children, atherosclerosis, unstable
angina, insulin resistance, type 2 diabetes, nonalcoholic fatty liver
disease (NAFLD), metastatic prostate cancer, lung cancer, adult
depression, depression in childhood and psychosis in young adult life,
coronary heart disease, and stroke.
|
An assessment of high hs-CRP levels in www.ahajournals.org/doi/10.1161/JAHA.119.012638
is:
| Most
patients with myocardical infarction [heart attack] exhibit elevated
hsCRP levels. Besides identifying populations at high-inflammatory
risk, this study extends the prognostic validity of this biomarker from
trial evidence to real-world healthcare settings. |
Please take a look at vitamindwiki.com/Vitamin+D+and+Boron
which links to articles such as M R Naghii et al. 2011:
Comparative effects of daily and weekly boron supplementation on
plasma steroid hormones and pro-inflammatory cytokines
tahomaclinic.com/Private/Articles1/SHBG/Naghii%202011%20.pdf
10mg boron per day raised Vitamin D levels and reduced
inflammatory cytokine levels.
As
far as I know, 12mg / day boron is safe for most people, but it is
probably best to start with 3mg and increase from there. The two
possible adverse reactions I am aware of are:
- I have read of arthritis and candida sufferers initially having a
Herxheimer reaction (en.wikipedia.org/wiki/Jarisch%E2%80%93Herxheimer_reaction)
due to the death of harmful micro-organisms.
- Several peer-reviewed journal articles by M R Naghii et al. in
Iran report that 10mg or so boron a day causes ultrasound-confirmed
kidney stones to disintegrate and leave the body. This is an
important finding since it implies that some or all classes of kidney
stone only exist due to the boron deficient state of most of the population.
Preliminary Evidence Hints at a
Protective Role for Boron in Urolithiasis (2012)
www.liebertpub.com/doi/10.1089/acm.2011.0865
The full article via Sci-Hub: sci-hub.se/10.1089/acm.2011.0865
Getting rid of kidney stones without surgery or drugs is a good
outcome, but the fragments can be painful and disturb the urethra,
which can cause a UTI (Urinary Tract Infection).
Here I mention this breakup of kidney stones as a potential "adverse
reaction" but it is really a very good reason to supplement with boron,
as long as this response is expected or desired. Please see the
next subsection: #boron-kidney-stones.
3mg boron capsules are readily available, but an alternatiive is to get a heaped
teaspoon of borax (about 8 grams), divide it by 4, and dissolve each
quarter in 2 litres of water. Two 50ml drinks a day provides
11.36 mg boron.
500 grams of borax is enough for 5,000 days at this rate, so a
single borax purchase would help a dozen or so households through the
current crisis. Beware
that in the European Union the sale of borax is apparently banned - and
what is sold as "borax" for laundry use is something else entirely.
#boron-kidney-stones
Update 2022-02-27: Here is what I know about boron and kidney stones. Please read this article:
Mohammad R. Naghii PhD is an Iranian nutrition researcher with a
special interest in boron. He trained, in part, in Sydney in the
1990s. His email address is available at https://journals.plos.org/plosone/article/authors?id=10.1371/journal.pone.0093790
He is not a medical doctor but has advised people and their doctors
about how existing kidney stones can be made to disintegrate by
supplementing with boron - typically in the form of borax.
Here is what I learned after corresponding with him several years ago regarding boron and kidney stones.
As best I understand it, the formation of the solid minerals which form the stones (see the various types and occurrences at: https://www.aafp.org/afp/2019/0415/p490.html ) results from dietary, hormonal and or drug imbalances, especially if the person is not drinking enough water.
Since boron is not a component of these solid materials, it seems that
the role played by supplemental boron, which goes straight into the
bloodstream, and is rapidly excreted in the urine, is to reduce the
inflammatory processes which cause particle of these solid materials to
stick together and form large cacluli AKA stones. (Boron's
biological mechanisms in mammals are not at all understood.) For
the background on low vitamin D and lack of helminths driving these
inflammatory processes, please see: https://vitamindstopscovid.info/06-adv/
Most people have no helminth infections (for good reason) and also have
very low 25-hydroxyvitamin D levels, such as 1/2 to 1/10th of the 25
ng/mL 125 nmol/L their immune system needs. Some people
find that higher levels suppresses their autoimmune diseases - see the
above page.
It is widely believed that vitamin D supplementation increases the risk
of kidney stones. I have not tried to properly research
this. Nguyen et al. 2013 25-Hydroxyvitamin D in the Range of 20 to 100 ng/mL and Incidence of Kidney Stones https://ajph.aphapublications.org/doi/10.2105/AJPH.2013.301368 (40 Google Scholar citations) argues against it. Other articles such as Latavernier and Daudon 2018 Vitamin D, Hypercalciuria and Kidney Stones https://www.mdpi.com/2072-6643/10/3/366 (53 Google Scholar citations) argue that in susceptible individuals, vitamin D supplementation raises the risks of kidney stone formation.
Vitamin K2 is widely - and I assume correctly - believed to reduce the
incidence of calcification of arteries in conditions of excessive
calcium levels. Blood calcium levels are very tightly
regulated. This is the primary function of the best known role of
the three vitamin D compounds - a very low level of 1,25-hydroxyvitamin
D, acting as a hormone, to regulate calcium, phosphate and bone
metabolism.
I don't know to what extent vitamin K2 might affect kidney stone
formation. Nor do I know to what extent it should be supplemented,
considering its potential toxicity and the fact that it is in many
common foods. Nor do I know what form of K2 to take. I
don't take any, and I am 69 kg, and take 0.125 mg 50,000 IU vitamin D3
a week (7143 IU/day),
Please remember that:
- Research on boron and kidney stones is done on people who are
generally highly vitamin D deficient (as is almost everyone in the
absence of proper vitamin D supplementation: https://vitamindstopscovid.info/01-supp/
, who may not be drinking enough water, who may have excessive calcium
intake and who may have a relatively low vitamin K2 intake, inadequate
magnesium and other nutritional imbalances, such as excessive salt.
- Research
on vitamin D supplementation and kidney stones probably involves people
with low boron intakes if one assumes, I think reasonably, that 10 or
so mg of boron intake a day is
healthy and that the typical unsupplemented quantities of 1 or maybe 2
mg a day are deficient. They may also have inadequate water,
magnesium etc. intakes and excessive salt intakes.
In M. R. Naghii's article mentioned above, 10 mg boron a day
(20 mg a day is known to be safe, implicitly for average weight adults)
was shown to cause ultrasound-confirmed kidney stones in all of 14
patients to disintegrate. Borax is 11.36% boron, so 10 mg
is contained in 88 mg of borax, about 1/12 of a gram.
Disintegrating kidney stones is a welcome development for the kidneys,
but can cause pain and disruption or the ureter, potentially leading to
bacterial infections which spread to the bladder as a urinary tract
infection. (UTIs can often be treated with vitamin C, the sugar D
mannose Google Scholar
and/or Hiprex hexamethylenetetramine, rather than with doctor-prescribed antibiotics.)
I understand from my correspondence that M. R Naghii also
recommends the use of vitamin E, zinc, selenium and vitamin B6
pyroxidine. However don't have any information on quantities or
the rationale s for these.
He recommends drinking 2 litres of water a day when trying to encourage
the disintegration of the kidney stones and the safe excretion of the
resulting fragments.
He also recommends people ingest the amino acid L arginine which is readily available as a food supplement. I don't know what quantities he recommends, but this article https://examine.com/supplements/arginine/
suggests that athletes typically ingest 3 to 6 grams prior to workouts
and that 10 grams or more can result in gastrointestinal
problems. He told me that this helps dilate (widen) the ureter
(the pipe which takes urine from the bladder) which enables relatively
large fragments to pass without pain or injury. (I think these
"stones" are not necessarily really hard, but can crumble with moderate
force.)
A Google Scholar search for arginine "ureteral obstruction" turns up some articles which indicate that L arginine had been researched and found useful for reducing ureteral obstructions.
He told me that the diameter of the ureter is normally 5 to 6 mm, but
that with the treatment he has recommended to people, including ~10 mg
boron a day, and an unspecified quantity of L-arginine, that some of
the fragments which have been excreted in the urine, apparently without
injury or much (or any?) pain were "similar to date pits, about 10* 20 mm".
I think it is reasonable to assume that continual ingestion of boron
supplements, such as 6 to 12 mg/day for 70 kg bodyweight, will also
prevent the formation of kidney stones.
The exact type of kidney stones was not mentioned in the 2012 article.
Most kidney stones are made of oxalates. If the action of
inadequately boron is to facilitate excessive inflammatory responses
which bind particles together into stones, with boron supplementation
preventing this and enabling the stones to disintegrate, then it would
be reasonable to assume that adequate boron supplements will reduce the
risk of all types of kidney stones forming.
Ideally I would research this further, but I am an electronic
technician and computer programmer and don't have time to do a proper
job of this. As far as I know this information is valid and will be
useful to many people if wisely considered.
I believe this boron - L arginine treatment and the UTI treatments
mentioned above are good examples of how mainstream medicine fails to
recognise, takes no interest in, or actively denies the importance of
simple nutritional supplements to prevent or treat serious diseases
which are normally assumed to require the concerted attention of
doctors, specialists, and the use of surgery, invasive and potentially
harmful ultrasound (to break up the stones) and/or drugs.
#boron-ra
While searching Google Scholar for "rheumatoid arthritis" and "boron" I found an interesting article from 2012:
Serum boron concentration in rheumatoid arthritis: correlation with disease activity, functional class, and rheumatoid factor
Ziad S. Al-Rawi, Faiq I. Gorial (GS),
Wejdi A. Al-Shammary, Fadhil Muhsin, Ahmed S. Al-Naaimi, Sa’ad Kareem
2012-12 Journal of Experimental and Integrative Medicine 3(1):9-15
researchgate.net/publication/264119179_Serum_boron_....
|
These Iraqi researchers measured boron concentrations in the blood with
an atomic absorption spectrophotometer. (Boron is not one of the
normal blood tests run by pathology labs.) They found the average
boron levels in 107 RA patients was 21.8ng/ml (standard deviation 8.6) while for 214 age- and sex-matched healthy control subjects, the average was about twice this: 43.5ng/ml (SD 9.8). For this difference p < 0.001,
which means that if there really was no underlying relationship, then
based on the random differences between the measured values, such a
deviation would only occur on average once per more than a 1000
trials. They also found some other significant inverse
correlations between boron levels and RA disease severity.
Some notes about this article and the journal it was published in:
The journal
Journal of Experimental and Integrative Medicine
is now defunct. I am not sure that it was ever recognised as a
legitimate open-access journal, so it may have been predatory.
The first two authors seem to have a good publication history in
legitimate journals. I found little or no history for the other
three, but some searches produced numerous matches for similar names,
and I did not scrutinise all the results.
I assume that the article is based on real research and that the
authors choice of journal was mistaken. This article was cited in
2017 by Forrest Nielsen of the US Department of Agriculture , who is
perhaps the most prolific and widely cited boron nutrition researcher:
Historical and recent aspects of boron in human and animal health
I think it is common for researchers from non-English speaking
countries, with limited funds, to choose open access journals with
lower fees than the mainstream, non-predatory, legitimate
journals. There are also quite a few Western, including English
speaking, researchers who publish in predatory journals, presumably not
being wise to what they are doing.
Two later articles, also from Iraq, mention boron and other mineral levels in RA patients: 2015-05 and 2015-07
. In both cases the RA patients' boron levels were also
about half of those of the control subjects. These two are in a
well-known predatory journal: the Pakistan-based, so-called: American Journal of Internal Medicine.
I regard these articles as probably being based on real research, but
not really citable due to the journal they appear in.
Boron supplement capsules and tablets are available from numerous
companies, usually with 3mg boron. This is suitable for taking
two a day, since this gives 6mg a day, and the half-life of boron in
the bloodstream is a little less than a day. An eBay search
for boron and 3mg showed products from obscure companies and major ones
such as Now, Solgar, Life Extension and Solaray. The best deal I
found was 250 3mg capsules for USD$6 or less: swansonvitamins.com .
I have noticed small amounts of boron, such in some Australian supplement tablets containing other compounds for arthritis:
I was pleasantly surprised to see boron in some mass-market (larger
supermarkets all over Australia) multivitamin capsules, from Cenovis: https://cenovis.com.au/?s=boron :
1mg as borax: Men's Multi , Women's Multi , Women's Multi + Energy Boost & Men's Multi + Performance .
3mg as boric acid: 50+ Multi
#09-salt
Salt
Everyone knows that most people consume too much salt. See some
journal article links below #salt concerning
excessive salt consumption driving pro-inflammatory immune responses -
and so sepsis.
Faced with the threat of imminent sepsis, I think many people could be
convinced by consistent medical advice to go easy on salt.
This should go along with the obligatory warnings to reduce or
eliminate smoking and alcohol.
#10-exercise
Exercise
Regular moderate exercise helps build a robust and well-regulated
(against sepsis) immune system. This 2018 article argues against
the view that intense exercise decreases immune competency: pubmed/29713319.
| Epidemiological
evidence indicates that regular physical activity and/or frequent
structured exercise reduces the incidence of many chronic diseases in
older age, including communicable diseases such as viral and bacterial
infections, as well as non-communicable diseases such as cancer and
chronic inflammatory disorders. |
The challenge is to maintain or increase regular exercise in a time of
social distancing and shelter-in-place.
#11-ht-drugs
Potassium supplementation with potassium gluconate solution is
superior to blood pressure medication
Please see the separate page on this: http://aminotheory.com/cv19/kna/
.
#12-blind-spots
Overcoming Western Medicine's blind spots in the next week or two
Conventional Western medicine excels at surgery and other acute
interventions, but has blind-spots regarding nutrition and chronic
diseases.
Since there is no money to be made from the nutrients mentioned
above, their full benefits are known only to some clinicians and
researchers. In the developed world, most people are deficient in
potassium, vitamin D and especially boron. This leads to illness
with aging, diabetes, stroke, CVD, sepsis etc.
As best we know, SARS-CoV-2 will induce debilitating and potentially
deadly sepsis in 5 to 20% of the population in April, May and
June. The terrible toll which is likely to come from this is due,
in large part, to easily corrected nutritional inadequacies.
These they can be solved, since the necessary nutrients are widely
available.
It is not right for me to be making such recommendations to the public
at large, since I have no medical training. I am an electronic
technician, computer programmer and amateur neuroscientist: aminotheory.com/rlsd/briefsumm/
. To the extent that
advice such as the above is valid, it needs to come from clinicians and
health authorities.
#links
COVID-19 and sepsis resources for healthcare professionals
- [#ssc]
Some aspects of the medical establishment are overly-resistant to new
information: emcrit.org/pulmcrit/coronavirus/
. This 2020-02-04 article, by Josh Farkas MD (associate professor of
Pulmonary and Critical Care Medicine at the University of Vermont) is
also critical of some aspects of the current WHO COVID-19
guidelines. It starts with a picture of someone drowning.
The
Surviving Sepsis Campaign is a blight on modern, evidence-based
medicine[2018-ref].
It's been clear for some years that its fundamentals were
flawed (centering around rapid, large-volume fluid
resuscitation).
Rather than adapt guidelines to modern evidence, the campaign recently
doubled down on immediate administration of fluid and antibiotics
within one hour. This provoked widespread protest, including a
petition to retire the Surviving Sepsis Campaign that garnered over
6,000 signatures.[ref]
Whether or not to retire the campaign was openly
debated in the journal CHEST.
Change takes time, meanwhile the Surviving Sepsis Campaign continues to
lumber forward. One consequence of this is that recommendations
in the
one-hour sepsis bundle have started to creep into other
literature. If
30 cc/kg fluid and antibiotics are good for septic shock, then perhaps
they're beneficial for other patients? One example of collateral
damage from these guidelines is their mis-application to viral
pneumonia.
|
- [#marik]
"Marik Protocol" is an informal
name for a series of recommendations regarding critical care patients,
including IV vitamin C and vitamin B1. Please see icu/#Marik-protocol .
- Kristina E. Rudd et al. 2020: Global,
regional, and national sepsis incidence and mortality, 1990–2017:
analysis for the Global Burden of Disease Study www.thelancet.com/journals/lancet/article/PIIS0140-6736(19)32989-7/fulltext
report that in 2017 there were about 48.9 million deaths from sepsis, representing about 19.7% of
all deaths.
- A 2019 article reporting that rats fed the equivalent of a
Western diet, high in sugar
and saturated fats
(omega 3 fatty acids found in fish and algae are unsaturated) had much
higher levels (estimated from gene expression) of the pro-inflammatory
cytokines TNF
(tumor necrosis factor) and IL-6 (interleukin-6) than rats fed
fiber-rich chow, when injected with a bacterial endotoxin
lipopolysaccharide (LPS) elsewhere described as "the most potent
microbial mediator implicated in the pathogenesis of sepsis and septic
shock". Western diet regulates
immune status and the response to LPS-driven sepsis independent of
diet-associated microbiome www.pnas.org/content/116/9/3688

- [#salt]
High salt (NaCl) and low potassium intakes are common - but
perhaps, in a crisis such as this, some people might be persuaded to moderate their salt intake,
and eat more vegetables and fruits high in potassium. There are
no doubt multiple negative outcomes from this high salt regime.
Researchers with more expertise than I have might be able to construct
an salt lowering strategy for COVID-19 along the following lines:
- (2013) Sodium Chloride
Drives Autoimmune Disease by the Induction of Pathogenic Th17 Cells
PMC3746493
T helper cells 17, which produce interleukin 17. "The Th17 cells
generated under high-salt display a highly pathogenic and stable
phenotype characterized by the up-regulation of the pro-inflammatory
cytokines GM-CSF, TNFα and IL-2."
- (2017) Th17/Regulatory
T Cell Imbalance in Sepsis Patients with Multiple Organ Dysfunction
Syndrome: Attenuated by High-volume Hemofiltration journals.sagepub.com/doi/10.5301/ijao.5000625
"The level of Th17/Treg imbalance in sepsis is related to the
occurrence and prognosis of multiple organ dysfunction."
- (2019) Where there is sodium
there may be sepsis www.ncbi.nlm.nih.gov/pmc/articles/PMC6735289/
"Although sepsis patients with hypernatremia face a greater mortality
rate, there is a lack of studies examining a potential association
between hypernatremia and sepsis."
COVID-19 and sepsis links:
- Dr Roger Seheult's
extraordinary Coronavirus Pandemic
video updates on YouTube: www.youtube.com/user/MEDCRAMvideos/videos
These are for clinicians, researchers and well-informed lay
people. References are in the text under the video. I
learned a lot from these videos, including about the
deadly use of aspirin in the Spanish Flu.
- Update 42:
Early and late antibodies (immunoglobulins). Rhesus monkey research
showing viral shedding peaked 3 days after infection, where the virus
was in the body, the development of immunity (antibodies) and how this
prevented the monkeys from being re-infected
a
second time. 28 days after infection, no viruses could be
detected and chest X-rays were normal. Progress on antibody
tests. RT-PCR tests are only about 60 to 70% sensitivity, at
least in some countries - for instance, in South Korean the tests may
be better. (13:24 he pronounces his surname like "shwelt" - his great
uncle was
a physician too.)
- Dr Emily Landon
(University of Chicago) speaking of the necessity of extreme Shelter in Place arrangements to
quell the spread of the virus: www.youtube.com/watch?v=kHUuWq6y8F0
(transcript).
- 2020-02-21 report from an ICU
doctor in New Orleans
on the large numbers of patients with extremely serious symptoms,
including those who are in their 40s and have no known pre-existing
conditions: www.propublica.org/article/a-medical-worker-describes--terrifying-lung-failure-from-covid19-even-in-his-young-patients
These symptoms leading to respiratory distress and death are due to
excessive inflammatory response. To what extent are these people
taking aspirin, ibuprofen or whatever in the early stages of their
disease? To what extent are they deficient in vitamin D, omega 3
fatty acids, boron, vitamin C? Most people are deficient in all
these nutrients and more.
| Instead
of temporarily overreacting, people are hesitating,
preparing less and taking fewer
precautions than the knots in their stomachs say they should – beset by self-doubt that maybe they’re
wrong and fear of embarrassment that maybe others will mock them.
Perhaps the most challenging job public health officials face right now
is helping us bear these feelings and ambivalences – and, of course,
bearing their own. |
To the index page of this site: ../
Contact details and copyright information: ../contact/
© 2020 Robin Whittle Daylesford, Victoria, Australia